1 ...8 9 10 12 13 14 ...21 A contrast CT scan is a very reasonable first imaging study to determine the extent of bone invasion of the hard palate and upper alveolus and will determine if any neural foramens are widened in keeping with perineural invasion. An MRI scan might be necessary and is used more often to determine the extent of soft tissue invasion and to determine if any perineural invasion is present. MRI is also helpful in distinguishing between different salivary tumors.
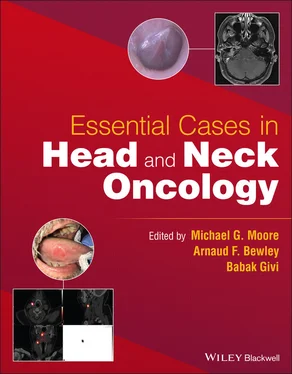
A core biopsy was done and reported as adenoid cystic carcinoma. A CT scan and MRI scan were done. The results of the MRI scan are shown in Figure 6.2.
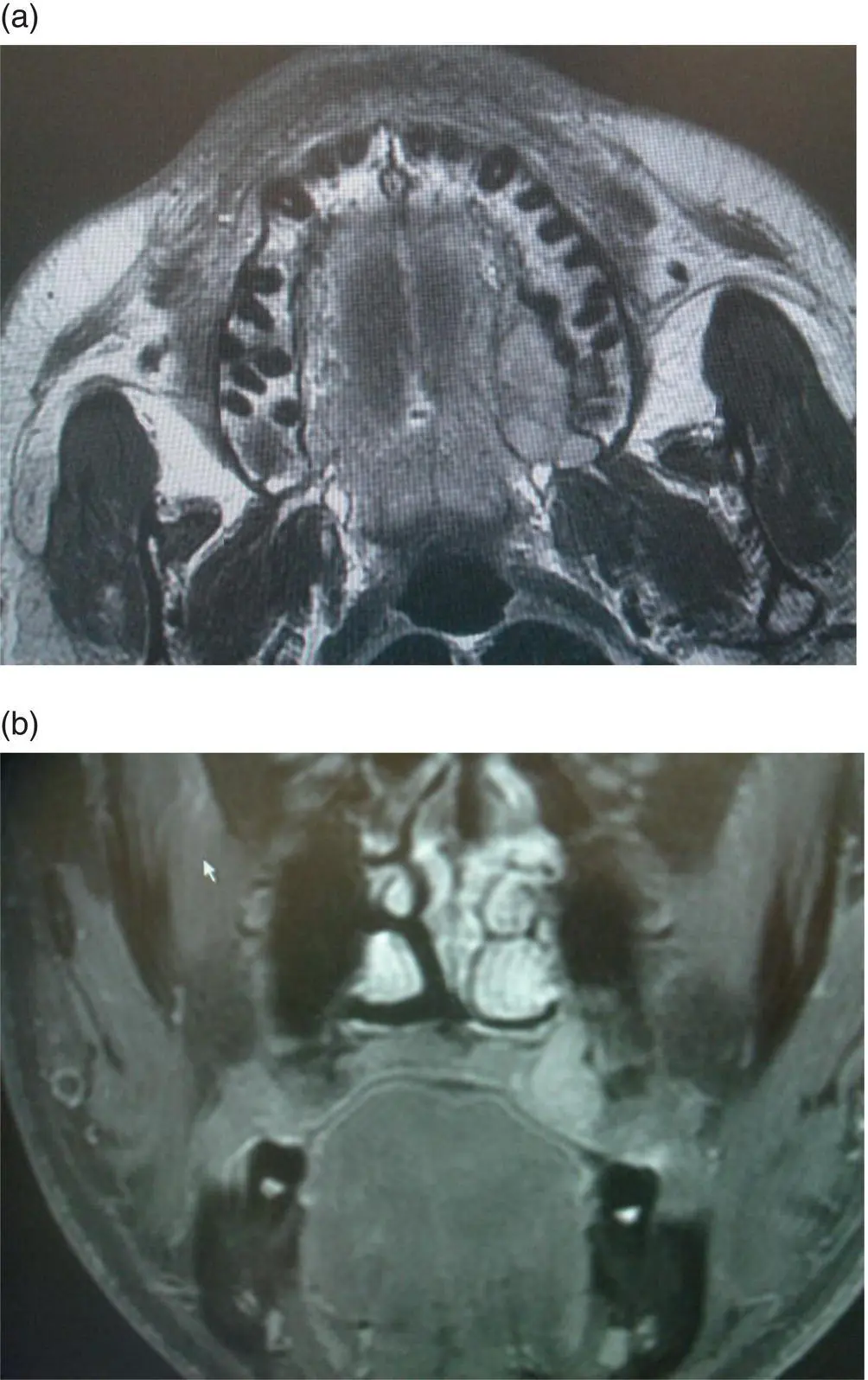
FIGURE 6.2 An axial T1‐weighted MRI image without contrast (a) and a coronal T1‐weighted MRI with contrast (b) show an enhancing submucosal lesion of the left hard palate.
