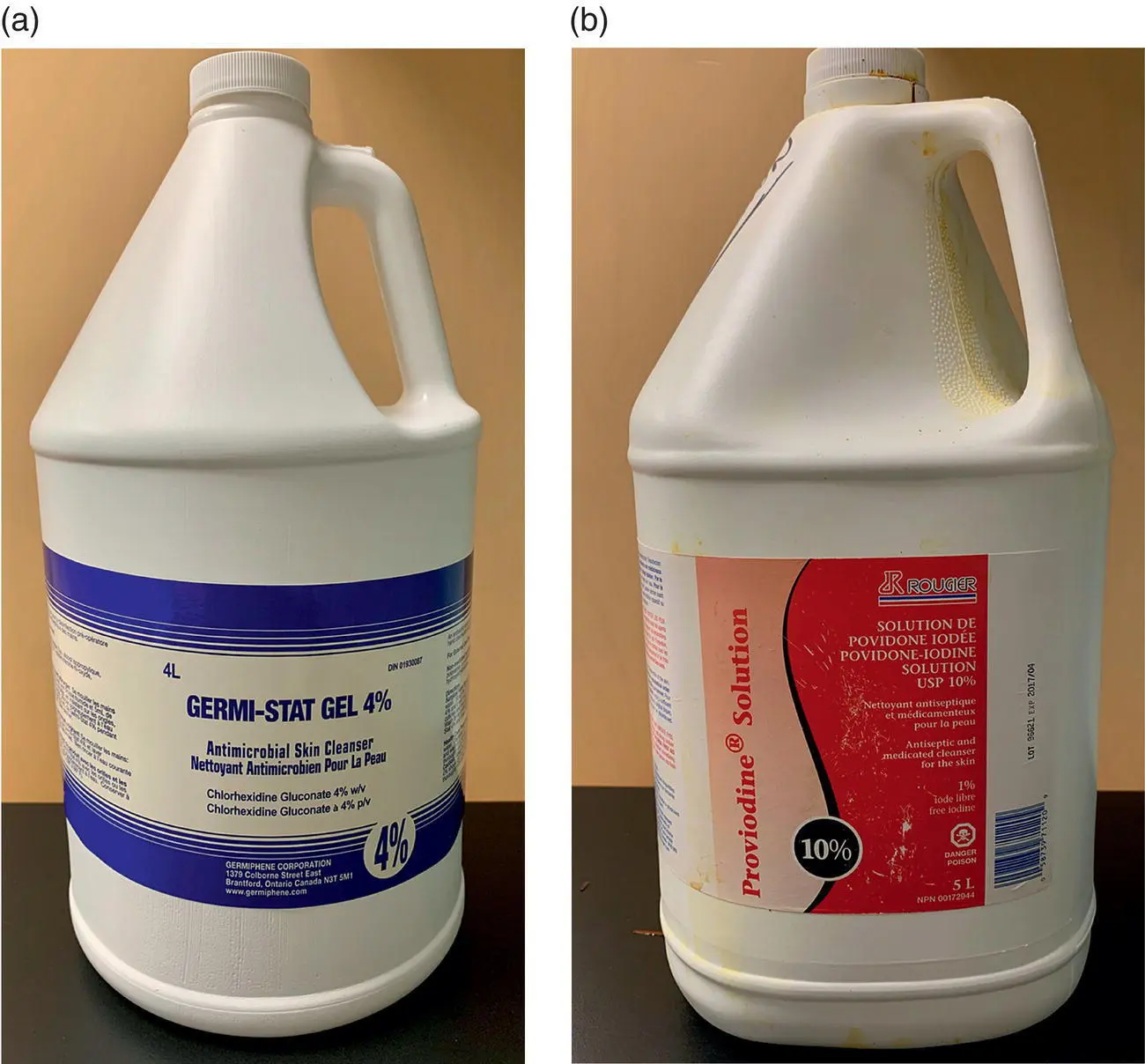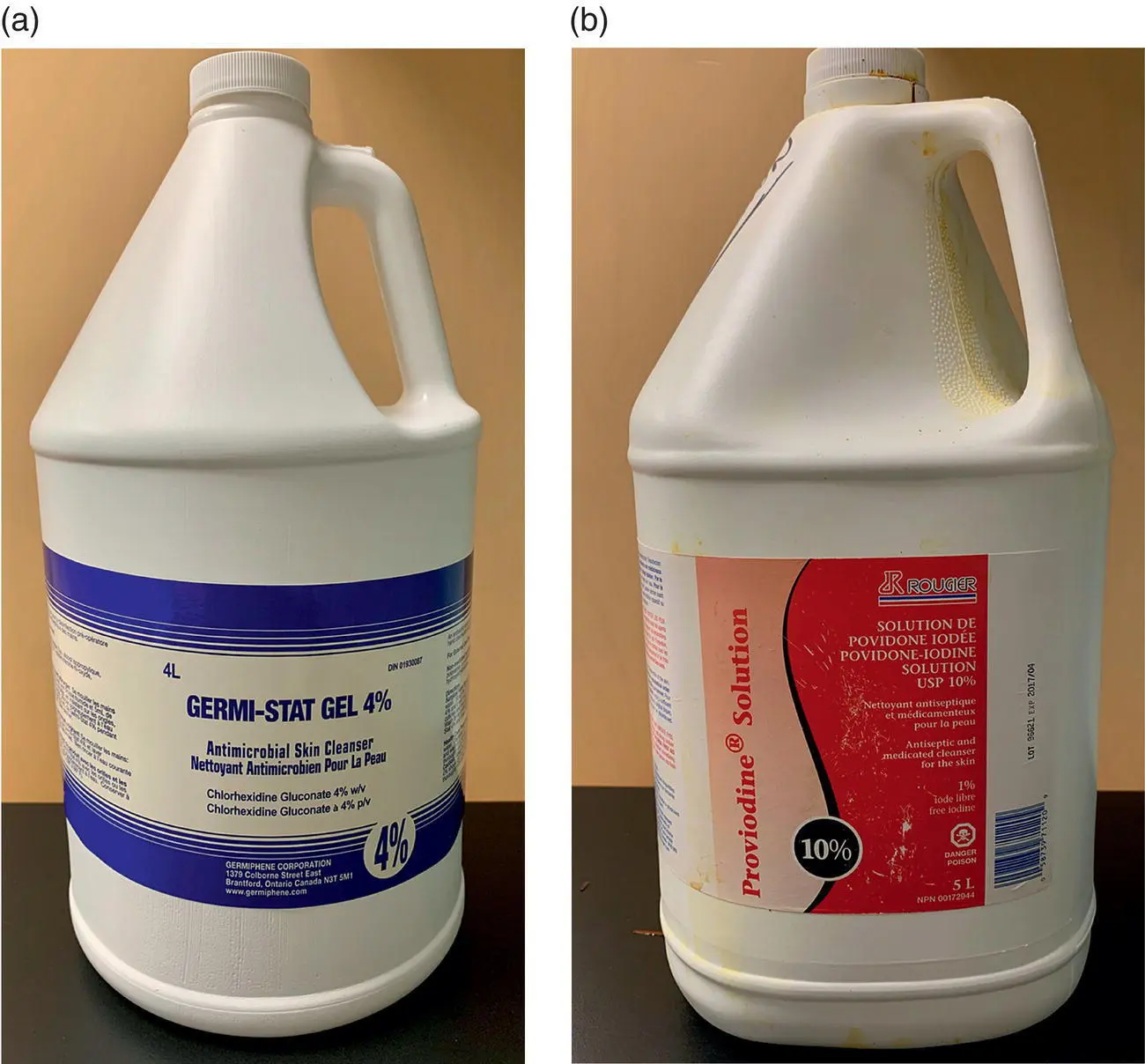
Figure 2.4 (a)Chlorhexidine gluconate 4% soap solution. (b)Povidone‐iodine 10% solution, with 1% free iodine.
As the majority of bacteria identified in contamination of surgical sites with and without SSIs arise from the microbiome of humans and animals within the OR, it is no surprise that an increasing number of OR personnel has been correlated with an increased SSI rate [2]. Reducing traffic in and out of the OR during clean orthopedic procedures may therefore reduce the amount of aerosolized bacterial contaminants and decrease contamination rates [53]. In academic settings, traffic in and out of the OR can anecdotally be higher, therefore in animals with inherent risk factors for SSI, attempts to reduce traffic in the OR are recommended. Both MRSA and MRSP have been identified in small animal hospital environments and among small animal employees [54]. It is possible that hospital personnel carrying MRSA and MRSP may cause direct or indirect transmission to animals [54].
2.4 Surgical Procedure
2.4.1 Surgeon Factors – Hand Hygiene, Glove Perforation, Surgical Technique
Surgeon microbiome contributes to bacterial contamination of surgical sites and therefore surgeon hand and forearm preparation is recommended to reduce the microbial burden prior to donning sterile surgical gowns and gloves.
