The main focus of this chapter, however, is to provide an explanation of autograft consolidation, and to discuss the clinical success of this therapy at the molecular and cellular levels. With an emphasis on bone augmentation, the chapter is intended to supplement the essential information on bone regeneration that has been obtained from histologic and biomechanical analyses.
It is a well-accepted fact that osteoblasts form the bone 40and osteoclasts resorb it. 12,121The osteocytes are important in that they are the masters of regulation in bone remodeling. 33The blood vessels are also important as they serve as a source of renewal and, in particular, as a transport medium for the precursor cells of osteoblasts and osteoclasts; 78,134they are also key in terms of inflammation, and are therefore relevant in pathologic conditions such as inflammatory osteolysis. 55,84In this context, classical questions are addressed in the chapter, such as the evidence that autografts are considered “osteoconductive, osteogenic and osteoinductive,” 98and the possible mechanisms of graft resorption.
1.2 Cells of bone remodeling
Three cell types are characteristic of bone tissue and are responsible for bone formation, maintenance, remodeling, and repair. However, bone biology and bone metabolism comprise a complexity of interactions involving many factors, including growth proteins and many humeral messages and events that are not described in this chapter. One main goal of the chapter is to provide an update on the essential activity of the bone-forming cells (osteoblasts) and the bone-resorbing cells (osteoclasts), with special attention paid to the osteocytes and their important role in the maintenance of bone structure.
