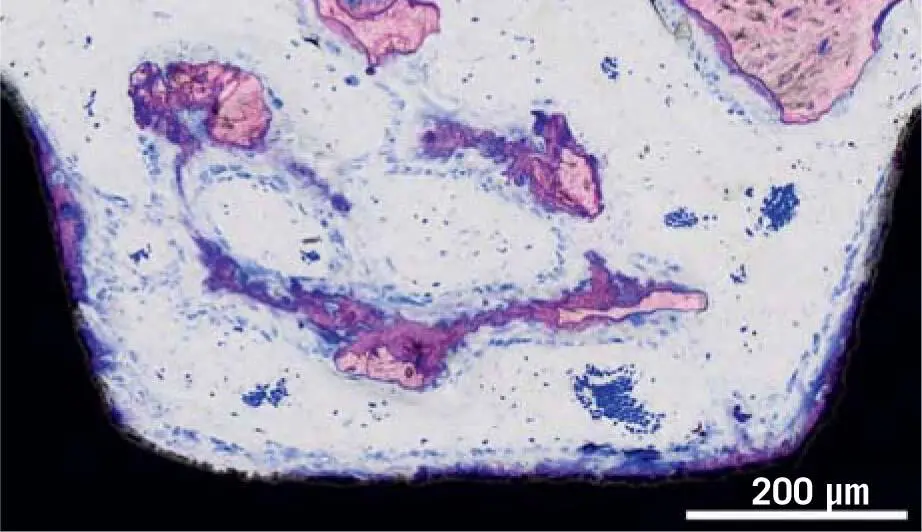
Fig 1-8Dental implant after 10 days of osseointegration in a pig jaw, from a study by Vasak et al. 131Dynamics of early bone formation in the grooves of an implant. New bone (purple) is growing on the implant surface as well as on fragments of old bone that is not resorbed (light pink). Erythrocytes (dark blue) indicate the presence of blood vessels.
1.3.2 Autogenous bone grafts
Even though there is a long tradition of considering autologous bone a gold standard, this claim needs to be specified. Bone transplantation dates back to 1879, when a bone allograft was performed on a 3-year-old boy affected by a huge humeral bone loss. 36Reviews such as the one by Albee in 1930 2are worth reading from an orthopedic perspective. 2From back in the pioneer days to today, the primary intention of bone grafting was to allow the replacement of missing bone in defects of critical size. 103In implant dentistry, starting in the 1980s, bone grafts harvested from the ilium and the mandible were used to reverse alveolar atrophy of the maxilla and mandible. 124At that time, bone regeneration with autografts was also being compared to those filled with bone substitutes.
Preclinical research in pig mandibular defects convincingly showed that, after 2 weeks, almost twice as much new bone formation had occurred in the presence of autologous bone chips compared with bone substitutes; 16,59,60however, this does not necessarily mean that autograft bone chips support bone formation. In the same model, when defects were foiled with corticocancellous blocks particulated by a bone mill, bone scraper, piezosurgery, and bone slurry, bone formation at 1 week was restricted to the borders of the defect, making a total of 3% to 4% of new bone; no bone formation was observed in the center of the defect. 100Bone chips that filled around 20% to 30% of the area were significantly covered by osteoclasts. 100After 2 weeks, bone formation had increased, covering 20% to 30% of the defect area, while within only 1 week, 20% to 40% of the bone chips were resorbed. 100This dynamic phase of graft resorption followed by extensive bone formation continues after 4 and 8 weeks, albeit slowing down overall. The low resorption and the favorable osteogenic potential of autographs is supported by the research of the editor of this book.