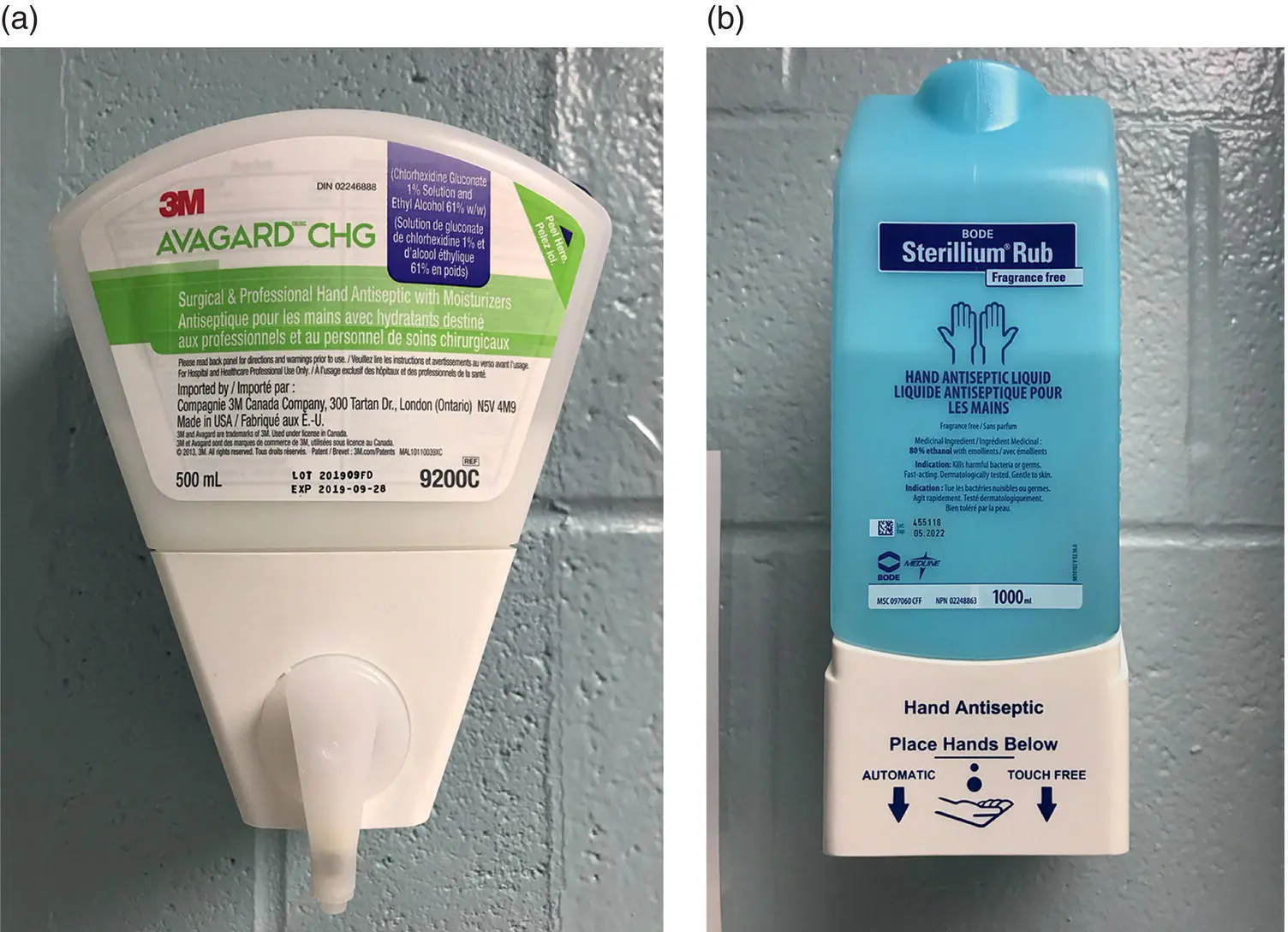
Two main options exist for hand and forearm preparation – surgical scrub versus alcohol‐based rubs (ABRs) ( Figure 2.5). Chlorhexidine and povidone‐iodine are the surgical scrubs most commonly used in veterinary medicine and are equally effective at reducing bacterial colony‐forming units [55]. ABRs, however, provide a faster and more effective sustained reduction in bacteria counts [1, 56]. The use of ABRs, preceded by hand washing using nonmedicated soaps to remove gross debris and oils, results in increased compliance likely due to the reduced time required to apply an ABR than to perform a traditional scrub [57]. A traditional scrub requires a minimum of 3‐minute contact time to be effective, whereas ABRs may be applied in under 2 minutes [58]. A traditional scrub is not required for the first case of the day prior to use of ABRs, as has been previously recommended. Use of ABRs as sole hand and forearm preparation is appropriate as prescrubbing with disinfecting soaps may decrease the effect of ABRs [59, 60]. ABRs are now considered superior for presurgical hand asepsis due to their improved dermal tolerance, along with their reduction in water usage, carbon waste, and potential chances for recontamination on sink fixtures compared to standard scrubs [61].
