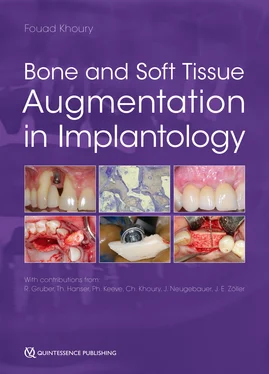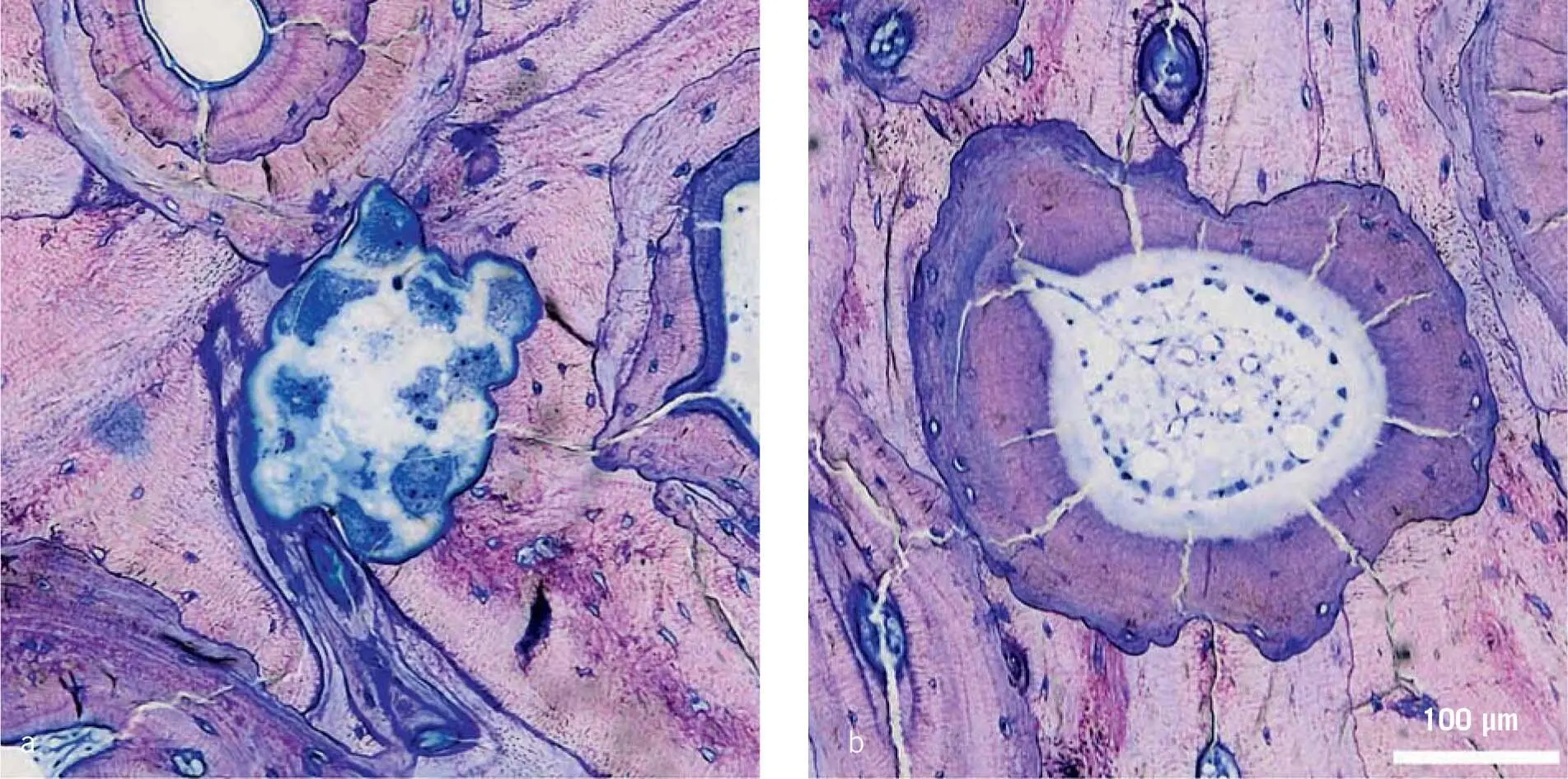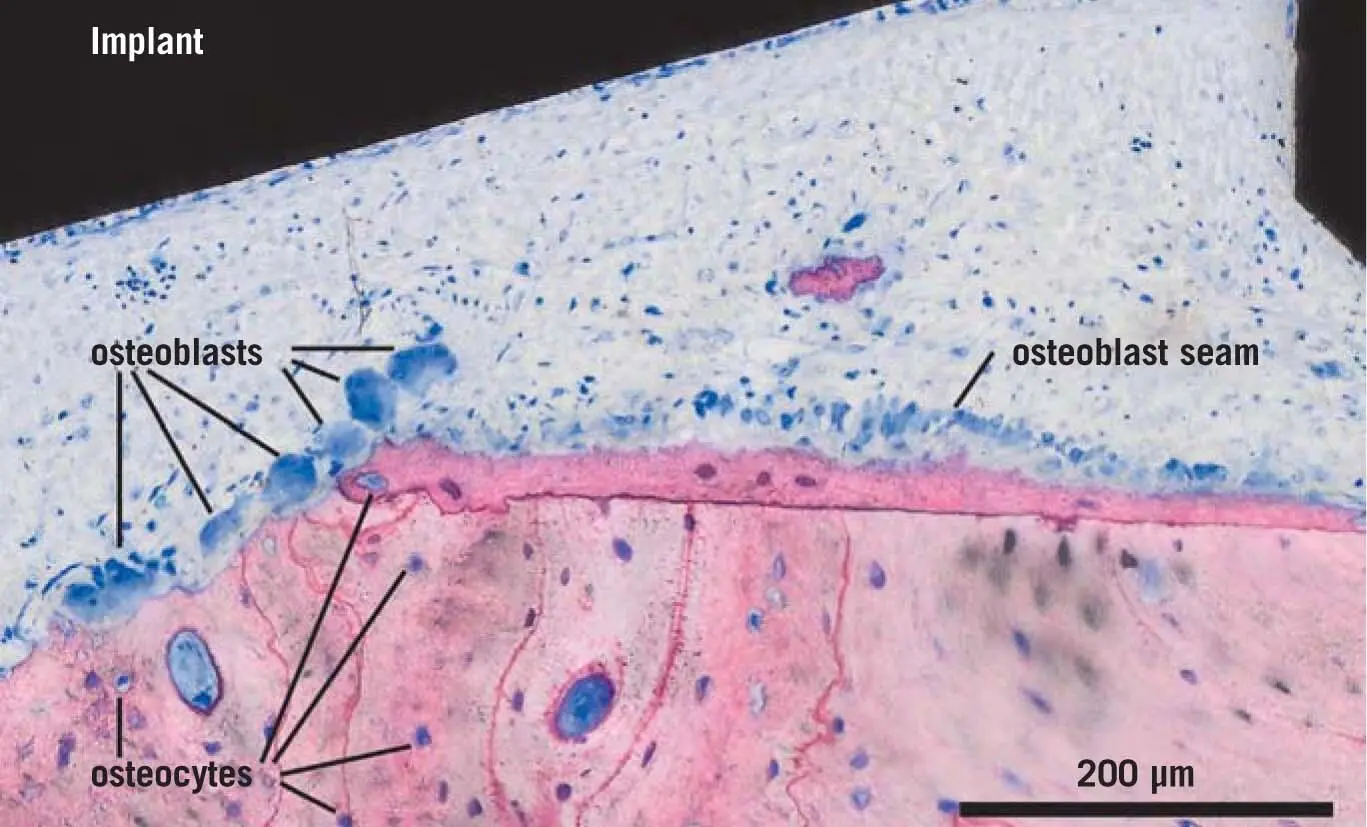
Fig 3-1Osteoclasts (boneresorbing cells), osteoblasts (bone-producing cells), and osteocytes. Osteoclasts are multinucleated cells that are exclusively capable of resorbing bone. In this image, which is a detail taken from Fig 1-7, a group of osteoclasts is resorbing bone next to a seam of osteoblasts, which are producing new bone. An osteoid seam is visible below the osteoblasts. Osteocytes are embedded in the bone. [The image is of pig bone.]