1.3.2.1 Bony lid technique
Already in 1987, Khoury reported his clinical data on the bony lid technique for the apical root resection of mandibular molars. 71In another study, he reported his prospective data on this technique in pre-implant and implant surgery. 67The bony lid is a cortical bone plate obtained by the cutting and luxation of parts of the mandible (see Chapter 4). The cortical bony lid can also be split into two halves that are used as a bony sheet (stabilized by micro screws) that holds the bone particles in place, thereby molding the augmentation and implantation site (see Chapter 4). At the re-entry 3 months later, the average width of the alveolar crest after placing the bony lid showed a loss of only 0.5 mm, which is around 7% of the original dimension, suggesting good volume stability.
1.3.2.2 Split bone block (SBB) technique
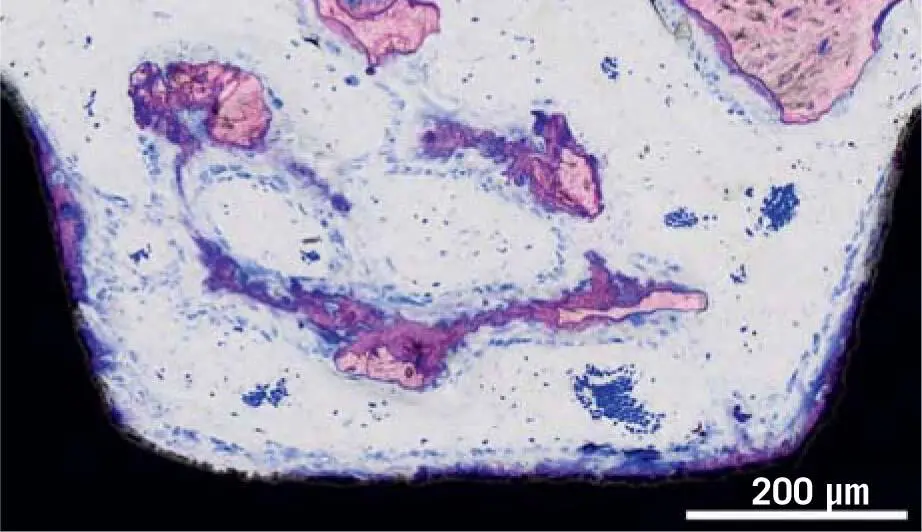
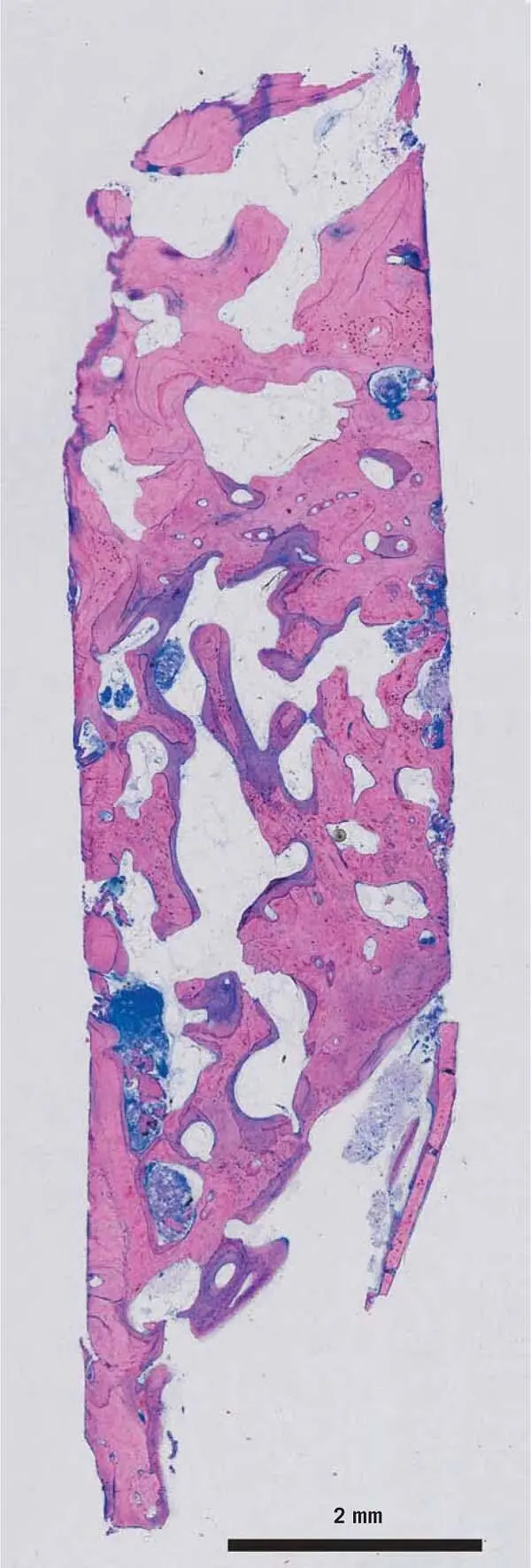
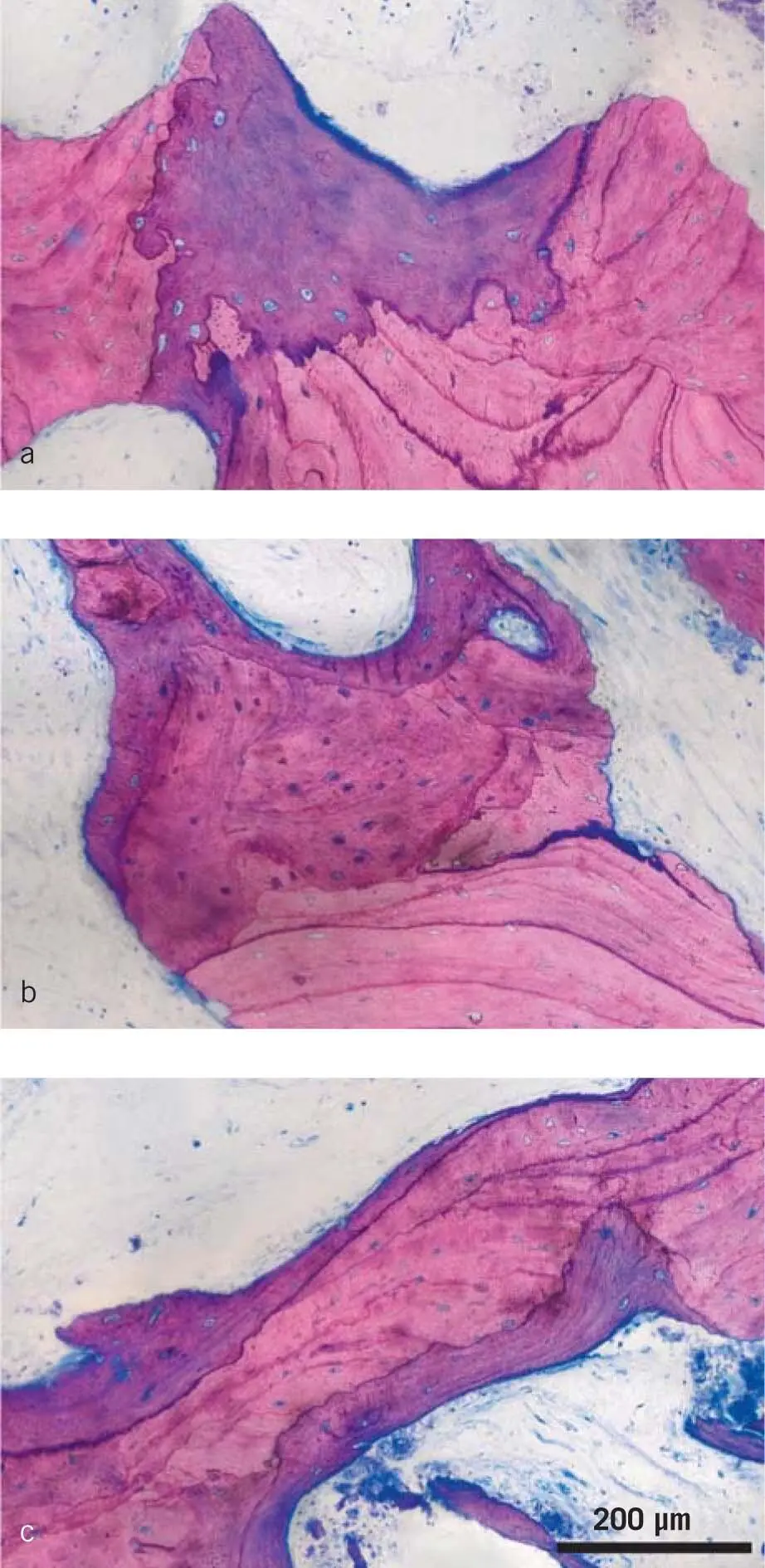
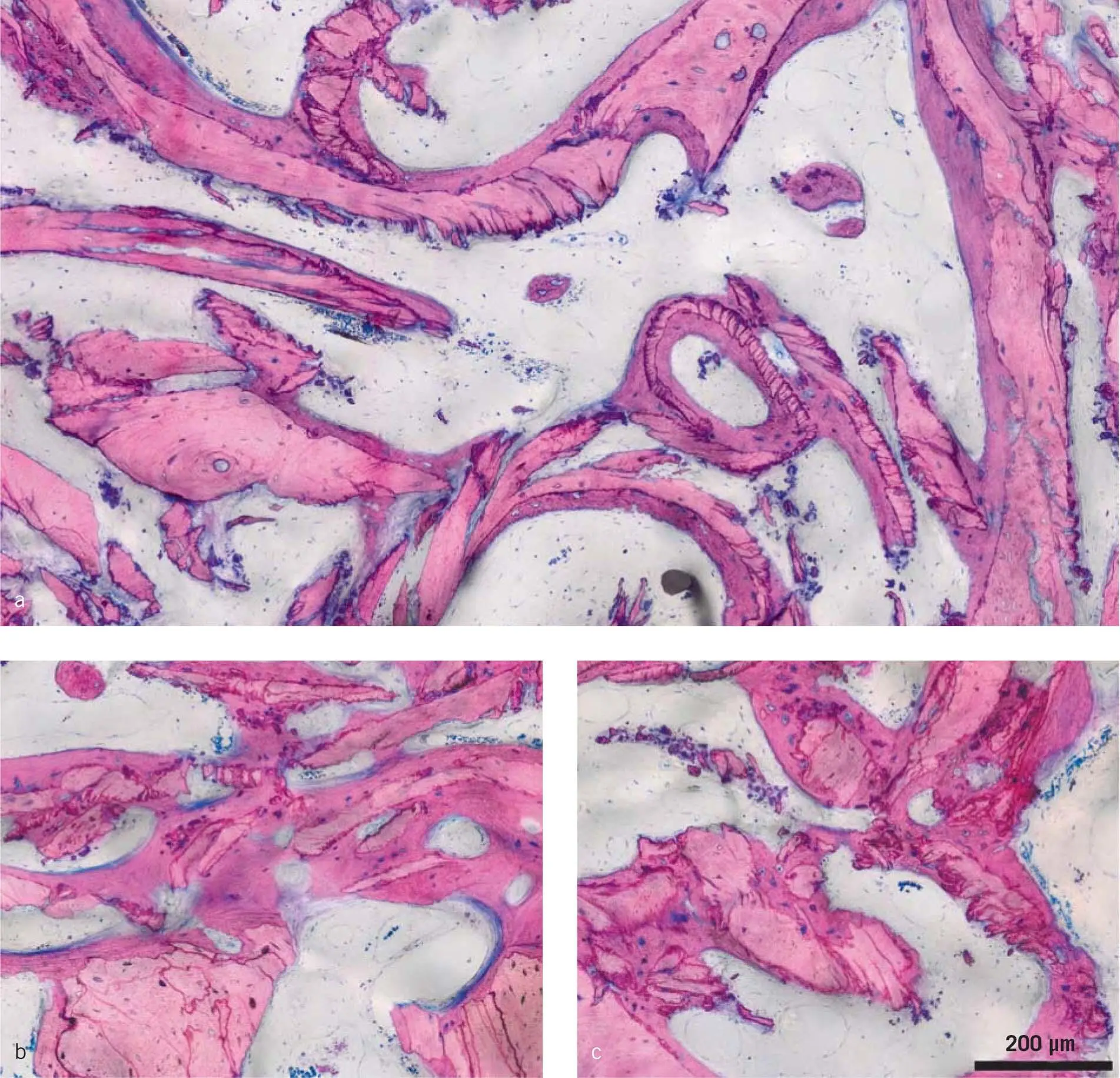
Based on the principles of the bony lid technique, Khoury went on to harvest monocortical bone blocks with the MicroSaw, especially from the retromolar area. 69The bone blocks were longitudinally split and thinned with a bone scraper, gaining at the same time a significant quantity of autogenous bone chips. The thin bone blocks were then stabilized at a distance from the alveolar crest with micro screws to recreate alveolar ridges with sufficient volume and thickness, especially for vertical bone augmentation, and allowing for later implant placement in the prosthetically required position. The space between the thin bone blocks and the remaining alveolar crest was