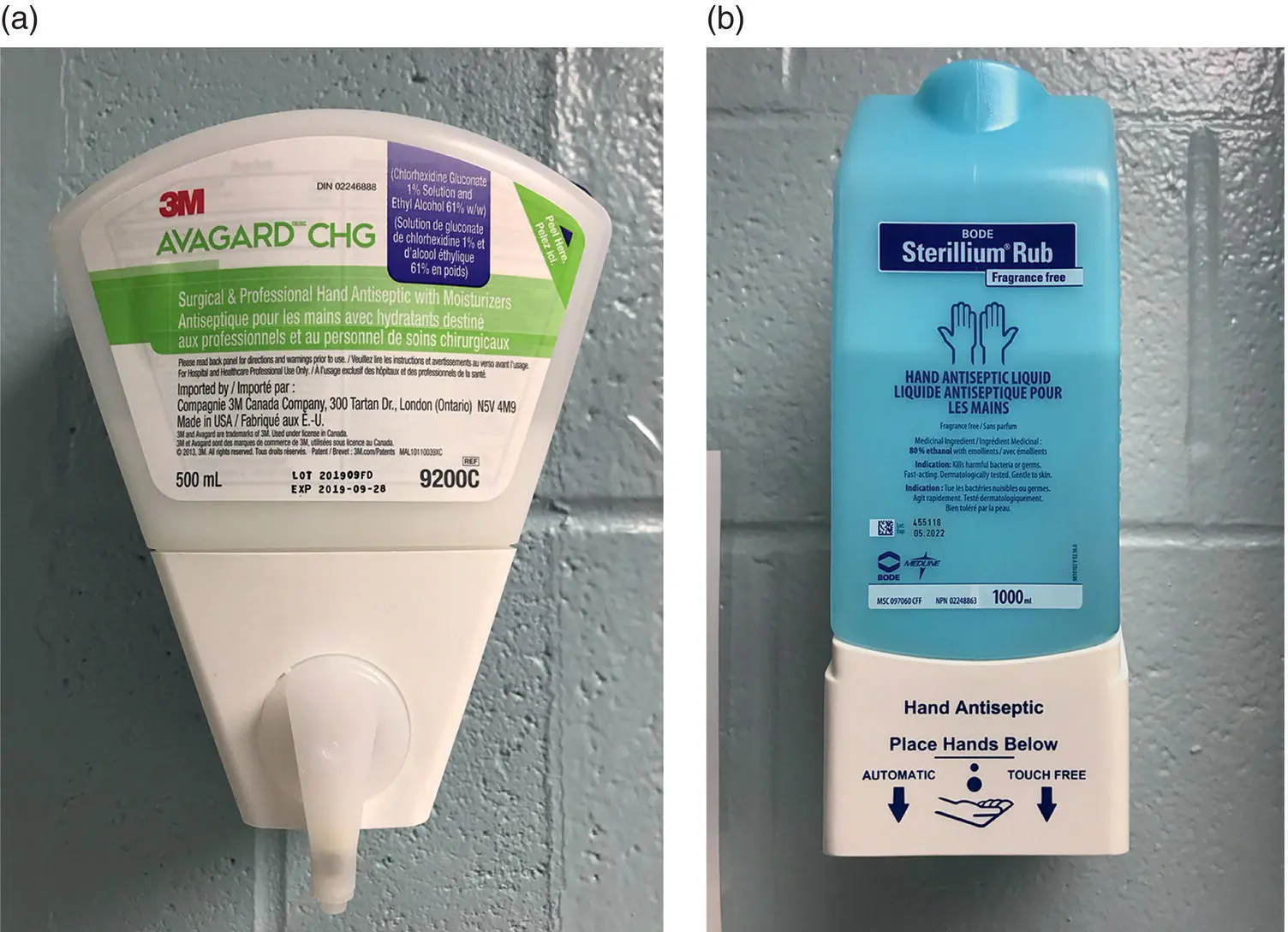
Figure 2.5 (a)Avagard™ chlorhexidine gluconate 1% + ethyl alcohol 61%. (b)Sterillium™ ethyl alcohol 80%.
