Thanks also to the further Director of the Department of Cranio-Maxillofacial Surgery, University Hospital Münster, Prof. Dr. mult. Ulrich Joos, as well as to the actual Director, Prof. Dr. Dr. Johannes Kleinheinz, for their scientific support.
My sincere thanks go to the entire team at Quintessence Publishing, especially Dr. Horst W. Haase, Mr. Christian Haase, Mr. Johannes Wolters, and Mrs. Anita Hattenbach, for their support and patience over the years. Many thanks also to Mrs. Avril du Plessis for the excellent correction and editing as well as to Mrs. Ina Steinbrück for the perfect layout.
Finally, the most important thanks are for my wife, Michaela, and my children, Chantal, Elias, and Chérine, for their love, great support, and endless understanding.

Fouad Khoury
Olsberg, Easter 2021
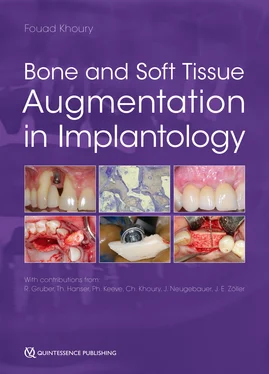
Editor
KHOURY Fouad, DMD, PhD
Director
Privatklinik Schloss Schellenstein
Olsberg, Germany;
Professor
Department of Cranio-Maxillofacial Surgery
University Hospital Münster, Germany
Contributors (in alphabetical order)
GRUBER Reinhard, DMD, PhD
Professor and Chair
Department of Oral Biology
School of Dentistry
Medical University of Vienna, Austria
HANSER Thomas, DMD, M.Sc.
Deputy Director
Privatklinik Schloss Schellenstein
Olsberg, Germany;
Senior Academic Lecturer
Department of Postgraduate Education
Goethe University Frankfurt, Germany
KEEVE Philip L., DMD, M.Sc.
Private Office for Periodontology and Oral Surgery
Hameln, Germany
KHOURY Charles, DDS, DES, CES, M.Sc.
Professor
Department of Prosthodontics
School of Dentistry
St. Joseph University, Beirut, Lebanon
NEUGEBAUER Joerg, DMD, PhD
Professor
Steinbeis University Berlin, Transfer-Institut, Management of Dental and Oral Medicine;
Senior Academic Lecturer
Interdisciplinary Department for Oral Surgery and Implantology
Department of Craniomaxillofacial and Plastic Surgery
University of Cologne, Germany;
Senior Oral Surgeon
Group Office for Implantology, Dr. Bayer and colleagues, Landsberg am Lech, Germany
ZOELLER Joachim, MD, DMD, PhD
Professor and Chairman
Interdisciplinary Department for Oral Surgery and Implantology
Department of Craniomaxillofacial and Plastic Surgery
University of Cologne, Germany
Foreword
Foreword of the first edition
Preface
Acknowledgments
Editors and Contributors
1 Biology of bone regeneration in augmentative procedures
Reinhard Gruber
1.1 Introduction
1.2 Cells of bone remodeling
1.3 Biology of bone regeneration
1.4 Autograft resorption
1.5 Osteoconductive characteristics of autografts
1.6 Osteogenic properties of autografts
1.7 Osteoinductive properties of autografts
1.8 Summary
1.9 References
2 Diagnosis and planning of the augmentation procedure
2.1 Introduction
2.2 Patient consultation
2.3 Anamnesis
2.4 Specific findings
2.5 Choice of grafting technique
2.6 Conclusion
2.7 References
3 Soft tissue management and bone augmentation in implantology
3.1 Introduction
3.2 The basics of incisions, suturing techniques, and soft tissue healing
3.3 Instruments
3.4 Soft tissue management before augmentation
3.5 Soft tissue management during augmentation and implantation
3.6 Soft tissue management during implant exposure
3.7 Soft tissue management following prosthetic restoration
3.8 References
4 Mandibular bone block grafts: diagnosis, instrumentation, harvesting techniques, and surgical procedures
4.1 Introduction
4.2 Biologic procedure for mandibular bone grafting
4.3 Techniques and methods for intraoral bone harvesting
4.4 Augmentation techniques
4.5 Bone remodeling and volume changes after grafting
4.6 Conclusion
4.7 References
Special Appendix
A. Use of the maxillary tuberosity (MT) in the immediate dentoalveolar restoration (IDR) technique
References
B. The palatal bone block graft (PBBG)
References
C. Alumni case reports
5 Bone grafts from extraoral sites
5.1 Introduction
5.2 Bone harvesting from the calvaria
