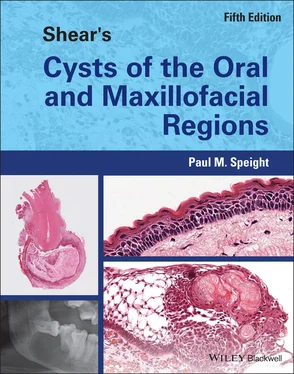
Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions
Здесь есть возможность читать онлайн «Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Shear's Cysts of the Oral and Maxillofacial Regions
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Shear's Cysts of the Oral and Maxillofacial Regions: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Shear's Cysts of the Oral and Maxillofacial Regions»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Shear’s Cysts of the Oral and Maxillofacial Regions
Shear’s Cysts of the Oral and Maxillofacial Regions Fifth Edition
Shear's Cysts of the Oral and Maxillofacial Regions — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Shear's Cysts of the Oral and Maxillofacial Regions», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
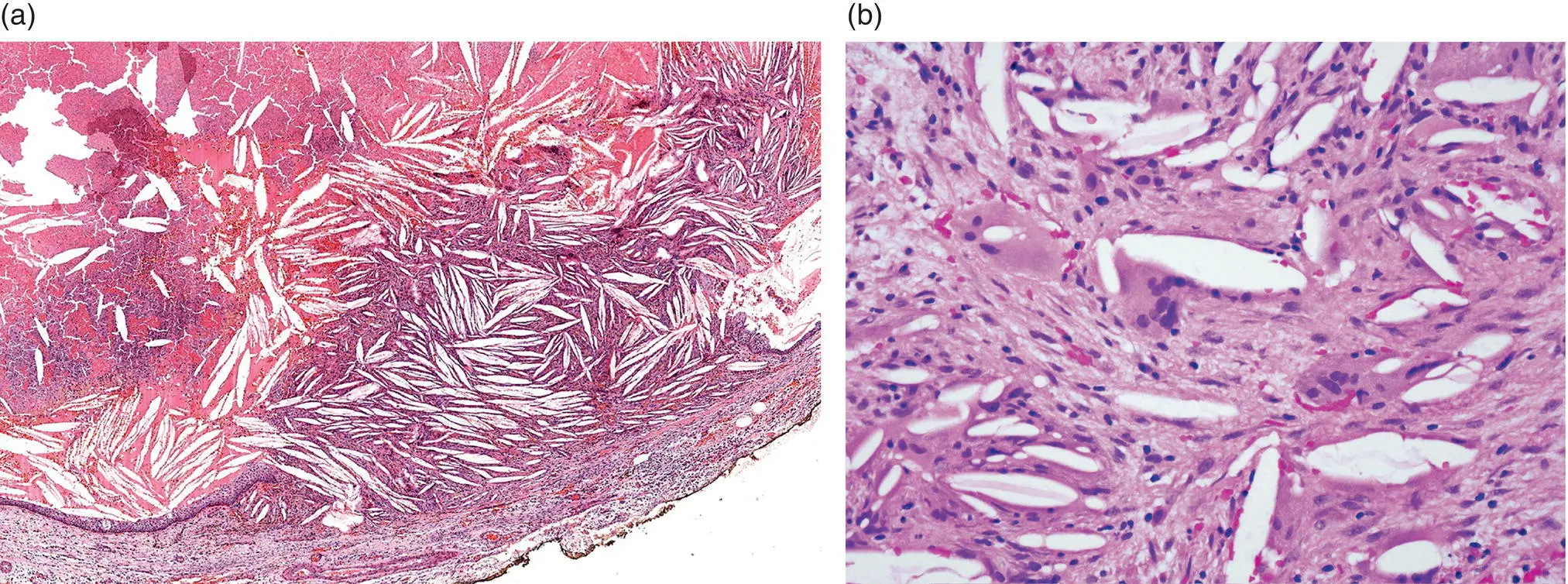
Figure 3.16 Cholesterol clefts in a radicular cyst. (a) An accumulation of cholesterol has formed a nodule that ruptures the cyst lining and protrudes into the lumen. (b) Multinucleate foreign body giant cells on the surface of cholesterol clefts in the wall of a radicular cyst.