Question: What are the pertinent findings in MRI on your review?
Answer:The MRI shows widening of the palatine canal, which is most likely due to the perineural invasion of the greater palatine nerve.
Question: What is the recommended management for this patient?
Answer:Adenoid cystic carcinoma is best managed by wide surgical resection followed by adjuvant radiation unless the tumor is considered unresectable. In this particular case, the extent of perineural invasion was limited to the greater palatine nerve with no extension to the skull base or cavernous sinus. The tumor was, therefore, deemed to be resectable. Due to the presence of perineural invasion and high incidence of positive margins in adenoid cystic cancer, adjuvant radiotherapy is recommended in the majority of cases to improve local control.
Question: What is the extent of surgery? What approach would you recommend?
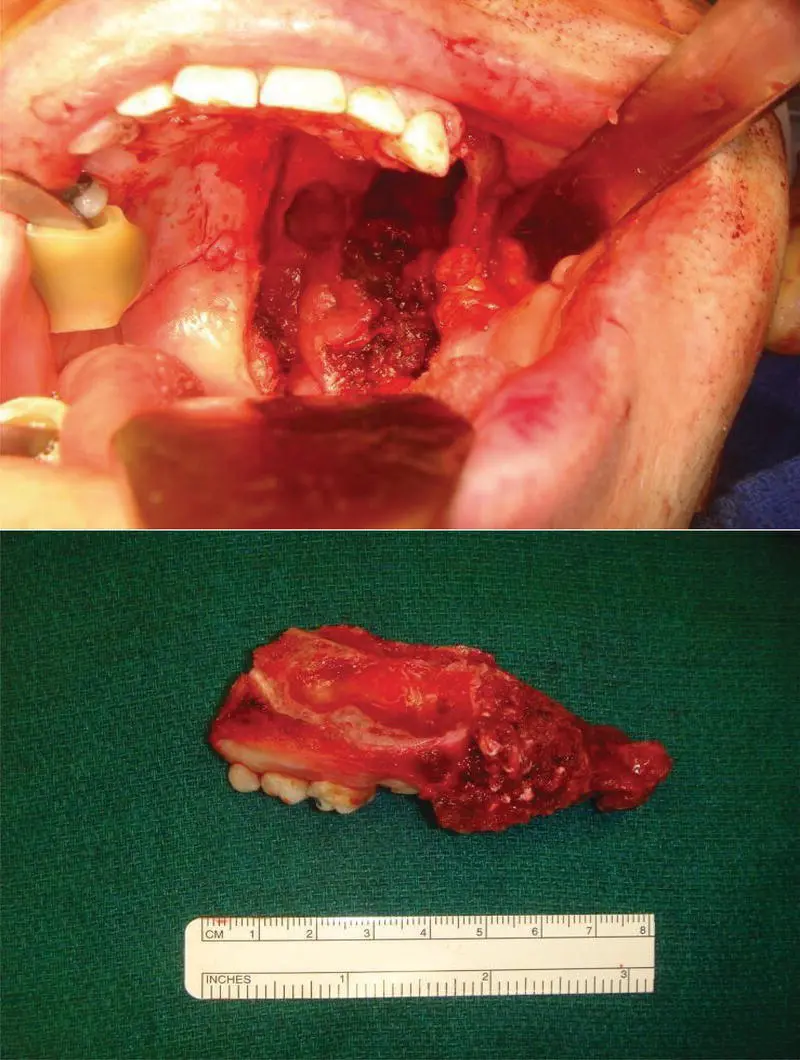
Answer:Based on the extent of the tumor on imaging and exam, peroral left infrastructure maxillectomy with resection of the hard palate, upper alveolus incorporating the palatine canal, and pterygoid plates appears to be a reasonable approach. The steps involved in the surgery are summarized in Figure 6.3.