Osteoclasts and osteoblasts are partners in the bone remodeling process – osteoblasts are the bone-building and osteoclasts the bone-resorbing cells ( Fig 1-4aand b). Osteoclasts are therefore specialized in the breakdown of calcified tissue. Hematopoietic cells, particularly those of the monocyte lineage, are the pool of progenitors that have the potential to become osteoclasts; otherwise, they develop into macrophages or dendritic cells with a focus on the immune system. The molecular signature to drive osteoclastogenesis was discovered almost two decades ago, with the introduction of the RANKL-OPG system, the agonist, and the respective antagonist. 23,61,118Mouse models that lack RANKL 73or the respective receptor RANK 38develop severe osteopetrosis, indicated by the lack of a bone-marrow cavity and non-disrupted teeth. In contrast, mice lacking RANKL-OPG acquire a fulminant osteoporosis. 14,111RANKL was considered the ‘bottleneck’ of osteoclastogenesis. Mature osteoclasts are characterized by the sealing zone that sticks the osteoclasts to the mineralized bone surface, surrounding that extensively folded ‘ruffled border,’ where the protons (to lower the pH) and the proteases (to digest the collagen, mainly cathepsin K) are transported into the space facing the naked bone matrix. 121Osteoclasts are considered to be of “great beauty” 18and are not simply “bone eaters” 27as they contribute to bone formation and also interact with the hematopoietic system, including the stem cell niche and adaptive immune cells.
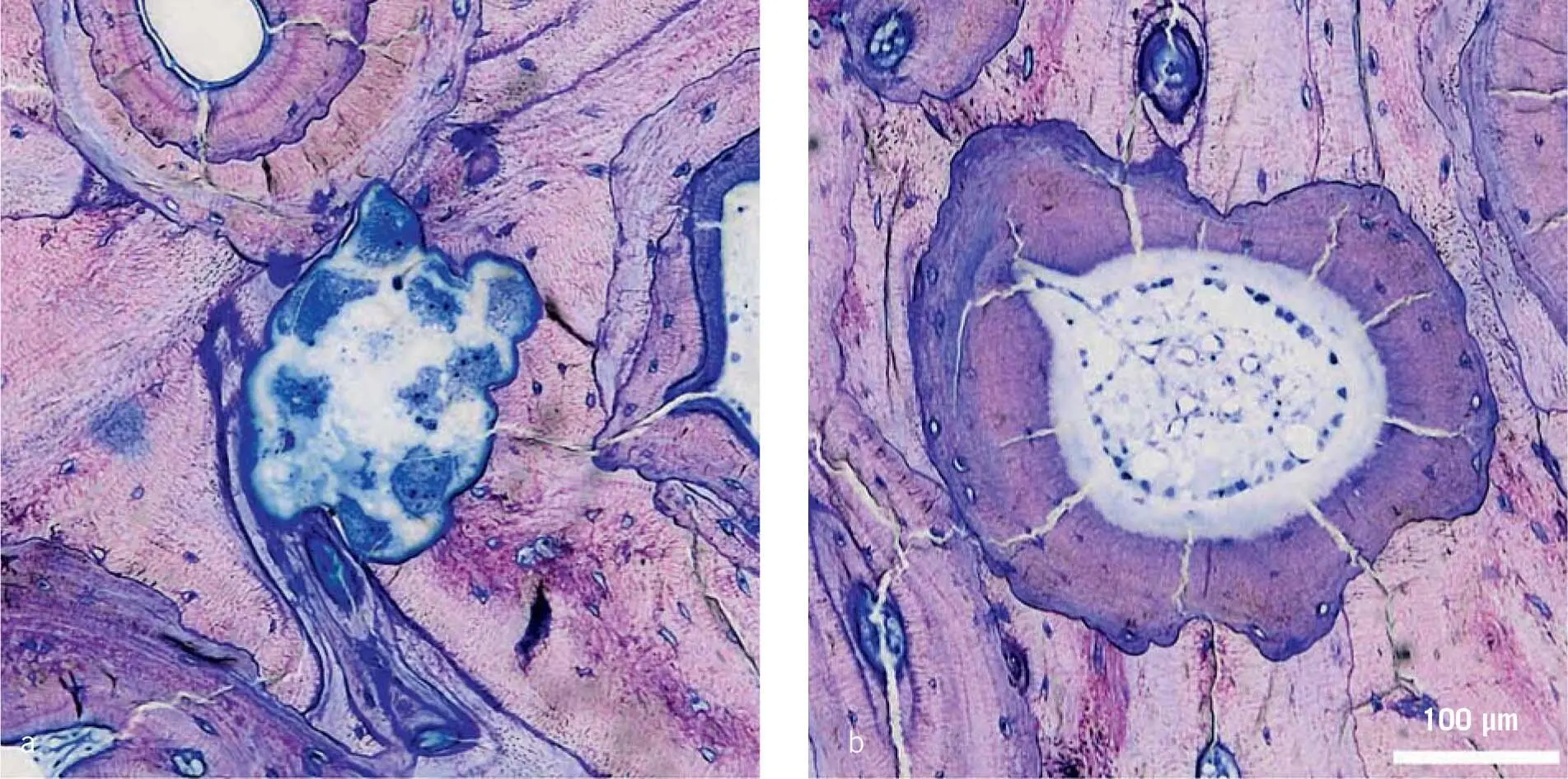
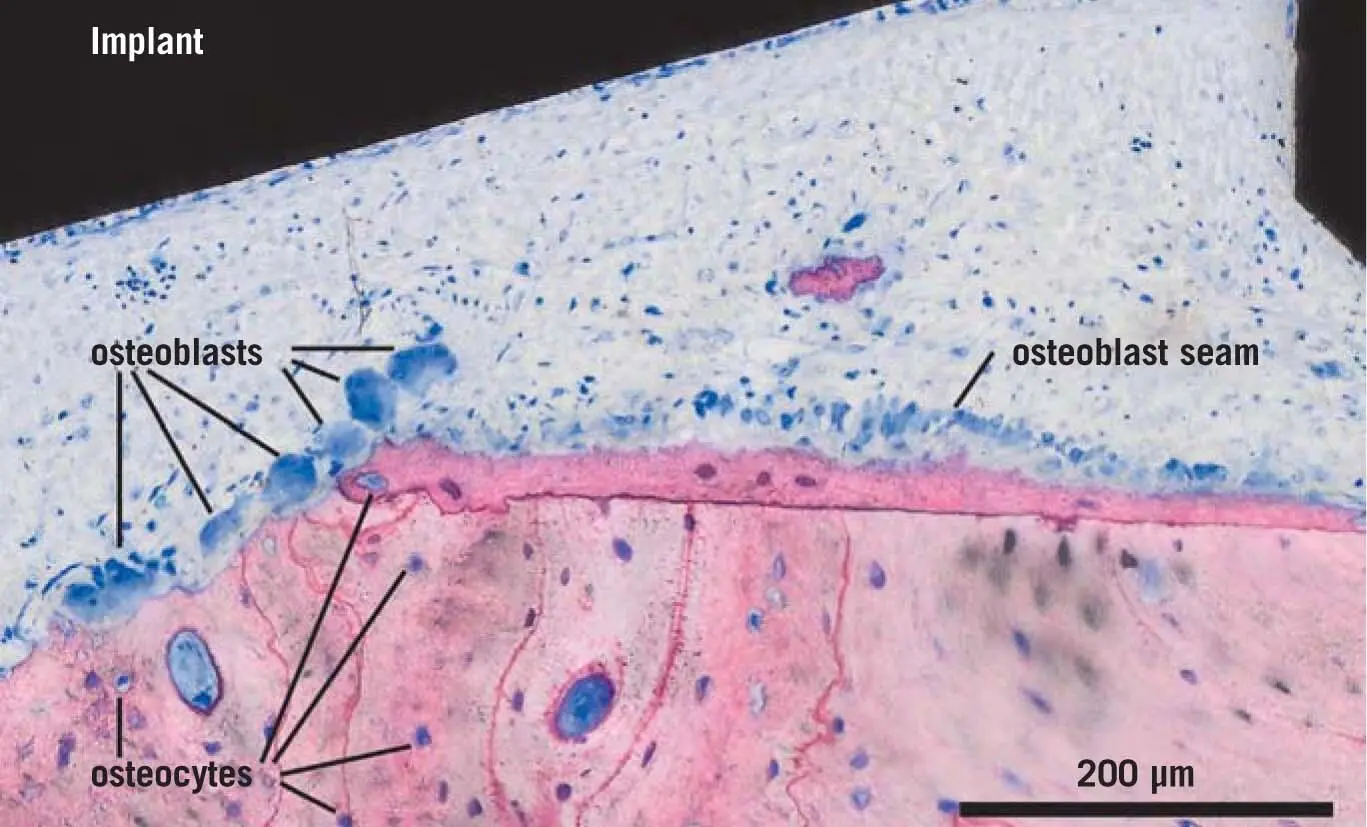
Fig 1-4Creation of osteons by basic multicellular compartments (BMU). The BMU defines the site of bone remodeling. (a) Tunneling of cortical bone by multinucleated osteoclasts. (b) This image is characteristic for the activity of bone forming osteoblasts with an osteoid layer, rebuilding the concentric structure of osteons. [The image is of pig bone.]