5.3 Bone harvesting from the tibia
5.4 Bone harvesting from the iliac crest
5.5 References
6 Clinical and scientific background of tissue regeneration via alveolar callus distraction
6.1 Introduction
6.2 History of the callus distraction
6.3 Principles of the callus distraction
6.4 Devices
6.5 Surgical technique
6.6 Distraction in different areas
6.4 Conclusion
6.5 References
7 Complex implant-supported rehabilitation from the temporary to the definitive restoration
7.1 Introduction
7.2 Specific aspects of temporary restorations
7.3 Treatment planning
7.4 Classification of temporary restorations
7.5 Restorative concept
7.6 Fixed complex restoration: step by step
7.7 Long-term provisional
7.8 Surgical procedures
7.9 Final restoration
7.10 Concluding remarks
7.11 References
8 Risk factors and complications in bone grafting procedures
8.1 Introduction
8.2 Risk factors
8.3 Intraoperative complications
8.4 Postoperative complications
8.5 Complications during implant placement after bone grafting
8.6 Complications during implant exposure
8.7 Late complications after prosthetic restoration
8.8 References
Index
1
Biology of bone regeneration in augmentative procedures
Reinhard Gruber
Regenerative dentistry critically depends on the functional understanding of bone biology – to be precise, bone development, bone modeling and remodeling and bone regeneration – in a physiologic but also in a pathologic and pharmacologic context. Bone biology also describes the cellular and molecular regulation behind Wolff’s law (form follows function), which was later refined by Frost’s Mechanostat theory. 44Bone biology is a molecular and cellular system that is essential for mammalian evolution. Besides being a framework connecting to tendons and muscles and for protecting the bone marrow, the skeleton is a storage for calcium and phosphate that is transported via the umbilical vein and later through the mother’s milk into the fetus and newborn. Understanding the delicate interplay of bone-forming cells and bone-resorbing cells – which act in concert with the osteocyte located within the bone matrix, the blood vessels providing support for the respective progenitors, and the cells originally dedicated to the immune system – provides one part of the information necessary for progress in medicine.
The concert has to be orchestrated, which is, in the context of bone biology, the cell-to-cell communication involving the classical path. This path can roughly be divided into local and systemic regulation. Local regulation includes cell communication via cytoplamatic connections or the release of signaling molecules, with particular receptors on the respective target cells. Systemic regulation refers to the endocrine system, whereby hormones or growth factors are released and transported via the bloodstream to target cells elsewhere in the body. It is fascinating to imagine all the different levels – molecular, cellular, tissue, and organ – to be coordinated, with the same aim of homeostasis. In a broader sense, not only does homeostasis maintain the tissue (which would be bone remodeling), it is also the mechanism to regain homeostasis after injury, thus bone regeneration. However, the delicate cellular and molecular mechanisms aiming for homeostasis are sensitive to change; for instance, the drop of steroid hormones during menopause, which causes not only enhanced but also disbalanced bone remodeling and ultimately leads to bone loss and postmenopausal osteoporosis. The mechanical integrity, particularly of the trabecular bone, is rapidly impaired, and fragility fractures of the vertebra and the hip become clinical hallmarks of the disease. 107Postmenopausal osteoporosis is but one example of how bone homeostasis undergoes a catabolic shift that, together with age-related changes, leads to a progression of bone loss over time.
Читать дальше