filled with the scraped autogenous bone chips. After 3 months, the implants were inserted into the grafted area 70,72(see Chapter 4). After 3 months of healing, the grafted area was exposed, and the height and width of the grafted area measured. At the same time, bone cores from the planned implant site were removed for histology and histomorphometry using trephine burs ( Fig 1-9). The mean bone resorption was 3.9% in the vertical and 7.2% in the horizontal dimension at the time of implant insertion in the case of 3D vertical augmentation in the posterior maxilla. After 10 years of observation, the mean vertical bone resorption measured on the radiographs was 8.3%. The core biopsies obtained prior to implant placement in the two-stage approach show larger ( Fig 1-10ato c) and smaller ( Fig 1-11ato c) bone chips, which now are integrated into the new bone. Noticeably, the bone surface is not occupied by multinucleated cells, and new bone formation is obvious, making the augmented area ideal for supporting the process of osseointegration of dental implants. This explains the long-term stability of the vertical grafted area with the osseointegrated implants.
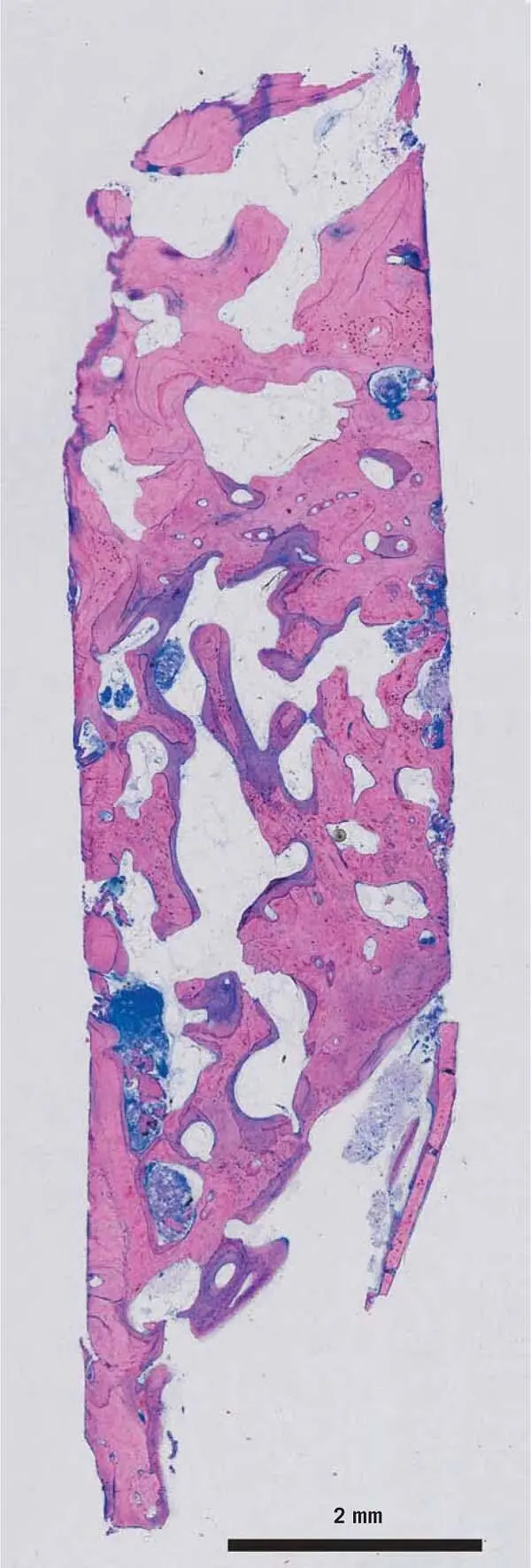
Fig 1-9Biopsy from the split bone block (SBB) technique. The space between the thin bone blocks and the remaining alveolar crest was filled with the scraped autogenous bone chips. After 3 months, the implants were inserted in the grafted area. 70,72After 3 months of healing, bone cores from the planned implant site were removed for histology. In this image, the new bone is stained purple, while the old pristine bone and the transplanted bone chips are pink.