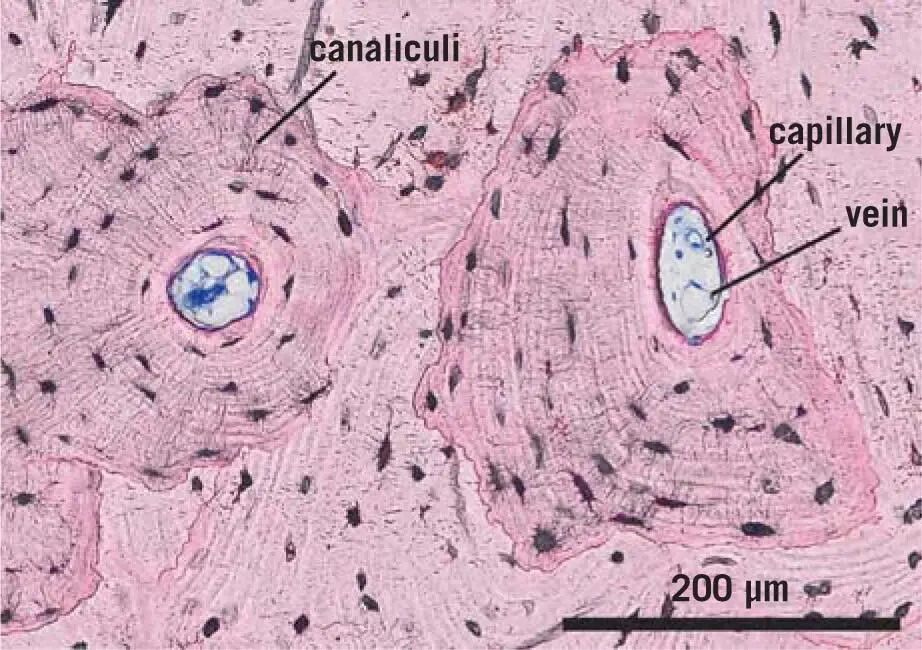
The main physiologic function of osteoclasts is to participate in bone remodeling. Localized in Howship’s lacunae, which represent the active resorption sites on a bone surface, osteoclasts are indicated as multinucleated cells staining positive for tartrate-resistant acid phosphatase. The acidophil cytoplasm contains vacuoles, which indicate resorption. In trabecular bone, osteoclast resorption does not usually exceed 70 µm before a team of osteoblasts fills the space with new bone. Howship’s lacunae are part of the bone remodeling compartment (BRC) canopy. 35In cortical bone, however, the basic multicellular unit (BMU) defines the site of bone remodeling. 106Here, osteoclasts produce a tunnel in the cortical bone that is closed in concentric layers of new bone by the bone-forming osteoblasts with a blood vessel in the center, culminating in the characteristic histologic picture of the osteons in a transversal section ( Fig 1-5). Even though the two remodeling compartments are not identical in structure, there is the common principle of the coupling: when osteoclastic bone resorption has ceased, osteoblastic bone formation is initiated. Preosteoclasts are not only important for bone renewal and remodeling but also for bone revascularization, 137thereby possibly supporting the sprouting of blood vessels at the site of bone regeneration.