These cells originate from pluripotent mesenchymal stem cells through the activation of a series of transcription factors 62partially involving members of the bone morphogenetic protein superfamily. 81,99Osteoblasts are present in layers on the bone surface. In all active bone-formation sites, they are responsible for extracellular matrix production (osteoid) and subsequent mineralization. Osteoblasts are polarized cells with a mineral-facing side through which the matrix is extruded. Once osteoid production stops, some osteoblasts are trapped in the extracellular matrix and differentiate into osteocytes, which are located in the bone lacunae. On the one hand, neurocranial bones, 21including the mandible (except the mandibular condyle) and maxilla as well as part of the clavicle, are formed by membranous ossification. This is a direct ossification without a cartilaginous phase, where differentiated osteoblasts lead to osseous matrix formation through mesodermal and ectomesodermal cellular condensation. On the other hand, the appendicular and axial skeleton follows an endochondral ossification route. A temporary cartilaginous scaffold is produced by chondrocytes, which mature and hypertrophy in a second stage. In a third stage, this cartilaginous matrix becomes mineralized. Finally, a vascularization is established that allows, at first, the arrival of osteoclasts (or chondroclasts), which lead to the resorption of the calcified cartilaginous matrix and, following that, the differentiation of osteoblasts that will replace the cartilaginous scaffold by a bony matrix. This matrix will lead to the formation of the trabecular structure of the long bones. 91
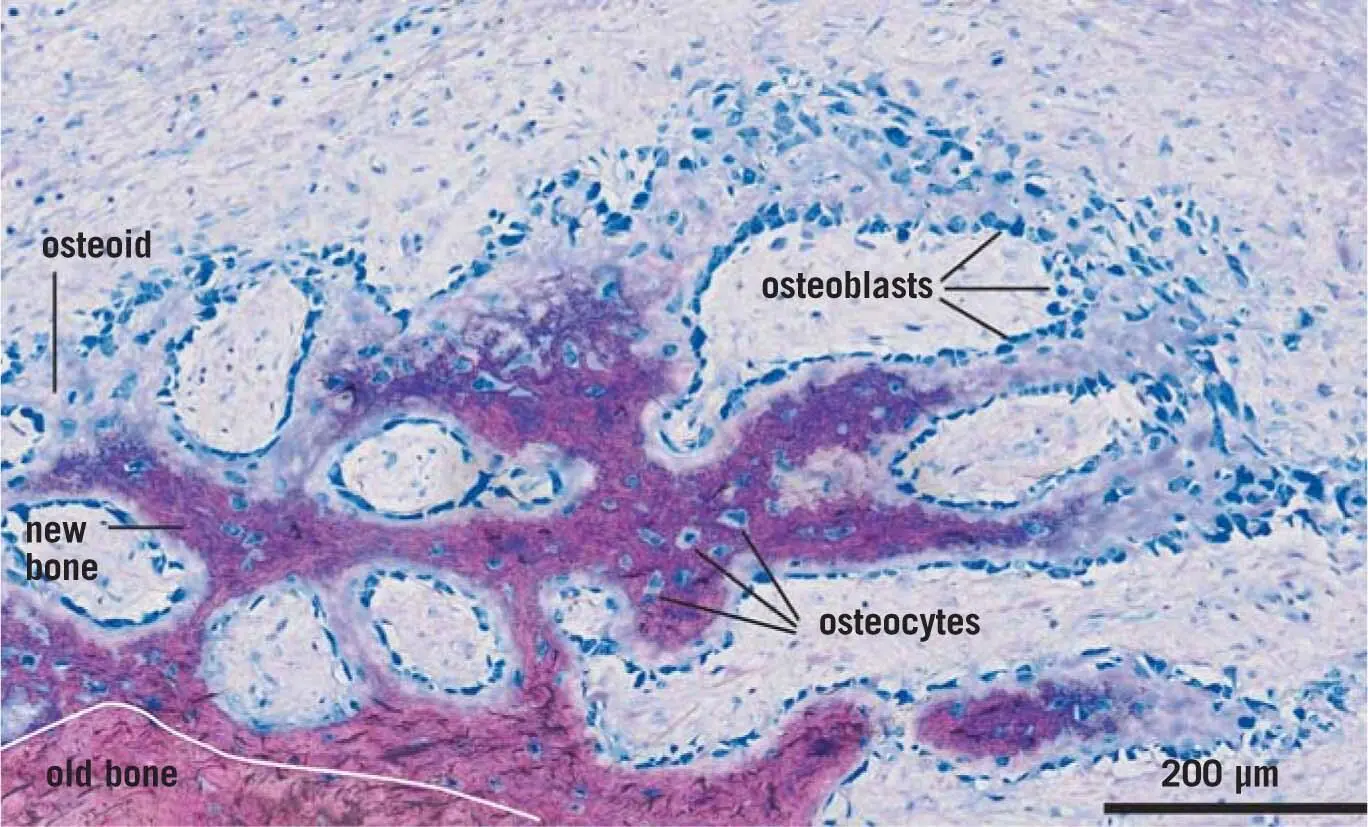
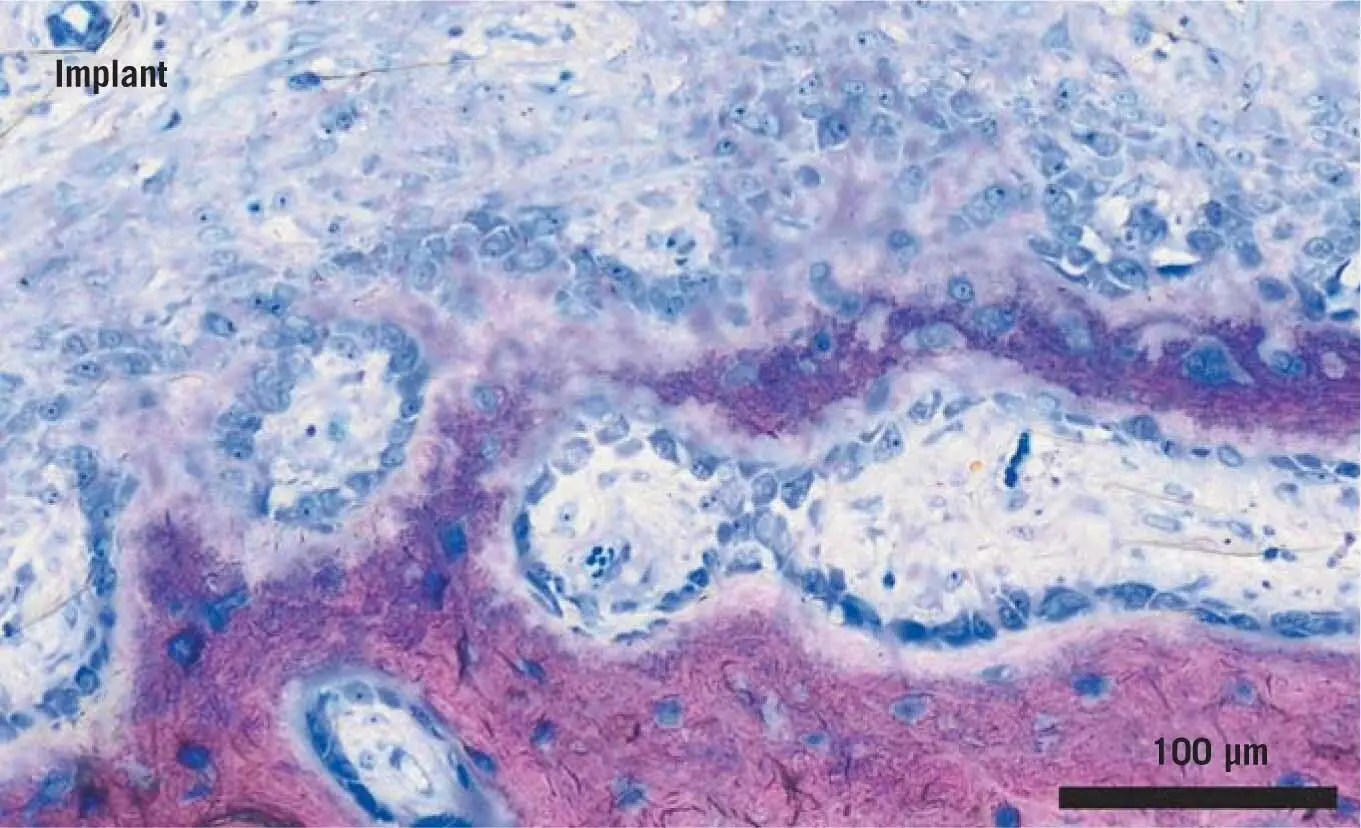