Occasionally isolated or scattered clefts may be seen within the cyst wall. High‐power examination shows that each cleft is surrounded by one or more large multinucleated giant cell ( Figure 3.16b), an indication that the crystals are recognised as foreign bodies. The persistence of cholesterol crystals in the tissues and the accumulation of macrophages may be an important cause of persistent chronic inflammation, and is thought to be a major factor in the persistence of non‐healing periapical lesions after endodontic treatment of the offending tooth (Nair 2006 ). Slutzky‐Goldberg et al. (2013 ) compared the incidence of cholesterol in periapical lesions in young and elderly patients, and found that the elderly (over 60 years) had a significantly higher incidence of cholesterol than young (13–21 years) patients. They suggested that this may be associated with increasing serum cholesterol with age, and that it may also be a factor in non‐healing of periapical lesions in older age groups. It is equally likely, however, that the increased frequency in the elderly is associated with the length of time the lesion, and associated chronic inflammation, has been present.
A number of other features are typically seen in radicular cysts, but these are not specific and are also associated with long‐standing chronic inflammation. As noted above (Browne 1971b ), deposition of haemosiderin pigment is common. Browne (1971b ) found haemosiderin in 61.4% of radicular cysts and noted a correlation with cholesterol and also with accumulation of foamy histiocytes. Haemosiderin is often found within histiocytes and Lin et al. (2010 ) found haemosiderin‐laden and foamy histiocytic in 6.0% and 6.8% of radicular cysts, respectively ( Figure 3.17). Buchner and David (1978 ) demonstrated the presence of pigmented cells in 42% of radicular cysts. However, in this study the pigment was not haemosiderin, but was identified as lipofuscin. It was found in association with haemosiderin deposits and cholesterol, and Buchner and David suggested it was also associated with the inflammatory process in the cyst wall. Lipofuscin is pale yellow‐brown in colour, is positive with PAS stain, negative for Perls Prussian blue, and shows a yellow autofluorescence under ultraviolet (UV) light. It can thus be differentiated from haemosiderin, which is dark brown in colour, PAS negative, and positive for Perls Prussian blue.
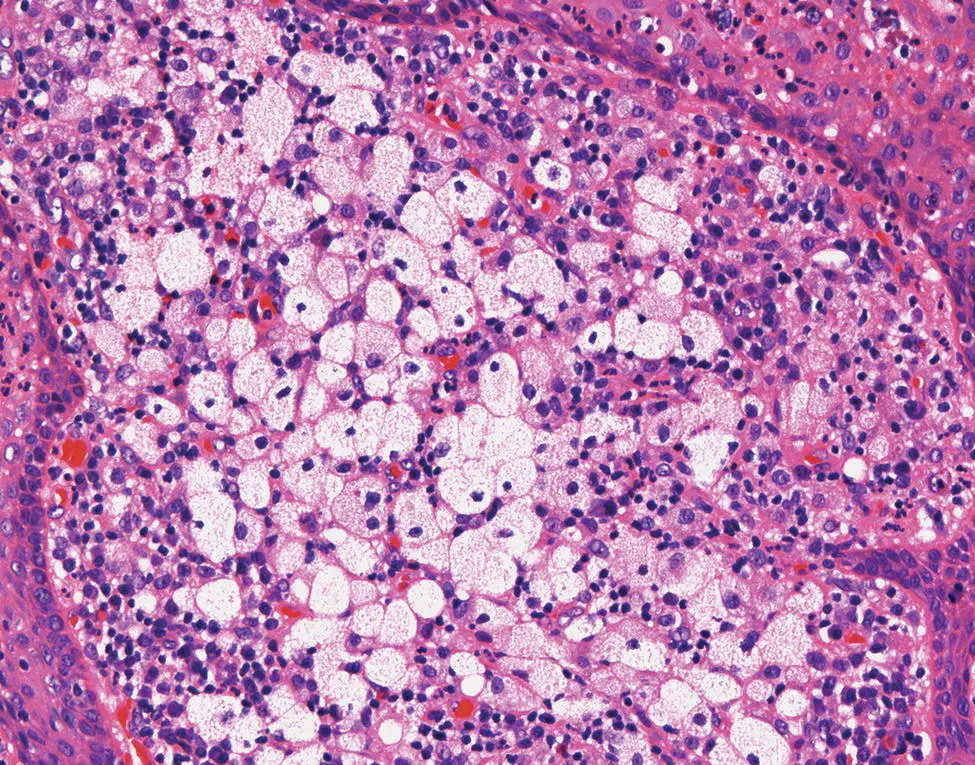
Figure 3.17 A focal accumulation of plump, foamy histiocytes in the wall of a radicular cyst.