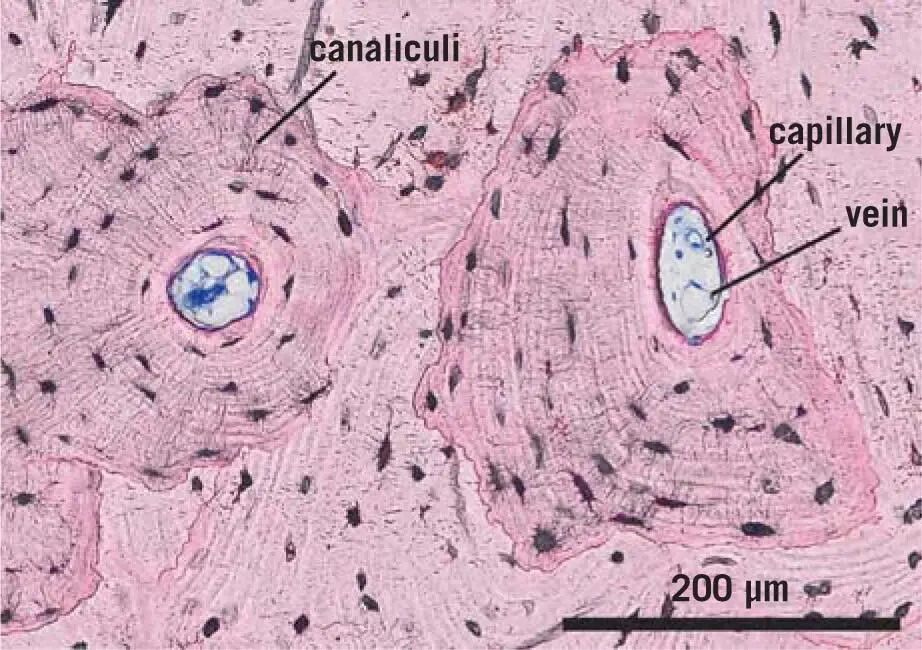
Fig 1-5Osteon with osteocytes being connected via their canaliculi. The osteon is a functional bone unit consisting of a central canal filled with soft tissue, with bone lamellae arranged concentrically around it. They can be found in the substantia compacta of the bone. Osteocytes are interconnected via canaliculi. They are in contact via canaliculi with the lining cells in the central channel. [The image is of human bone, from an implant extraction.]
1.3 Biology of bone regeneration
Bone regeneration is another important aspect of bone biology. Bone regeneration works perfectly in the sense that no scar tissue is formed, which contrasts with the classical skin wound healing in adults, where the defect is left with a matrix rich in collagen but poor in cells. This is summarized in excellent reviews on bone regeneration, particularly in fracture healing 30,42and wound healing. 90,113,143Both events start with the formation of a blood clot, where the coagulation cascade of proteases culminates in the formation of thrombin, which cleaves fibrinogen. The fibrin itself assembles into a transient extracellular matrix, where platelets are activated and form aggregates, together with erythrocytes. Growth factors and other molecules are released, attracting neutrophils into the blood clot to clean the defect site. Macrophages appear later in the blood clot. To make space for the granulation tissue, which is characterized by the sprouting of blood capillaries into the new tissue and the concomitant appearance of fibroblastic cells, fibrinolysis is initiated. The invading cells release activators for plasminogen being stored in the blood clot – it is plasmin that cleaves the fibrin matrix. Interestingly, mouse models lacking fibrinogen allow bone regeneration, 141while those lacking plasminogen show impaired bone regeneration. 64These findings highlight the importance of fibrinolysis over the formation of the fibrin matrix.
Mouse models have also helped in the understanding of the importance of macrophages in bone regeneration, as they were shown to be in wound healing, early on. The depletion of macrophages and the genetic modification of the cells to erase their activity culminate in impaired bone regeneration, including intramembranous ossification, which is the more relevant path in regenerative dentistry compared with the endochondral ossification that is typically observed in fracture healing. 95,135However, the role of macrophages is not restricted to a defect situation. For example, macrophages form a canopy structure over mature osteoblasts during bone remodeling, suggesting that they interact via juxtacrine and a paracrine mechanism that remains to be fully elucidated. 25The clinical implication of this fundamental principle in regenerative dentistry is unclear, but it opens a wide arena for research that may involve biomaterials. Mouse models have also provided evidence that at least a transient inflammation is required for bone regeneration, as, for example, the knockout of TNFα 24,48and COX-2 142caused impaired bone regeneration. Moreover, in bones lacking bone morphogenetic protein 2 (BMP-2), the earliest steps of fracture healing seem to be blocked, 125and it is possible that the local inflammation controls the expression of BMP-2, at least in vitro. 46To what extent macrophages are involved in the inflammation required for bone regeneration has not yet been investigated. Also, here, the clinical relevance of these observations should be interpreted with care. For example, painkillers should not be a great concern in regenerative dentistry as they do not completely block cyclooxygenases and are only used temporarily. 49Bone regeneration is not influenced or jeopardized when inhibitors of TNFα are used, 122as in a situation of chronic inflammation, including rheumatoid arthritis and colitis ulcers. Thus, findings from the extreme situation of a gene knockout or enhanced expression in mouse models should be interpreted carefully in the clinical context.
Читать дальше