An infrastructure maxillectomy is started by completing mucosal cuts to allow for at least a 1 cm soft tissue margin around the visible and palpable tumor. The next steps in the maxillectomy are accomplished by performing bone cuts. This is first done through the use of an oscillating saw. Due to the risk for bleeding, the posterior cut is often saved for last and is accomplished by the use of a curved osteotome followed by heavy curved scissors.
Question: What would you recommend for rehabilitation or reconstruction of this defect?
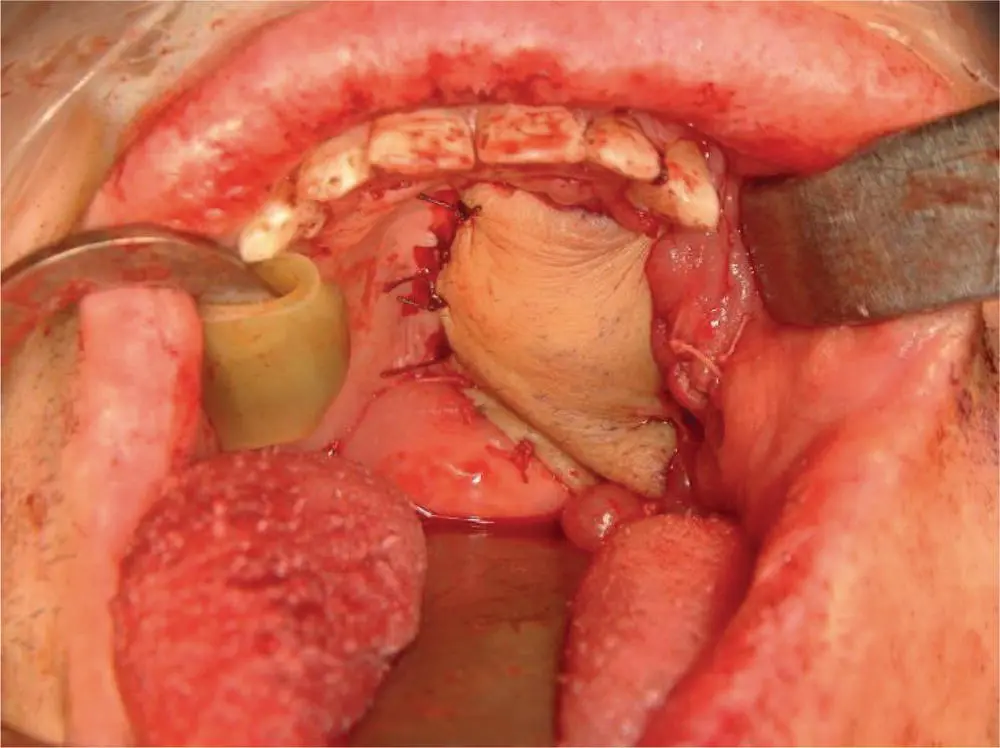
Answer:This patient could be rehabilitated with a dental obturator. The obturator allows for inspection of the resection site as well as for dental rehabilitation. The main disadvantage is the inability to eat without the prosthesis and nasal speech. An alternative method is with a free radial forearm flap, which allows for eating without a prosthesis and normal speech. However, a dental plate with teeth is still required for dental rehabilitation. In this particular case, a free radial forearm flap was used with donor vessels arising from the facial artery (see Figure 6.4).
Final pathology showed adenoid cystic carcinoma, predominantly tubular, 3.5 cm, no bone invasion, but with gross perineural invasion into the greater palatine nerve. All margins are free of tumor.

