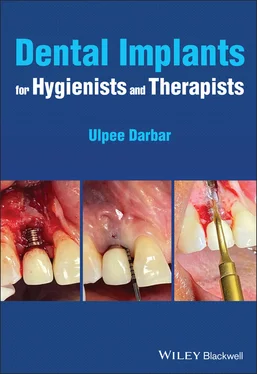
Ulpee R. Darbar - Dental Implants for Hygienists and Therapists
Здесь есть возможность читать онлайн «Ulpee R. Darbar - Dental Implants for Hygienists and Therapists» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Dental Implants for Hygienists and Therapists
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Dental Implants for Hygienists and Therapists: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Dental Implants for Hygienists and Therapists»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Dental Implants for Hygienists and Therapists
Dental Implants for Hygienists and Therapists
Dental Implants for Hygienists and Therapists — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Dental Implants for Hygienists and Therapists», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
4 Chapter 4Figure 4.1 Tooth replacement controls...Figure 4.2 a: Denture wearer showing...Figure 4.3 a, b: Gingival tissue...Figure 4.4 Assessing gingival tissue...Figure 4.5 Anatomy of the gingival tissues...Figure 4.6 Bone/ridge mapping using sectioned casts.Figure 4.7 Cone beam scans showing the radiographic...Figure 4.8 a, b: Conventional diagnostic...Figure 4.9 Virtual diagnostic wax ups showing ...Figure 4.10 Patient journey...Figure 4.11 a–h: Show a patient...Figure 4.12 Patient with hypodontia.
5 Chapter 5Figure 5.1 a: Flapless implant placement...Figure 5.2 Surgical tray showing...Figure 5.3 a–f: Drilling sequence...Figure 5.4 Second-stage surgery...Figure 5.5 Different timings...Figure 5.6 Skull showing the fenestrations...Figure 5.7 Thin gingival...Figure 5.8 a–c: cases showing...Figure 5.9 Principles of guided...Figure 5.10 a–d: Cases...Figure 5.11 Different types...Figure 5.12 Different materials...Figure 5.13 a–c: Immediate...Figure 5.14 Computerised...Figure 5.15 a–c: Ball...Figure 5.16 Fixed...Figure 5.17 Access...Figure 5.18 Resin-based...Figure 5.19 a–c: Minor...Figure 5.20 a, b: Major...Figure 5.21 Impression...Figure 5.22 Encode...Figure 5.23 Locating...
6 Chapter 6Figure 6.1 Shows...Figure 6.2 Probing...Figure 6.3 a: Biologic...Figure 6.4 Peri-implant...Figure 6.5 Factors...Figure 6.6 Peri-implant...Figure 6.7 Peri-implantitis.Figure 6.8 a, b: Incorrect...Figure 6.9 Air polisher:...Figure 6.10 a, b: Topical...Figure 6.11A Resective...Figure 6.11B Regenerative...Figure 6.12 a, b, c:...Figure 6.13 Cumulative...Figure 6.14 Treatment...
7 Chapter 7Figure 7.1Figure 7.2a Healthy...Figure 7.2b Healthy...Figure 7.3 Early signs...Figure 7.4 Shows the presence...Figure 7.5 Showing the probing...Figure 7.6 a, b, c, d: Probing...Figure 7.7a Recession...Figure 7.7b Bone levels...Figure 7.8 a, b, c, d:...Figure 7.9 a, b: Loose...Figure 7.10 a–d:...Figure 7.11 a, b:...Figure 7.12 a, b, c, d, e:...Figure 7.13 Water pick/flosser.
8 Chapter 8Figure 8.1 Members...Figure 8.2 Information...Figure 8.3 Role...Figure 8.4a: Patient...Figure 8.4b: Post...Figure 8.4c: Patient...Figure 8.4d: Patient...Figure 8.4e: Radiographs...
