Table 1.2 Drugs which may contribute to falls.
| Drug class |
Indications |
Examples of drugs |
| Antipsychotics |
Psychosis delirium |
Haloperidol, Promazine, Trifluoperazine, Quetiapine, Olanzapine, Prochlorperazine. Risperidone |
| Antidepressants |
Mood |
Amitriptyline, Trazodone, Fluoxetine, Citalopram. Paroxetine, Sertraline |
| Hypnotics (sedatives) |
Insomnia |
Zopiclone, Zolpidem |
| Benzodiazepines Hypnotics (sedatives) |
Insomnia, agitation |
Diazepam, Lorazepam, Temazepam, Nitrazepam |
| Anti‐hypertensives |
High blood pressure |
Ramipril, Lisinopril, Perindopril, Valsartan, Hydralazine, Bisoprolol, Atenolol, Propranolol |
| Antidiabetics |
Diabetes |
Glibenclamide, Glipizide, Metformin, Sitagliptin |
| Opiates |
Pain |
Codeine, Tramadol, Morphine, Fentanyl, Buprenorphine, Oxycodone |
| Diuretics |
Heart failure, fluid overload, hypertension |
Bendroflumethiazide, Furosemide, Bumetanide, Amiloride |
| Nitrates |
Cardiovascular disease |
Isosorbide mononitrate, Glyceryltrinitrate (GTN) Nicorandil |
| Parkinson's Medication |
Parkinson's disease |
Co‐Beneldopa, Co‐Careldopa, Selegline Hydrochloride, Pramipexole |
| Non‐steroidal anti‐inflammatory drug (NSAIDS) |
Pain, inflammation |
Ibuprofen, Naproxen, Diclofenac |
| Antimuscarinics (anticholinergics) |
These are mentioned in other classes, e.g. for urinary incontinence |
Procyclidine, Oxybutynin, Tolterodine, Amitriptyline |
| Aminoglycosides |
Infection |
Vancomycin, Gentamicin |
| Antihistamines |
Allergies, itch |
Chlorphenamine, Hydralazine, Cetirizine |
ADMINISTERING DRUGS SAFELY
Drug Administration Competence
Many hospitals have drug administration competencies for staff to ‘prove’ that they are competent in the clinical skill of drug administration. Only when these competencies have been signed off can a nurse administer medications alone. Also, the student in healthcare, i.e. Registered nurse, Nursing Associate, etc. will need to be signed off in their medicines management competencies as part of their pre‐reg training. Appendix 1shows an adaption of a typical section of post‐reg medicines management competencies.
Also, in order to be able to administer intravenous medications, qualified staff are required to pass a drug calculations test to prove mathematical ability, as poor mathematical skills have been indicated in medication errors with the misplacement of the decimal point leading to a tenfold error overdosing or underdosing. Many healthcare environments also set calculation tests during the interview stage.
Activity 1.4shows a sample question of the sort that you may be expected to answer in one of these tests. Don't worry if your reaction to answering these questions is  we'll go through this in Chapter 4.
we'll go through this in Chapter 4.
 Activity 1.4
Activity 1.4
Drug calculations sample question.
A drug is presented as 5 g in 500 ml A patient weighing 70 kg is prescribed 10 mg/kg/h of the drug.
1 How many milligrammes per hour of the drug does the patient need?
2 How many millilitres per hour do you set the infusion pump?
 To first work out how much of the drug the patient requires according to their body weight we use the formula weight (kg) × dose, and then using the formula:
To first work out how much of the drug the patient requires according to their body weight we use the formula weight (kg) × dose, and then using the formula:
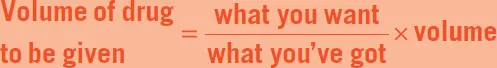
But remember to keep the decimal units the same throughout the formula.
Reports and Safety Alerts
In order to alert health carers of the problems around drug administration, the Department of Health and National Safety Patient Agency (NPSA) issue reports and safety alerts, perhaps when mistakes have been made for shared awareness:
Problems with missed doses,
Promoting safer use/monitoring of patients on anticoagulant therapy (e.g. warfarin for deep‐vein thrombosis [DVT]),
Promoting safer measurement and administration of liquid medicines,
Promoting safer use of injectable medicines,
Safer practice with epidural injections and infusions.
 Department of Health
Department of Health
The government department responsible for health regulation and policy in the United Kingdom.
Venous thromboembolism (VTE)
A medical condition including DVT, whereby a blood clot forms inside a vein, and pulmonary embolism (PE), whereby part of the DVT breaks off and travels to the lungs, blocking the blood flow.
Improving Medication Safety
The NPSA produced seven key actions to improve medication safety which are still relevant today ( Table 1.3).
Why do you think it is important that we know not just what medications the patients are allergic to, but also what foodstuffs?
Patient Self‐Administration of Medication
Health carers often take over the medication care of in‐patients with diabetes and mess up their blood sugars by not being able to deliver their insulin and other medications at the correct times. Patients with Parkinson's disease also have strict regimes and we may again fail to deliver their medications on time, with profound effects on their independence and wellbeing. Many hospitals now have secure boxes at the bedside for patients to store their medication and allow them to self‐medicate.
Table 1.3 Seven key actions to improve medication safety.
Source: Department of Health (2007).
| Increase reporting |
Increase reporting and identify actions against local risks by way of an annual medication report: clinical risk. |
| Implement NPSA safer medication practice recommendations |
Implement NPSA recommendations – audit safer medication practice – includes alerts on anticoagulants, injectable medications, and wrong‐route errors. |
| Improve staff skills and competencies |
Improve skills: preceptorship competencies will help nurses to work towards the required level of competence. |
| Minimise dosing errors |
Minimise errors: information, training, and tools to make calculations easier. |
| Ensure medicines are not omitted |
It also can be linked with neglect when medications are not given. The NPSA reviews medicine storage and medication supply chains. |
| Ensure medicines are given to the correct patient |
Ensure correct medications with correct patient – improve packaging and labelling of medicines – support local systems that make it harder for staff to select the wrong medicine. |
| Document patient's medicine allergy status |
Document: improve recording of patient's allergy status. |
Remember that not all patients have the ability to do this; for example, patients with dementia or those too ill to administer their own medication. But please remember, patients with dementia may have windows of opportunity whereby they can self‐medicate. As with all health care, this aspect of their care must be monitored frequently. Many patients in the community have their medication distributed by their pharmacist into ‘dosset’ boxes, boxes that have timed sections or partitioned by morning, afternoon, or evening, in order for them to take their medication.
Читать дальше
 we'll go through this in Chapter 4.
we'll go through this in Chapter 4. Activity 1.4
Activity 1.4 To first work out how much of the drug the patient requires according to their body weight we use the formula weight (kg) × dose, and then using the formula:
To first work out how much of the drug the patient requires according to their body weight we use the formula weight (kg) × dose, and then using the formula: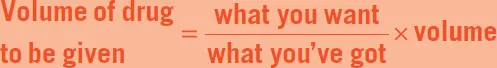
 Department of Health
Department of Health