During these early decades, several attempts were made to develop new surgical techniques to augment local bone deficiencies in the alveolar ridge in order to overcome these local contraindications for implant therapy. The proposed techniques included vertical ridge augmentation using autogenous block grafts from the iliac crest in extremely atrophic arches, 24 , 25 sinus floor elevation procedures in the maxilla, 26 – 28 the application of autogenous onlay grafts for lateral ridge augmentation, 29 – 31 or split-crest techniques such as alveolar extension plasty. 32 – 34
During the same period, in addition to these new surgical techniques, the concept of guided bone regeneration (GBR) with barrier membranes was introduced. Based on case reports and short-term clinical studies, various authors reported first results with this membrane technique for the regeneration of localized bone defects in implant patients. 35 – 40
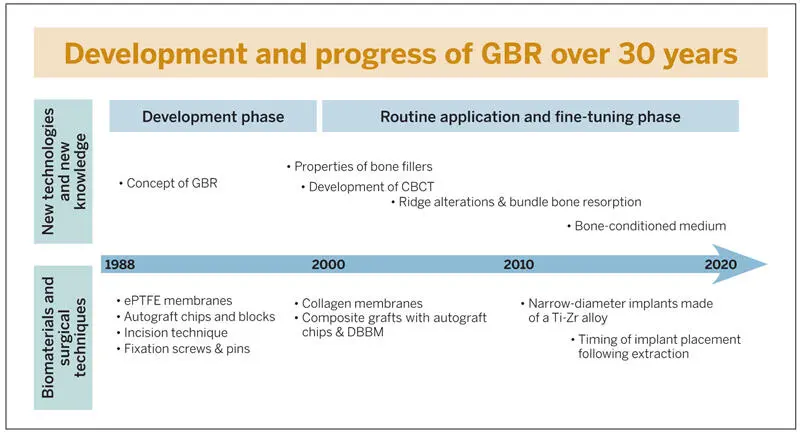
This textbook will provide an update on the biologic basis of the GBR technique and its various clinical applications for implant patients. Clinical experience with GBR in daily practice now spans 30 years. These 30 years can be divided into a development phase and a phase of routine application with extensive efforts to fine-tune the surgical procedure (Fig 1-1). The focus was on improving the surgical technique, expanding the range of applications, improving the predictability for successful outcomes, and reducing morbidity and pain for the patients.
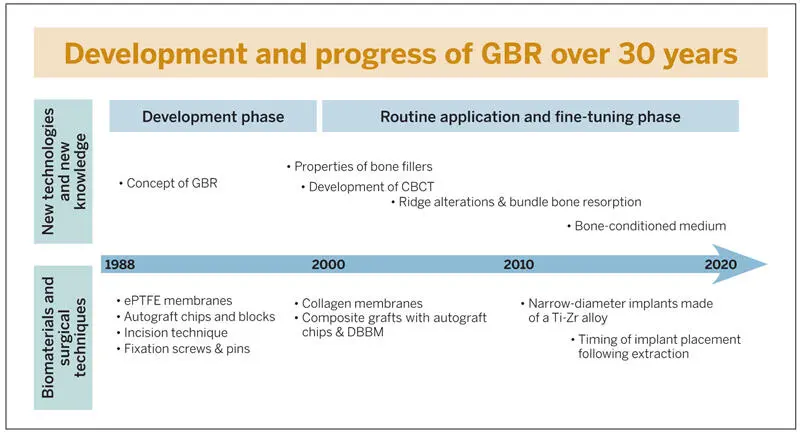
Fig 1-1Development of GBR over 30 years since the late 1980s. ePTFE, expanded polytetrafluoroethylene; DBBM, deproteinized bovine bone mineral; Ti-Zr, titanium-zirconia
Development Phase of GBR
The use of barrier membranes for implant patients was certainly triggered by the clinical application of barrier membranes for periodontal regeneration, called guided tissue regeneration (GTR). GTR was first developed in the early 1980s by the group led by Nyman et al. 41 , 42 The initial studies were performed with Millipore filters, which had already been used in experimental studies in the late 1950s and 1960s for the regeneration of bone defects. 43 – 45 However, these studies had no impact on the development of new surgical techniques to regenerate localized defects in the jaws, since the potential of this membrane application was probably not recognized at that time.