Osteoblasts can produce three types of bone: woven bone, primary parallel-fibered bone, and lamellar bone. The difference between these bone types is related to the orientation of the collagen fibrils: In woven bone, the fibrils are three-dimensionally and randomly distributed due to the rapidity of osteoid deposition and mineralization ( Fig 1-1). Compared with mature lamellar bone, this bone is more elastic and mechanically less consistent due to the low level of mineralization and the lack of a specific orientation of the collagen fibers. In adults, this type of bone is produced during healing processes, and it is the only bone able to grow in the absence of a pre-existing mineralized tissue. Woven bone forms ridges and roots between and around the blood vessels ( Fig 1-2). Primary parallel-fibered bone is characterized by a more parallel distribution of the collagen fibrils, and is typically produced during periosteal and endosteal bone apposition. The mechanical properties are as weak as those of woven bone. Lamellar bone is a well-organized mineralized tissue. Collagen fibrils are distributed in parallel layers that have a thickness of 3 to 5 µm. Osteoid production is slow (1 to 2 µm per day) compared with woven bone, and it takes about 10 days to be mineralized at a well-defined mineralization front. Lamellar bone needs a pre-existing bone surface to be produced by osteoblasts, which means that, unlike woven bone, it is not able to bridge gaps.
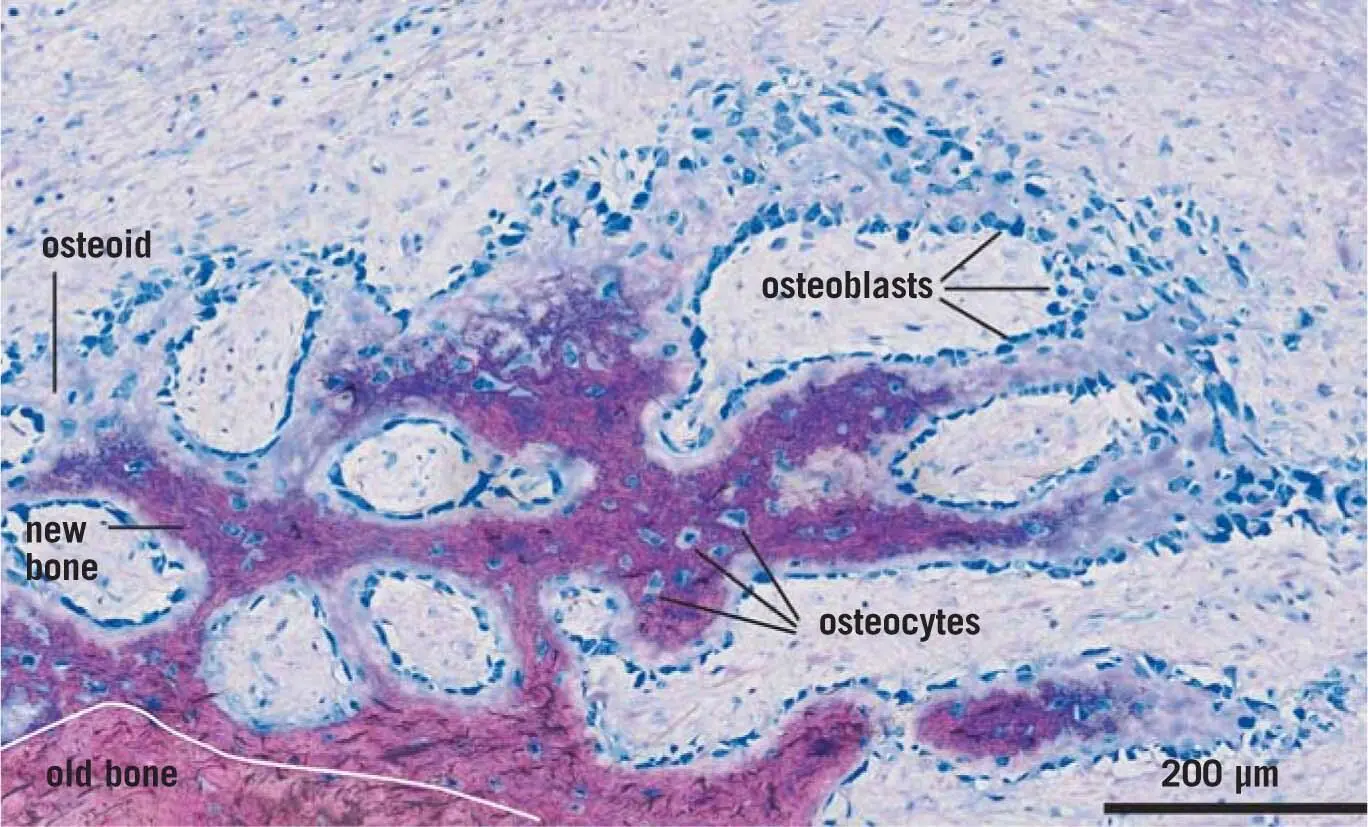
Fig 1-1Osteoblasts produce bone on the surface of a host bone. Bone formation occurs on the surface of existing bone (pink). New bone (dark purple) is lined by seams of osteoblasts and arranged in osteonal structures. Osteoid (barely stained) is bone that is not yet mineralized. The direction of new bone formation can be anticipated by the sprouting of extension into the defect area. [The image is of pig bone.]
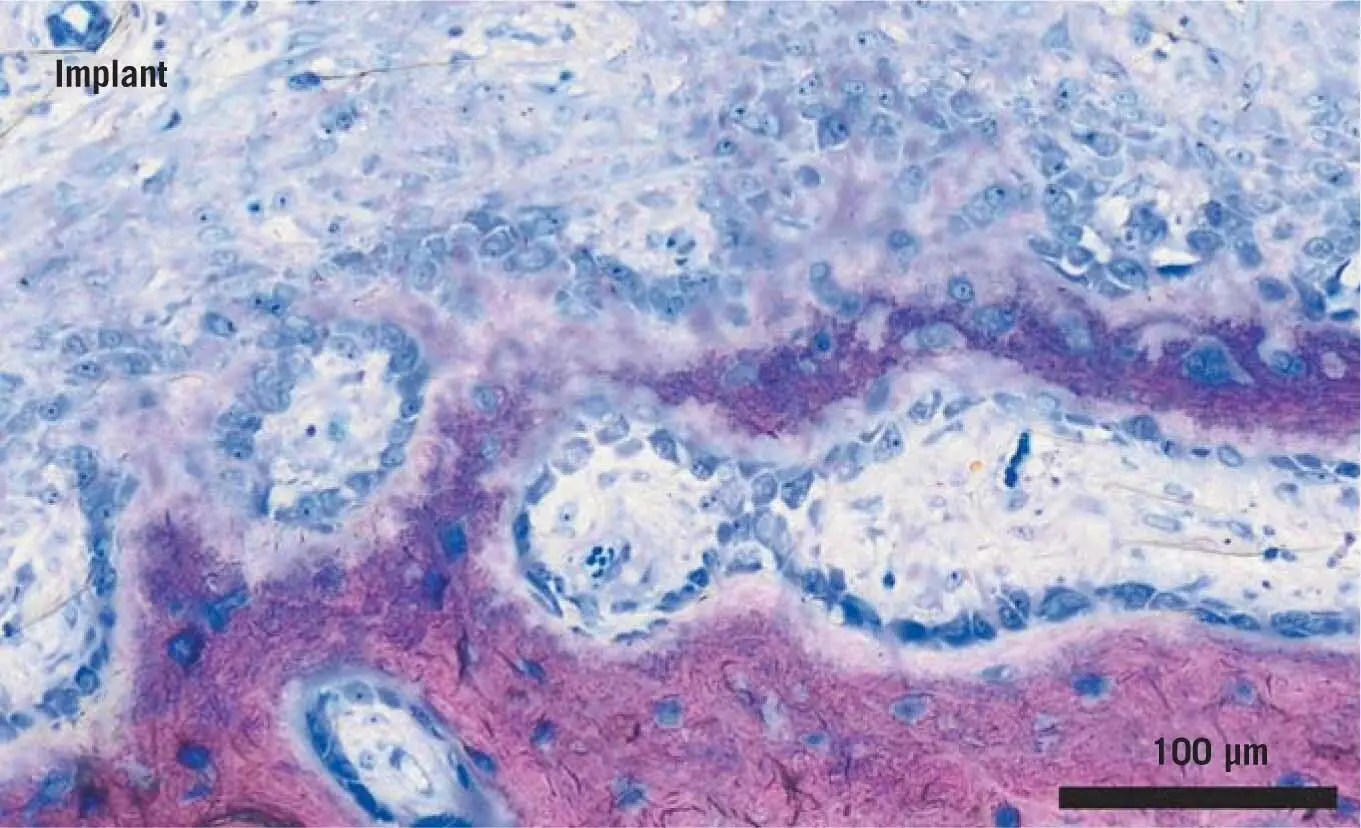