List of Tables
1 Chapter 1 Table 1.1 Progressive Development of Methods... Table 1.2 Some of the Mainstream Dental Implant Systems.
2 Chapter 2 Table 2.1 Factors Affecting Osseointegration.Table 2.2 Different Generations of Implant... Table 2.3a Criteria for Success as Suggested by Albrektsson et al. 1986. Table 2.3b Reported Success Criteria for Dental Implant... Table 2.4 Factors Affecting Implant Success Rates.
3 Chapter 3Table 3.1 Connection Types Associated with Different Implant Systems.
4 Chapter 4Table 4.1 Principles of Treatment Planning for the Implant Patient.Table 4.2 Medical conditions that can affect implant treatment.Table 4.3 Components that should be considered during the Intraoral...
5 Chapter 5Table 5.1 Timelines for Dental Implant Placement.Table 5.2 Barriers Most Commonly Used for Guided Bone Regeneration;Table 5.3 Different Graft Materials Used for Augmentation.
6 Chapter 6Table 6.1 Similarities and Differences between the Tissues...Table 6.2 Different Classification Systems Used for Peri-Implantitis.Table 6.3 Treatment Modalities for Peri-Implant...
7 Chapter 7Table 7.1 Plaque Indices Used for Plaque Assessment...Table 7.2 Clinical Practice Guidelines to Assess Peri-Implant...Table 7.3 Definition of Implant Success and Failure...
8 Chapter 8Table 8.1 Clinical Criteria Used to Describe Success and Failure...
Guide
1 Cover
2 Title page
3 Copyright
4 Table of Contents
5 Glossary
6 Begin Reading
7 Index
8 End User License Agreement
Pages
1 i
2 ii
3 iii
4 iv
5 v
6 vi
7 vii
8 viii
9 ix
10 x
11 1
12 2
13 3
14 4
15 5
16 6
17 7
18 8
19 9
20 10
21 11
22 12
23 13
24 14
25 15
26 16
27 17
28 18
29 19
30 20
31 21
32 22
33 23
34 24
35 25
36 26
37 27
38 28
39 29
40 30
41 31
42 32
43 33
44 34
45 35
46 36
47 37
48 38
49 39
50 40
51 41
52 42
53 43
54 44
55 45
56 46
57 47
58 48
59 49
60 50
61 51
62 52
63 53
64 54
65 55
66 56
67 57
68 58
69 59
70 60
71 61
72 62
73 63
74 64
75 65
76 66
77 67
78 68
79 69
80 70
81 71
82 72
83 73
84 74
85 75
86 76
87 77
88 78
89 79
90 80
91 81
92 82
93 83
94 84
95 85
96 86
97 87
98 88
99 89
100 90
101 91
102 92
103 93
104 94
105 95
106 96
107 97
108 98
109 99
110 100
111 101
112 102
113 103
114 104
115 105
116 106
117 107
118 108
119 109
120 110
121 111
122 112
123 113
124 114
125 115
126 116
127 117
128 118
129 119
130 120
131 121
132 122
133 123
134 124
135 125
136 126
137 127
138 128
139 129
140 130
141 131
142 132
143 133
144 134
145 135
146 136
147 137
148 138
149 139
150 140
151 141
152 142
153 143
154 144
155 145
156 146
157 147
158 148
159 149
160 150
Glossary
Abutment:The component of an implant that interfaces with the implant fixture and the prosthetic entity. Retained with a screw or can be adapted for a prosthesis to be cemented. Made of titanium, alloyed metals, gold; zirconia; ceramic. They can be preformed and come as straight or angled or custom made. Analogue:Replica of the implant fixture or the abutment which is used by the laboratory to make the prosthesis. Abutment driver:Instrument used to connect the abutment to the fixture. Abutment healing cap:A temporary cover used to protect the implant fixture head during the healing period. Abutment–implant interface:The surface of contact between the implant fixture and the abutment. Abutment-level impression:Impression of the abutment taken once the abutment is connected to the implant fixture either directly through conventional impressions or indirectly through an impression coping. Abutment Screw:The screw used to connect the abutment to the implant fixture and has different features depending if it is a single crown or a bridge. It is torqued to the final position. Allogenic bone:Bone from the same species. Alloplastic material:Material of synthetic origin that does not have human or animal origin. Anti-rotation:A feature that prevents rotational movement Barrier membrane:A material used to exclude cells from invading into the defect allowing the preferred cells to grow into the defect. When used technique is called guided bone or tissue regeneration. Membrane can be resorbable or non-resorbable. Made of collagen or synthetic derivatives which are resorbable or titanium or polytetrafluorethylene (PTFE) which are non resorbable. Bicortical