The two papers by Nyman et al 41 , 42 in the field of GTR, both of which demonstrated successful treatment outcomes of GTR procedures, were received with great interest and led to increased research activities in the mid to late 1980s. 46 – 49 These studies were already being performed with expanded polytetrafluoroethylene (ePTFE), which is a bioinert membrane and became the standard membrane for GTR and GBR procedures during the development phase of both techniques. The use of ePTFE membranes for bone regeneration was initiated in the mid 1980s by the group of Dahlin et al, who performed a series of preclinical studies. 50 – 52 These studies confirmed the concept that the application of an ePTFE membrane established a physical barrier that separated the tissues and cells that could potentially participate in the wound healing events inside the secluded space. The barrier membrane promoted the proliferation of angiogenic and osteogenic cells from the marrow space into the bone defect without interference by fibroblasts. These events were nicely demonstrated by Schenk et al 53 in a landmark experimental study in foxhounds. The current biologic understanding of wound healing events in membrane-protected bone defects is presented in detail in chapter 2of this textbook.
The use of ePTFE membranes for GBR procedures started in the late 1980s. The main objective was to achieve regeneration in peri-implant bone defects in implant sites with local bone deficiencies. The GBR technique has been used with both simultaneous and staged approaches. Implant placement with simultaneous GBR was predominantly used for immediate implant placement in postextraction sites to regenerate peri-implant bone defects 35 , 36 , 38 or for implants in sites with crestal dehiscence defects. 40 The staged approach was used in clinical situations with healed ridges but an insufficient crest width. The membrane technique was used to enlarge the crest width with a first surgery, and implant placement took place after 6 to 9 months of healing in a second surgical procedure. 37