The incidence of intraoperative contamination reported to occur secondary to glove perforations ranges between 18% and 43% [46, 62, 63]. An increased number of glove perforations are associated with orthopedic surgery, likely in part due to the use of power equipment, screws, pins, and wire [62, 63]. Use of thicker orthopedic gloves was not associated with a reduced rate of glove perforation [63]. However, a hospital‐wide policy change to the use of orthopedic gloves for TPLO surgeries, in addition to other protocol changes, lead to a reduction in SSI rate in one hospital [64]. Identification of glove perforations was poor, but the addition of color indicator undergloves increased the identification rate [62, 63]. The primary surgeon is at highest risk for glove perforation [62, 63].
Evidence exists that SSI rates may differ between surgeons within an institution and may be associated with surgeon experience [14, 27]. Surgeons performing >20 TPLO procedures had reduced SSI rates compared to novice surgeons in one study [27]. While this may not be true in all institutions, two factors that may contribute to a novice surgeon having increased SSI rates include prolonged surgery times and inferior surgical techniques. Excellent surgical technique following Halstead's principles of surgery may aid in reduction of SSI development due to reduced tissue trauma, preservation of blood supply, limited hemorrhage, reduction of dead space, tissue apposition under minimal tension, and adherence to strict aseptic technique [65].
2.4.2 Anesthesia and Surgery Time
Both prolonged anesthesia and surgery times have been associated with increased SSI rates [2, 5, 9, 14, 16, 40, 41]. The risk for SSI has been reported to increase between 0.5% and 4% per minute of anesthesia and 7% per minute of surgery [5, 9, 16]. Theories that lead to this increased SSI rate have included hypotension, hypothermia, and tissue hypoxia but no correlation has been made between these factors [5]. One study that correlated prolonged anesthesia and surgery times with the development of SSI also identified that with prolonged anesthesia and surgery times, more antimicrobial resistance developed [14].
Reducing anesthesia and surgery times requires a concerted effort between members of the surgical team, anesthetists, and diagnostic imaging. Ensuring all equipment is available and all involved personnel are prepared before inducing anesthesia may aid in efficiency and therefore reduce anesthesia and surgery times. In an academic setting where student teaching occurs, it may not be possible to reduce these times, especially when novice surgeons (i.e., surgical interns and residents) are performing portions of the surgical procedure. For animals with known inherent risk factors for SSI, reducing these times may aid in lowering their SSI risk. Introducing surgical checklists ( Figure 2.6) is one way to improve communication between the surgery and anesthesia team and reduce complications that can lead to increased patient morbidity and mortality [66, 67].
Draping of the surgical site ( Figure 2.7) is advised to minimize contamination and use of impervious single‐use disposable drapes is considered best practice [68]. While there are limited studies investigating the use of incise films, noniodonated incise films have been shown to increase bacterial growth beneath the drape, thus increasing the risk for SSI [68]. Despite a lack of evidence for iodinated incise films to reduce the SSI rate, there have been no reports of increased bacterial growth beneath iodinated drapes, which makes an iodinated incise film a superior choice to a noniodinated incise film, if elected for use [30, 68]. When applying incise films, appropriate application without lifting the edges following application is recommended to reduce the risk of bacterial contamination. Implementation of an iodinated incise film, in addition to other protocol changes, lead to the reduction of SSI rate in one hospital following TPLO [64].
As a variety of surgical procedures exist for stabilization of the CCL‐deficient stifle, a wide variety of implants also exist. Implants themselves have been significantly associated with the risk of developing a SSI [1]. When considering extracapsular stabilization techniques, suture types have included nylon fishing line, nylon leader line, ultra high molecular weight polyethylene (UHMWPE), and other multifilamented nonabsorbable suture materials [11, 12, 69]. Nylon has been shown to have reduced bacterial adherence compared to UHMWPE with variation in bacterial colonization of nylon between methods of sterilization [69]. In 1981, multifilamented nonabsorbable suture material used for extracapsular stabilization was reported to have an SSI rate of >21% [11]. In a more recent study using multifilamented UHMWPE, an SSI rate of 1.8% was reported [12]. The discrepancy in SSI rates may be due to improved sterilization and aseptic surgical techniques. Anecdotally, additional protective measures such as applying new sterile gloves prior to handling these materials may reduce the chances of bacterial colonization from skin contamination.
Читать дальше