As mentioned above, foamy histiocytes are also commonly seen in the walls of radicular cysts ( Figure 3.17). Most often they are scattered or form small focal accumulations in areas of inflammation or are associated with cholesterol clefts. Occasionally, however, sheets of large, pale foamy histiocytes may be encountered, which appear disconcertingly like a xanthogranulomatous reaction.
Residual Cyst
The histopathological features of the residual cyst are similar to those described above for conventional radicular cysts. However, because the cause of the cyst has been removed, residual cysts may progressively become less inflamed so that eventually the cyst wall is composed of uninflamed collagenous fibrous tissue ( Figures 3.11and 3.13). The epithelial lining may be thin and regular and indistinguishable from a developmental cyst, such as a dentigerous cyst or lateral periodontal cyst. In these cases, it is important to establish the relationship of the lesion to the teeth and recall that a residual cyst must arise at a site of an extracted tooth.
Pocket Cyst (Bay Cyst)
With regard to the relationship between the tooth and the cyst lining, there is some evidence that there are two distinct histological types of radicular cyst. Brief mention has already been made of work by Simon (1980 ), who found that in some lesions a cavity may be present that is open to the root canal and is lined by epithelium that is attached to the root apex. Simon examined 35 extracted teeth with apical lesions still attached. Each specimen was decalcified and serial sectioned through the whole block. He found that the majority of lesions (27 cases: 75.2%) were periapical granulomas and that 8 (22.9%) of these contained strands of proliferating epithelium without evidence of cyst formation (e.g. see Figure 3.7). Only 6 cases (17.2%) were diagnosed as cysts. Three cysts showed an epithelial lining that was attached to the root apex, so that the root protruded into the cyst lumen, and the lumen was in direct continuity with the root canal, forming an open ‘pocket’ ( Figure 3.18). Simon (1980 ) called these lesions bay cysts . The remaining cysts showed cavities entirely lined by epithelium with an inflamed fibrous wall, with no epithelial connection to the root apex. These were regarded as true cysts . Simon's data also suggest that cysts only comprise about 17% of periapical lesions and that bay cysts and true cysts have an equal frequency. This has been confirmed in a number of more recent studies that have shown that pocket cysts comprise about 50% of all periapical cysts. The actual frequencies reported have been 50.0% (Simon 1980 ), 38.5% (Nair et al. 1996 ), 56.3% (Ricucci et al. 2006b ), and 52.2% (Ricucci et al. 2020 ).

Figure 3.18 A low‐power view of a pocket cyst. The cyst lining is attached to the apex of the tooth (inset). Although in this plane of section the apical foramen is not visible, it can be seen that the tooth apex protrudes into the cyst lumen.
In the largest study, Nair et al. (1996 ) undertook meticulous serial sectioning of 256 periapical lesions and found that only 39 (15%) were radicular cysts. They also confirmed Simon's observations and showed that of the 39 cysts, 24 (61.5%) were true cysts and 15 (38.5%) were pocket cysts. In further detailed examination of these lesions, Nair (1998 , 2003 ) showed that in pocket cysts the epithelium was attached at the root apex, so that the lumen formed an extension of the root canal, and the intact epithelium acted as a barrier to seal off the contents of the infected root canal from the adjacent tissues ( Figure 3.18). The cyst grows through accumulation of debris and necrotic tissue in the thus‐formed ‘bay’ or ‘pocket’. Simon (1980 ) and Nair (1998 , 2003 ) attached considerable clinical significance to the distinction of the two cyst types and suggested that pocket cysts were likely to heal after tooth extraction or endodontic treatment, whereas a true cyst may be self‐sustaining and can persist after treatment. From his data, Nair (1998 ) suggested that apical true cysts only account for about 10% of all periapical lesions, and this may explain the frequency of about 10% of persistent periapical lesions after conventional root canal treatment, and the low prevalence of residual cysts. Ricucci and Bergonholtz (2004 ) consider that the pocket cyst may be problematic for the endodontist, because the cyst fluid may be under pressure and may continuously wet the root canal, making instrumentation and filling difficult.
Читать дальшеИнтервал:
Закладка:
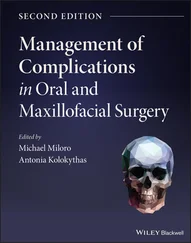
Похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions»
Представляем Вашему вниманию похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Shear's Cysts of the Oral and Maxillofacial Regions» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.