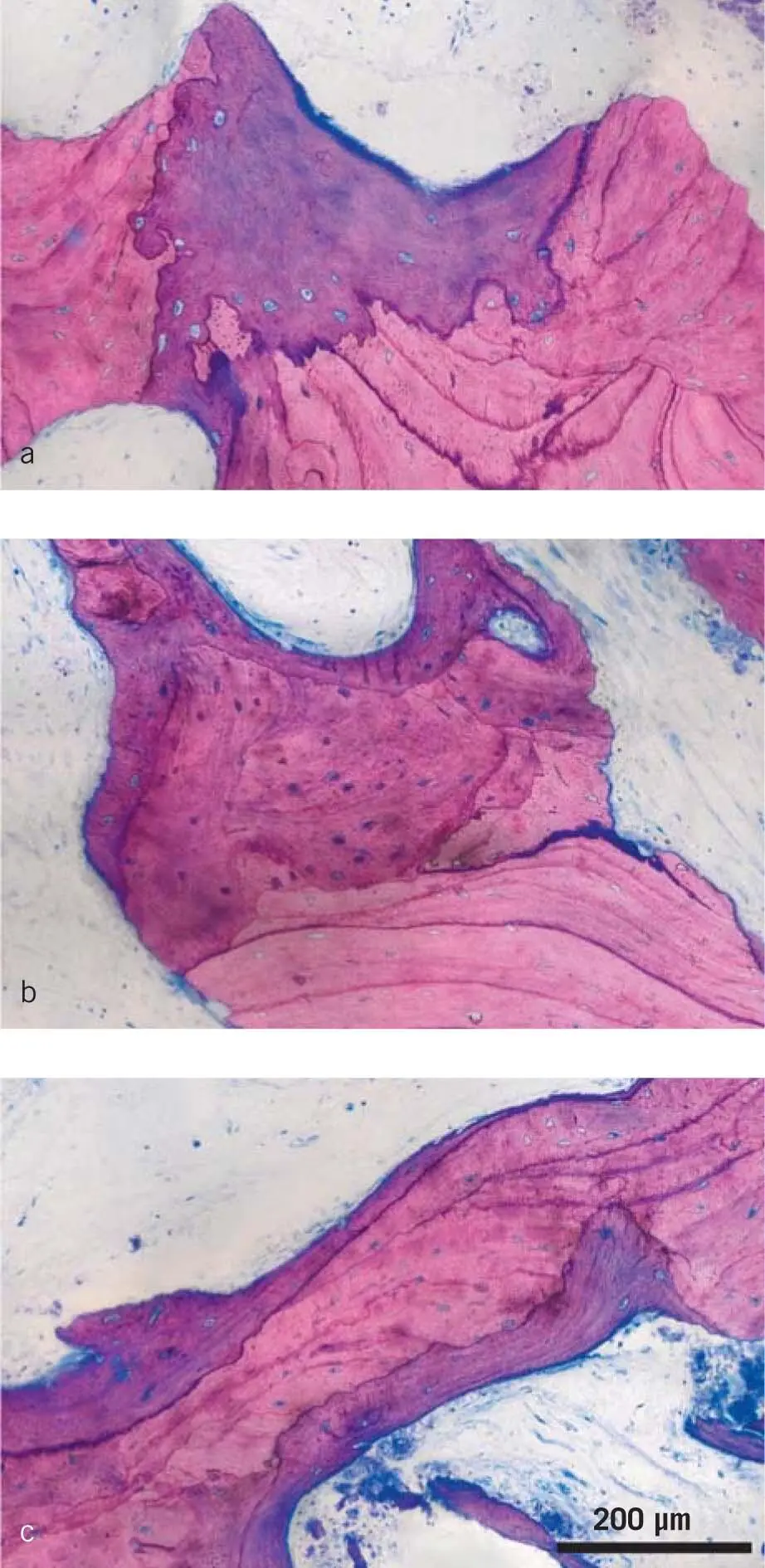
Fig 1-10a to cNew bone formation on the surface of transplanted bone chips. In the SBB technique, scraped autogenous bone chips fill the space between the cortical bone blocks. After 3 months, healing bone cores from the future implant site were removed. The new bone is stained purple, while the transplanted bone chips are pink. Note the cement lines of the transplanted bone, which are signs of previous bone remodeling. Osteocyte lacunae are either empty or filled.
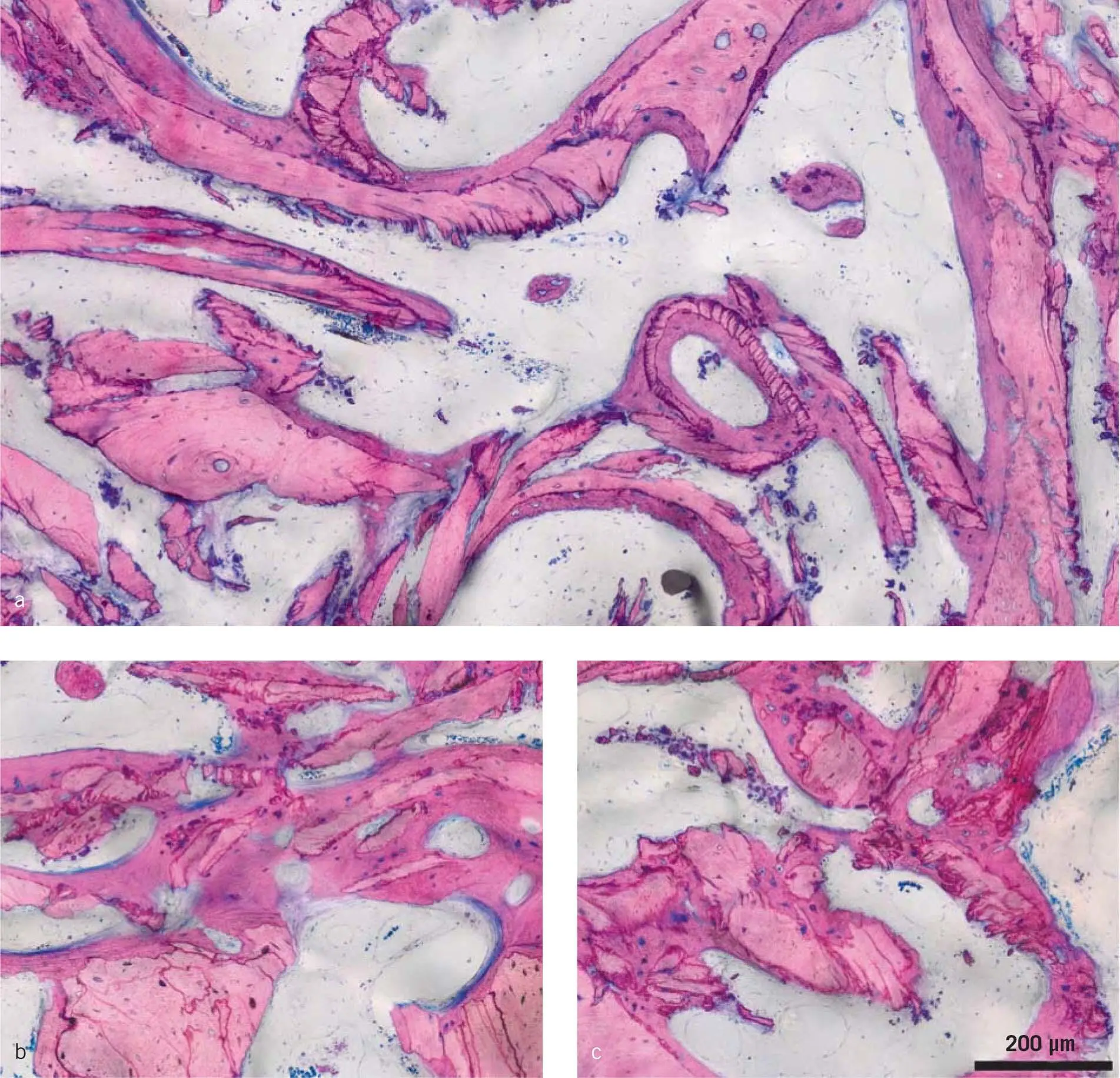
Fig 1-11a to c New bone formation on the surface of transplanted bone chips. Scraped bone chips can have various shapes and may even resemble bone dust. In the SBB technique, after 3 months of healing, the bone chips are covered by new bone and no obvious signs of resorption are visible.
1.3.2.3 Bone core technique