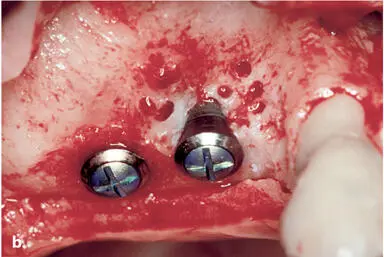
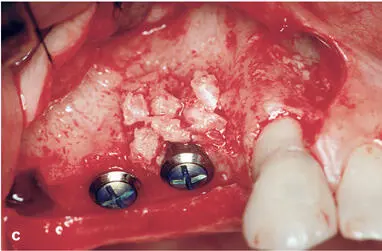
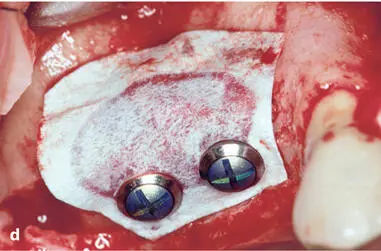
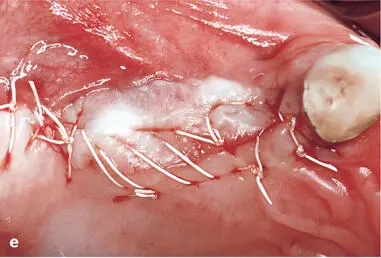
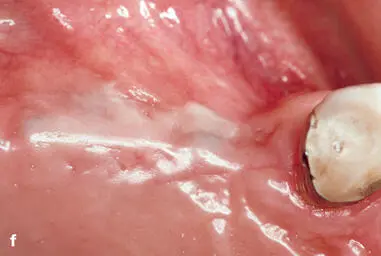
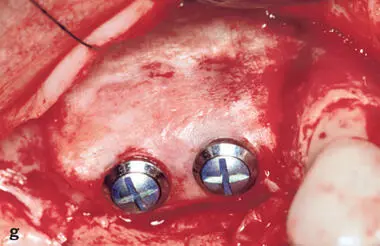
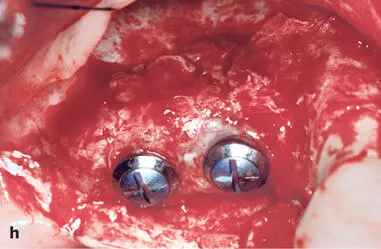
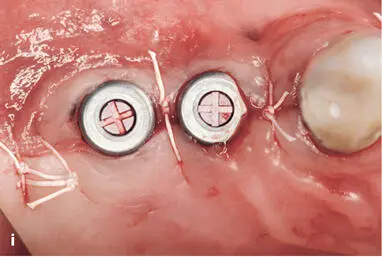
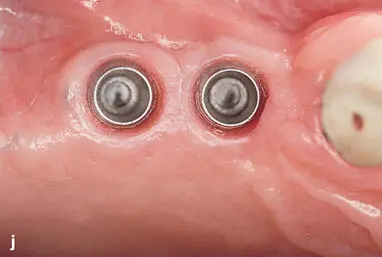
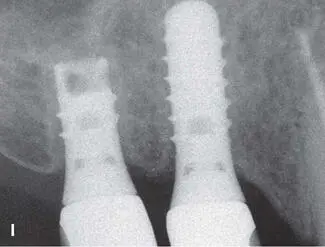
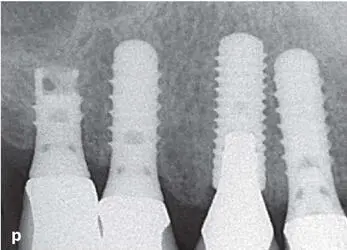
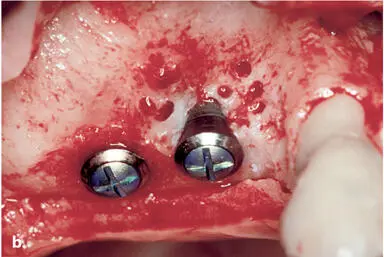
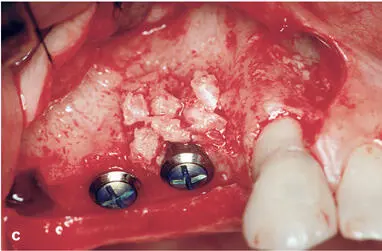
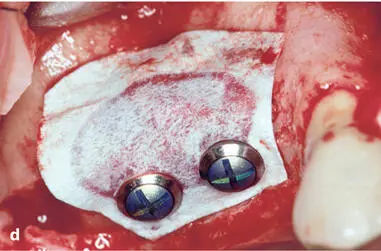
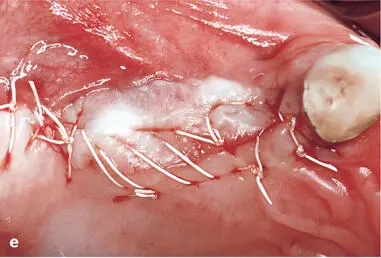
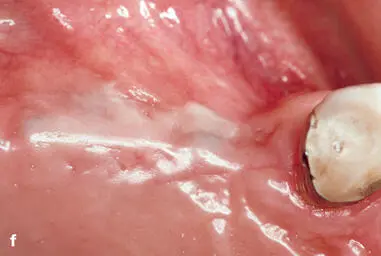
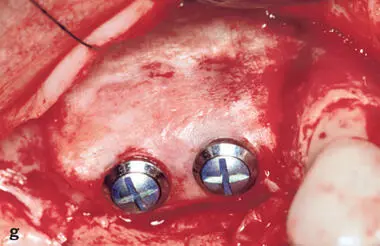
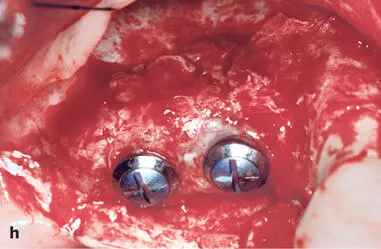
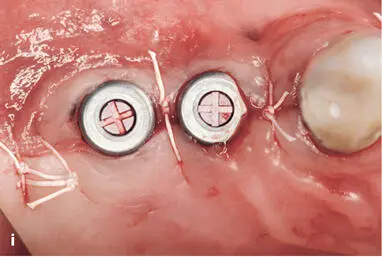
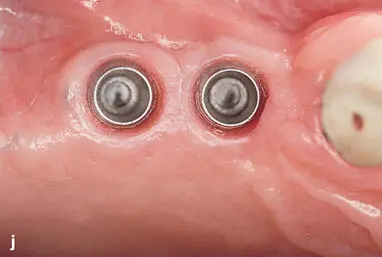
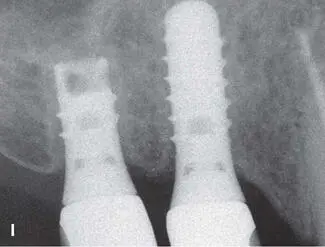
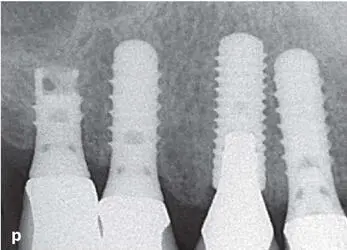
Early on, several complications were observed with both approaches, and modifications of the surgical techniques were proposed to improve the predictability of successful treatment outcomes. One frequent complication was the collapse of the ePTFE membranes, which reduced the volume of the regenerated tissue underneath the membrane. In addition, some of the regenerated sites demonstrated insufficient bone formation and the formation of a periosteum-like tissue underneath the membrane. 37 , 40 Therefore, bone fillers such as autografts or allografts were recommended by various groups, primarily to support the membrane and reduce the risk of membrane collapse. 54 – 56 The combination of ePTFE membranes and autogenous bone grafts provided good clinical outcomes for both approaches. Some of these patients are still being followed and documented up to 25 years after surgery (Figs 1-2 to 1-4).





Читать дальше