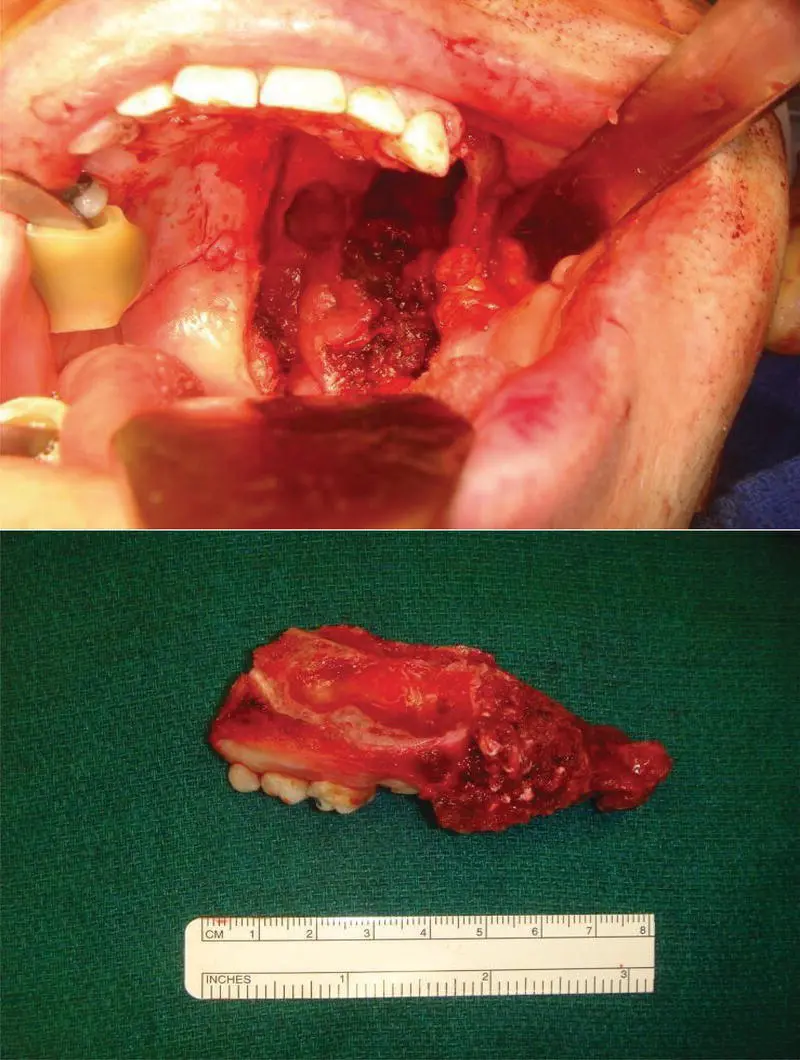
FIGURE 6.3 These intraoperative images show the surgical approach transorally and the resulting maxillectomy defect as well as the associated specimen.
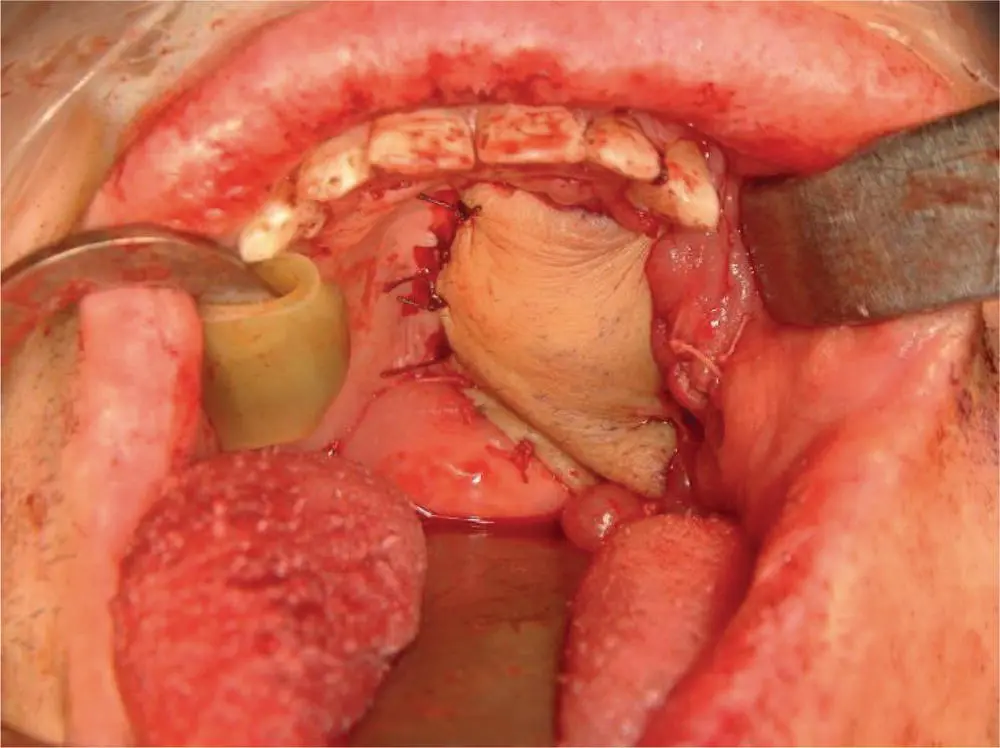
FIGURE 6.4 This intraoperative photo shows the palate defect after reconstruction using a radial forearm free flap. An alternative approach would have been a maxillary obturator given the preservation of the ipsilateral canine tooth and adequate contralateral maxillary dentition.
Question: What would you recommend next?
Answer:Although the tumor is completely excised, the risk of local failure is still significant in adenoid cystic carcinoma. Adjuvant radiotherapy is recommended. Since there are no adverse features (such as lymph node involvement, positive margins), adjuvant chemotherapy or consideration of clinical trials to add chemotherapy to radiotherapy are not appropriate in this case.
Question: What is the expected outcome for this patient?
Answer:Patients with minor salivary cancer tend to have a very good overall survival of 80% and disease‐specific survival of 80–90%. The main predictors of outcome are stage III/IV disease and high‐grade pathology. Female patients have a superior survival compared to male patients. Distant failure is more common and is the main cause of death.
This patient was treated with adjuvant radiation and remains disease‐free at 3 years post‐treatment.
The oral cavity is the most common location for the development of minor salivary gland tumors due to the high concentration of minor salivary gland tissue in this location.
Adenoid cystic carcinoma is the most common minor salivary gland cancer.
For minor salivary gland cancers of the palate, evaluation includes a detailed history, physical exam, a thorough cranial nerve exam, and a biopsy, often with a fine needle aspiration.