Fig 2-1Osteoblast seams during the early stages of bone formation. Bone formation is the consequence of osteoblast activity. Osteoblasts dominate the scene, and non-mineralized bone (osteoid) is visible. [The image is of pig bone.]
When not active in osteoid production, osteoblasts can differentiate into bone-lining cells. This particular conformation determines a flat distribution of osteoblasts over the bone surface, creating a barrier-like layer between the bone and the extracellular space that seems to be responsible for ion exchange. The bone lining cells may also be responsible for bone resorption through two mechanisms: the first is determined by cell contraction and subsequent bone surface exposition; the second is defined by the direct secretion of osteoclast activating factors.
Osteocytes are characterized by a slower metabolism than osteoblasts and present elongations of the cytoplasmic membrane that connect osteocytes to each other and to the surface cells through gap junctions, creating a three-dimensional canalicular network in the mineralized tissue that is particularly impressive in the osteons ( Fig 1-3). The diffusion of nutrients and ions, otherwise impossible, is guaranteed by this cell network. A limit in diffusion through the canalicular system exists, which is approximately 100 µm. This is also the mean wall thickness of osteons in the cortical bone and also the packets in trabecular bone. The osteocytes, which control the effector cells (the osteoclasts and osteoblasts), 7,10,33require a long lifespan because they are embedded in lacunae within the mineralized matrix, and are connected via dendritic processes that run through the canaliculi. The dense, interconnected network that spans the entire skeleton also connects to blood vessels and to the cells on the bone surface, e.g. the lining