stabilisation:Used when both the superior and inferior cortices of bone are used to obtain stability of the implant. Bisphosphonate-related osteonecrosis of the jaw (BRONJ):Also called medication-related necrosis, it is the necrosis of bone related to bisphosphonates. Bone to implant contact:A term used to describe the direct contact of bone to the implant. Bone to implant interface:The line of separation between the living bone and implant fixture surface. CAD-CAM:Computer-aided design computer-aided manufacture used to plan, design and construct implant restorations. It forms part of the digital workflow. Connective tissue attachment:The mechanism by which the connective tissue attaches to the implant. Countersinking:Bone preparation of the crestal aspect using special drivers to allow subcrestal (below the bone) placement of the implant shoulder. Cover screw:Fits over the implant head to protect it when the gum tissue is closed over it and the fixture is submerged. Dental implant:A screw made of titanium that is screwed into the jawbone using specialised and specified techniques to resemble a tooth root. Diagnostic wax up:Procedure in which the teeth are created to match the planned restoration and used in planning and also for construction of a radiographic and surgical guide. Digital workflow:A workflow that uses digital technology to convert analogue structures into a digital format. External connection:The connection that protrudes on top of the implant fixture platform and connects the prosthesis to the fixture. Fixed prosthesis:A prosthesis that is fixed to the implant fixture which the patient cannot remove for cleaning. Fixation screws and tacks:Used to stabilise membranes or block grafts to the underlying bone. Fixture:Endosteal dental implant. Guide drill:The first drill used to open the cortical bone at the implant site during implant surgery. Guided bone regeneration:Technique used to selectively allow bone cells to populate the defect. Healing abutment/cap:Used after the first- or second-stage surgery to connect the implant fixture to the oral cavity. Implant stability:Clinical evaluation of the implant assessing its degree of stability. Implant substructure:The metal framework onto which the crown or prosthesis is connected. Impression coping:A device used to register the position of the dental implant or abutment. Immediate loading:The prosthesis is placed underload at the same time as implant fixture placement. Internal connection:The connection which sits inside the body of the implant fixture and links the implant fixture to the prosthesis. It comes in different configurations. Peri-implant diseases:Include peri-implant mucositis where there is reversible inflammation of the gingival tissues and peri-implantitis where there is irreversible loss of bone with inflammation. Prosthetic screw:Screw used to connect the prosthesis to the abutment. Primary stability:Mechanical stability achieved when the implant fixture is placed. Also knows as the initial stability. Provisional restoration:Temporary restoration placed whilst the tissues are healing. Radiographic marker:A radio-opaque material incorporated into the radiographic guide to show the position. Radiographic stent/guide:Used to direct the position of the tooth in relation to the underlying bone. Worn by the patient when having the radiograph or CT scan. Regeneration:Technique used to reconstitute tissues lost through disease. Surgical guide/template:Used during the surgical implant placement to guide the placement of the implant fixture to be placed in the correct restoratively driven position and angulation. Torque driver:Instrument used to apply the correct level of tightening force (torque) to the screws. Two-stage surgery:When the implant fixture is covered over by the soft tissue and a minor procedure is undertaken to uncover the fixture.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Dental Implants for Hygienists and Therapists»
Представляем Вашему вниманию похожие книги на «Dental Implants for Hygienists and Therapists» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Dental Implants for Hygienists and Therapists» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.