For further assessment of palate salivary cancers, both CT and MRI are typically employed to assess for bone erosion and perineural invasion, respectively.
Due to the close association of the mucosa of the hard palate and the underlying bone, infrastructure maxillectomy is often required.
When considering a patient for an infrastructure maxillectomy, it is essential to consider the expected defect and discuss options for rehabilitation. If the use of a maxillary obturator is considered, a preoperative evaluation by a maxillofacial prosthodontist is crucial to get a surgical obturator created.
To successfully retain an obturator, it is necessary to have adequate dentition to stabilize the prosthesis. Retention of the ipsilateral canine tooth typically allows for excellent obturator stability.
In patients where a maxillary obturator is not appropriate or desired, more definitive reconstruction with a regional or free flap is needed.
Multiple Choice Questions
1 In managing a 52‐year‐old female patient with a cT1N0M0 SCC of the right lateral tongue, you offer a right partial glossectomy. Final pathology demonstrates invasive SCC with maximal dimension of 1.5 cm and 6 mm depth of invasion. What would be the most appropriate next step in management of this patient?Close observation of the neck with clinical exam and ultrasound every 3 months.A right‐sided supraomohyoid neck dissection.A right‐sided radical neck dissection.A bilateral supraomohyoid neck dissection.Answer: b. This patient has a pT2 lesion. With a depth of invasion greater than 3 mm, level I evidence shows improved disease control and overall survival when an ipsilateral supraomohyoid neck dissection is performed. Since they are cN0, a radical neck dissection would not be appropriate. Moreover, since it is a lateral tongue cancer, it would not be necessary to do a bilateral dissection.
Читать дальше