cells, osteoblasts, and osteoclasts. As recently summarized, 151 mm 3of bone contains about 20,000 to 30,000 osteocytes, each having 100 dendritic processes and a radius of approximately 70 nm. Around 40 billion (10 9) osteocytes with 20 trillion (10 12) connections and a total length of dendritic processes of 200,000 km can be calculated for the entire skeleton. The surface area and the volume of the lacuno-canalicular network are around 200 m 2and 40 cm 3, respectively. Osteocytes are not only interconnected via their dendritic processes but are surrounded by a liquid that connects them to the overall circulation. Osteocytes are obviously predestined to control bone homeostasis at the local and systemic levels. For example, osteocytes are the cells that almost exclusively produce sclerostin, an inhibitor of the Wingless-related integration site (Wnt) signaling pathway. 129,130The molecular function becomes obvious when one considers bone overgrowth, including the jaw and facial bones of sclerosteosis and van Buchem disease, which are caused by the loss of sclerostin expression and secretion, respectively. 128,130Mouse models lacking sclerostin also display systemic high bone mass, and increased alveolar bone and cementum. 77,82Osteocytes are also a main source of RANKL required for physiologic bone remodeling and in pathologic situations, including ovariectomy, 45,94secondary hyperparathyroidism 140or glucocorticoid excess. 92Mice lacking osteocyte-derived RANKL even resist the bone loss caused by tail suspension. 93Recently, osteocyte-derived RANKL was considered relevant in inflammatory osteolysis 51and orthodontic tooth movement. 109Thus, osteocytes control bone formation and bone resorption during good health and during disease, including their expression of sclerostin and RANKL.
Читать дальше