For small augmentations, the bone core technique is recommended. A bone core is harvested using trephine burs of different diameters, but on average a 3.5-mm external and a 2.5-mm internal diameter (see Chapter 4). The bone cores are used together with bone chips to augment the bone immediately after implant placement. This trabecular bone core can be used analogous to the cortical bone plate, providing a small bony sheet for the bone particles, again requiring stabilization with micro screws. After 3 months of healing, the implants and the grafted bone are exposed, and the width of the grafted area measured. Bone cores grafted completely inside the bony contours demonstrated no resorption 3 months postoperatively, while in most cases bone cores grafted partially outside the bony contours showed partial resorption of the bone outside the bony contours. 67Similar to the bony lid technique, at the re-entry 3 months later the average width of the area reconstructed with the trabecular bone core only lost 0.3 mm, which is around 13% of the original dimension, again suggesting good volume stability. What we can learn from this approach is that, in a clinical scenario, the resorption of cortical bone plates as well as trabecular bone cores is low, and that bone chips are well integrated into the newly formed bone after 3 months. 67-69Taken together, autografts in this particular indication allow and may even support the occurrence of natural bone formation originating from the host bone and maybe also from the transplanted autografts. In addition, and interestingly, the augmented volume remains rather stable, with around 7% to 13% resorption after 3 months.
Читать дальше