Becoming a Reflective Practitioner
Здесь есть возможность читать онлайн «Becoming a Reflective Practitioner» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Becoming a Reflective Practitioner
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Becoming a Reflective Practitioner: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Becoming a Reflective Practitioner»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Becoming a Reflective Practitioner
Becoming a Reflective Practitioner
Becoming a Reflective Practitioner — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Becoming a Reflective Practitioner», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
The reality of today’s NHS is that nurse shortages are reportedly reaching crisis point (Hall 2003); bed occupancy is constantly ‘red alert’. In such an environment, Wall et al. (1997) note that NHS staff suffer considerably more stress than any other workforce, with 28% recording levels above the symptom threshold. Wind the clock forward. BBC News reports that NHS Foundation Trusts need to resubmit their financial plans. Only essential posts should be filled. The news asks what impact on patient care. What impact on staff morale and stress. Pick up my local newspaper and staff morale at RCHT is low. 10 Wind the clock forward to the 2019 general election and the conservatives are proposing 50 000 more nursing jobs. Tides turning. So why let it get so bad in the first place and putting lives at risk and in misery for both patients and staff?
Tools such as the feeling fluffy–feeling drained scale can help practitioners focus on stress factors and work at reducing them. At the end of your next shift, stop, reflect, and mark how stressed you feel along with the feeling fluffy–feeling drained visual analogue scale ( Figure 4.2). 11
Stewing in our own juices is not healthy. Imagine your body is like a water butt‐ slowly filling with stress. As it fills, we are more tired and more intolerant but contain it, that is until you feel you are drowning and then one of two things happens. Either you blow up inside and have a breakdown, or else you snap and ‘blow your top’. You rage at events or people (Wilkinson 1988; Parker 1990; Pike 1991).
Pike (1991, p. 351) writes:
Moral outrage ensues when the nurse’s attempts to operationalize a choice is thwarted by constraints. The outrage intensifies when these constraints not only block action, but also force a course of action that violates the nurse’s moral tenets.
Then ask yourself:
What factors contribute to your sense of feeling drained?
What factors contribute to your sense of feeling light and fluffy?
What do you need to do to home feeling more fluffy and less drained?
Use this scale over a period of time to monitor stress patterns and any improvement in your ‘fluffiness’. 12
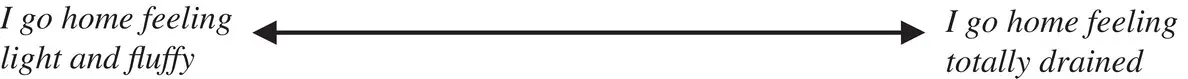
FIGURE 4.2 The feeling fluffy–feeling drained scale.
Many practitioners wear this T‐shirt. However, the water butt does have a drainage tap. Through reflection, the practitioner can learn to monitor her stress levels and open her tap. She can then drain and convert the stress into positive energy necessary to take appropriate action to resolve the sources of stress (Hall 1964) just as the gardener draws water from the water butt to water the flowers and nourish their growth. However, the tap might be blocked, requiring help to unblock it – again, the value of guidance. If stress accumulates then the risk of burnout looms large on the horizon. Cherniss (1980) describes burnout as a process in which ‘the professional’s attitudes and behaviours change in negative ways in response to job strain’ (p. 5). Maslach (1976) suggested that the major negative change in those experiencing burnout in people‐centred work was ‘the loss of concern for the client and a tendency to treat clients in a detached, mechanical fashion’ (p. 6). McNeely (1983) observed that when practitioners felt they had lost the intrinsic satisfaction of caring, they became focussed on the conditions of work, for example, off duty rosters and workload issues, characteristic of bureaucratic models of organisation. McNeely believes that bureaucratic conditions are antithetical to human service work and strongly advocated that such organisations needed to move to collegial ways of working staff in order to offset the risks of burnout. Burnout is a descent into a black hole when the caring self has been scrapped away on the uncaring sharp edges of systems.
And yet, burnout can be a healing space, where the practitioner can recover/discover herself. It may be dark, lonely, and painful but it can still be a necessary healing space. Such healing is a journey to discover rather than recover because recovery suggests returning to what she was before, only for the hurting to start all over again.
Benner and Wrubel (1989) believe that the answer to stress and burnout is to reconnect to caring rather than the development of personal detachment, as advocated by Menzies‐Lyth (1988). Caring is a reciprocal relationship. If nurses and other healthcare practitioners are expected to care, then they need to work in caring environments. If the practitioner is suffering, it is likely that other colleagues also suffer, sapping their energy and limiting their availability to be with patients. And yet often, practitioners seem to need to cope, to not expose their vulnerability as if it is a weakness not to cope or admit to strain. They would prefer a collusive silence. To care, we need ways to penetrate the silence to support each other and create a therapeutic team – a team whereby its members are actively and genuinely available to each other. As such, the reflective practitioner is mindful of their colleague's well‐being. Then suits of armour can be discarded.
Consider the following questions:
Are adequate support systems in place?
Are people stressed or worse, burnt‐out?
If so, why do you think that is?
Do you see seeking help as a strength rather than weakness?
Do you explore your anxiety as a learning opportunity?
Are you truly available to support your colleagues?
The human response to manage anxiety is to control their environment, and with it, the source of their anxiety. Unfortunately, the mismatch of expectations within healthcare is wide with a consequential impact on morale and patient care.
It follows that the ability to know and manage self or ‘poise’ is a vital attribute of the practitioner seeking to realise desirable practice. Practitioners may well sacrifice integrity to manage anxiety and stress, and thus view the reflective project as an overt threat to their security or rather their insecurity. In my experience, very little education in practitioner training focuses on self‐management except perhaps an hour or two on stress management.
How Do I Now Feel About the Situation?
Having worked through the MSR cues, the practitioner will feel positive and in control of their practice, prepared to move into the third and fourth dialogical movements. Whilst negative feelings and anxiety may not have been totally eclipsed, at least the practitioner can acknowledge and understand them. The value of reflection is reinforced, and with it, a stronger sense of purpose and commitment towards a practice that the practitioner can acknowledge as they close the reflective spiral.
Through writing and reflection, the practitioner naturally learns to pay attention to their everyday experiences. In doing so, their practice becomes more alive and meaningful. They become increasingly mindful of self within practice itself. Things are less taken for granted. Practitioners become more curious, more questioning. The gate is open to becoming a reflective practitioner as someone who lives reflection in his or her everyday practice.
Summary
The MSR is designed to enable the practitioner to reflect on experience towards gaining insight. It offers insight into the potential breadth and depth of reflection yet always remembering that it is a heuristic rather than prescription. Besides enabling practitioners to explore reflection, the MSR also enables the development of clinical skills. An application of the MSR is set out in chapter 8. In the following chapter, I set out a framework for perceiving insights.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Becoming a Reflective Practitioner»
Представляем Вашему вниманию похожие книги на «Becoming a Reflective Practitioner» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Becoming a Reflective Practitioner» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.