Fig 1-4Case 3. (a) Preoperative view (1993). The occlusal view shows a distal extension situation in the left mandible. This woman’s healed ridge was atrophic with a severe buccal flattening. (b) The intraoperative view shows a crest width of less than 3 mm. (c) Status following horizontal ridge augmentation with two block grafts harvested in the third molar area within the same flap. (d) The block grafts were covered with an ePTFE membrane. The membrane was stabilized with multiple miniscrews. (e) The surgery was completed with a tension-free wound closure with mattress and single sutures to achieve a primary wound healing. (f) Clinical status after 6 months of healing free from complications. (g) Following flap elevation and membrane removal, an excellent augmentation outcome is visible in the areas of the first premolar and first molar, allowing for implants to be placed. (h) Following successful restoration, the periapical radiograph at the 1-year examination (1994) shows stable bone crest levels at all three tissue-level implants. (i) Clinical status at the 15-year examination. The peri-implant mucosa is stable but shows some signs of mucositis. (j) The radiograph confirms stable bone crest levels at all three tissue-level implants. (k) Clinical view at the 25-year follow-up examination (2019). The patient is now 85 years old, and the plaque control is no longer optimal. The mucosa around the tissue-level implants with a machined implant surface in the neck area show very stable peri-implant tissues. (l) The periapical radiograph confirms stable bone crest levels at all three tissue-level implants after 25 years of function. (m) A CBCT scan is taken to examine the peri-implant bone volume. The orofacial cuts demonstrate fully intact buccal bone walls at the two implants in the first premolar and first molar sites, where a block graft augmentation with GBR was done in 1993.
In 1994, an expert meeting took place in the United States to discuss the potential and the limitations of the GBR technique used in daily practice after 5 years of clinical experience (Fig 1-5). This meeting clearly showed that improvements of the GBR technique were needed to allow more widespread use in implant patients. The experts agreed that the GBR technique—based on the use of ePTFE membranes in combination with bone grafts or bone substitutes—had the following weaknesses and shortcomings:
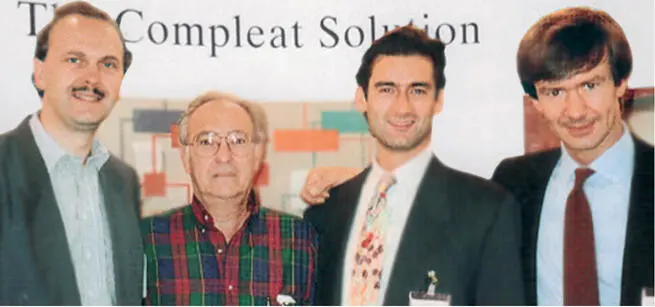
Fig 1-5Photo of the expert meeting in 1994 in Arizona with (from the left) Danny Buser, Bill Becker, Sascha Jovanovic, and Massimo Simion.
A significant rate of membrane exposures due to soft tissue dehiscences, often leading to local infection beneath the membrane and subsequently to a compromised regenerative outcome of the GBR procedure. 57 – 60
Difficult handling of the membrane during surgery due to its hydrophobic properties, requiring stabilization of the membrane with miniscrews or pins. 55 , 56 , 61
The need for a second surgical procedure to remove the bioinert, nonresorbable membrane, thereby increasing the morbidity and overall treatment time for the patient.
During this meeting, objectives were defined to improve the predictability and attractiveness of GBR procedures both for implant patients and for clinicians ( Box 1-1).
Box 1-1Objectives for improvements of the GBR technique in the mid 1990s
Improve the predictability of successful outcomes following GBR
Reduce the rate of complications due to membrane exposure and membrane infections
Make the GBR technique more user friendly, with easier application of the membrane during surgery
Make GBR more patient friendly by eliminating a second surgical procedure for membrane removal whenever possible, and by reducing healing periods as much as possible
It was clear to the participants at this expert meeting that these objectives could only be achieved with the use of a bioresorbable membrane. This trend was again initiated in the field of GTR, with the introduction of the first bioresorbable membranes in the early 1990s. 62 , 63 Subsequently, numerous animal studies were performed to examine different bioresorbable membranes for GBR procedures. 64 – 74 In general, two different groups of bioresorbable membranes were evaluated 75 :
Polymeric membranes made of polylactic or polyglycolic acid
Collagen membranes produced from various animal sources
Paralleling these preclinical studies, clinicians started to use bioresorbable membranes in patients. The first published clinical reports predominantly tested collagen membranes, 76 – 80 and today, collagen membranes are routinely used in daily practice for GBR procedures.
In addition to selecting an appropriate barrier membrane, the selection of appropriate bone fillers for GBR procedures is just as important for the regenerative outcome of GBR procedures. In the early 1990s, autogenous bone chips were primarily used from a mechanical point of view. The role of these filler particles was to support the membrane to avoid a membrane collapse during healing. In the mid 1990s, a first preclinical study in minipigs by Buser et al 81 helped us to understand that bone fillers have different biologic characteristics in terms of their osteogenic potential and rate of filler substitution during bone remodeling.
The various biomaterials used for GBR procedures, such as bone grafts, bone substitutes, and barrier membranes, are also discussed in chapter 2.
Routine Application and Fine-Tuning Phase of GBR
Around the year 2000, GBR entered a phase of routine application in daily practice. Since then, the GBR technique has been the standard of care for the regeneration of localized bony defects in implant patients. This was confirmed in 2007 in a systematic review by Aghaloo and Moy, 82 who demonstrated that implants placed with the GBR procedure have favorable survival and success rates, and the GBR procedure was the only well-documented surgical technique among various surgical techniques used for localized ridge augmentation. The only other scientifically well-documented surgical technique for bone augmentation at that time was sinus grafting and sinus floor elevation in the posterior maxilla.
Over the past 20 years, however, significant progress has been made with GBR procedures, thanks to new developments in technology and a much better understanding of the tissue and graft biology involved.
The most important improvements are as follows:
The development of a much better 3D radiographic technique based on CBCT
Much greater knowledge of tissue biology in postextraction sites
A much better understanding of the biologic characteristics of bone grafts and bone substitutes
The development of new narrow-diameter implants
CBCT as the new 3D radiographic methodology
The development of the CBCT technique started in the late 1990s with a first publication by Mozzo et al, 83 and it represents probably one of the most important improvements in implant dentistry in the past 20 years. This new 3D radiographic technique allowed cross-sectional imaging with much better image quality and a clear reduction in radiation exposure when compared with the computed tomography (CT) technology used for dentistry in the 1990s. The CBCT technique allows cross-sectional imaging not only for the preoperative examination of patients, but also for the follow-up documentation of bone augmentation procedures. 84 , 85 During preoperative examination, CBCT helps to assess the extent of bone deficiencies in potential implant sites, and hence to categorize defect morphologies. These aspects are discussed in detail in chapter 5. In addition, CBCT is also one of the basic techniques necessary for the use of digital technology, including computer-assisted implant surgery (CAIS) in patients.
Читать дальше