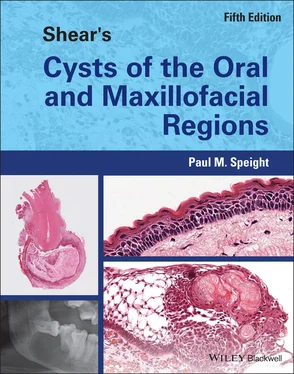
Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions
Здесь есть возможность читать онлайн «Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Shear's Cysts of the Oral and Maxillofacial Regions
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Shear's Cysts of the Oral and Maxillofacial Regions: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Shear's Cysts of the Oral and Maxillofacial Regions»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Shear’s Cysts of the Oral and Maxillofacial Regions
Shear’s Cysts of the Oral and Maxillofacial Regions Fifth Edition
Shear's Cysts of the Oral and Maxillofacial Regions — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Shear's Cysts of the Oral and Maxillofacial Regions», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Box 3.4 Histopathology: Key Features
The cyst is lined by proliferating non‐keratinised stratified squamous epithelium
In long‐standing and residual cysts, the epithelium may become thin and regular
The cyst wall is composed of inflamed fibrous and granulation tissue
Cholesterol clefts and deposits of haemosiderin are often seen
Hyaline bodies are characteristic, but only seen in about 10% of lesions
Other features include mucous cells, cilia, focal keratinisation, and accumulation of foamy histiocytes
More recently, however, it has been suggested that true cysts and pocket cysts do not differ in any clinically significant way, and that the management can be the same. Ricucci et al. (2020 ) undertook a detailed clinicopathological analysis of 11 true cysts and 12 pocket cysts and found no significant differences in any of the clinical or histological features studied, including signs and symptoms, sex, location, size, or degree of acute inflammation. They also examined the presence of bacteria in the root canal or the cyst lumen and found no differences. The authors concluded that there are no clinically important differences between the two cyst types and that there is no real need to draw a diagnostic distinction between true cysts and pocket (bay) cysts. Furthermore, they also found that both pocket cysts and true cysts were infected, and suggested that there is little evidence for the idea that true cysts may be self‐sustainable independent of the infected root canal.
Malignant Change in Radicular Cysts
Primary intraosseous squamous cell carcinoma is defined as a central lesion in the jaw bones, which cannot be categorised as any other type of carcinoma (Koutlas and Sloan 2022 ). To establish the diagnosis, an oral lesion that has invaded the jaws, or metastatic lesions to the jaw bones, must be excluded. Intraosseous carcinomas are derived from odontogenic epithelium and may arise de novo , with no identifiable precursor lesion, or may be preceded by an odontogenic cyst or a benign odontogenic tumour. In a review of the world literature, Thomas et al. (2001 ) were only able to identify 35 cases of de novo lesions, suggesting that the majority of intraosseous squamous carcinomas arise in a pre‐existing lesion and most probably arise in odontogenic cysts. Eversole et al. (1975 ) reviewed series of cases of central squamous cell carcinoma and found that 75% were associated with a cyst lining. In a detailed review of the literature, Gardner (1969 ) examined the evidence presented with each of 63 cases reported during the period 1889–1967 and concluded that 25 (39.7%) fulfilled the criteria for an origin from odontogenic cyst.
Bodner et al. (2011 ) reviewed 116 cases of primary intraosseous squamous cell carcinomas that had arisen in odontogenic cysts. Of these, 70 cases (60.3%) were associated with radicular or residual cysts, 19 (16.4%) with dentigerous cysts, and 16 (13.8%) with an odontogenic keratocyst. Only 1 lesion was found to be associated with a lateral periodontal cyst and 10 could not be classified. The majority of cases (92, 79.3%) were found in the mandible and there was a male : female ratio of 2 : 1.
Before the diagnosis of carcinoma arising from a cyst lining can be established, a number of alternative possibilities must be excluded (Bodner et al. 2011 ; Woolgar et al. 2013 ; Koutlas and Sloan 2021 ). It is possible that a benign cyst and the carcinoma may have developed independently adjacent to one another and ultimately fused in some parts. Careful questioning of the patient and clinical examination are necessary to exclude the possibility that the neoplasm arose primarily from the oral mucosa, or that it is a metastatic deposit in the jaw. A further possibility to be considered is that the lesion was initially an epithelial neoplasm that underwent secondary cystic change. To be certain of the diagnosis, histological evidence of frank squamous cell carcinoma directly in transition from a typical odontogenic cyst lining is regarded as the gold standard diagnostic criterion, but in some cases the malignancy may have overgrown and effaced the precursor lesion. It is also important not to overinterpret an inflamed or proliferating cyst lining as malignant. On occasions, the arcading epithelium of a radicular cyst may give a pseudoepitheliomatous appearance and islands of odontogenic epithelium in the wall are not uncommon. Attention to the cytology of the islands is helpful. Often the epithelium is bland and resembles squamous odontogenic tumour rather than the atypical epithelium of malignancy (Parmar et al. 2011 ; Chrcanovic and Gomez 2018a ).
Despite the undoubted examples that occur from time to time, the frequency of neoplastic change is exceptionally rare in relation to the large numbers of cysts that are seen. There is no evidence, however, that cyst epithelium is at particular risk and there is therefore no justification for regarding cysts as pre‐cancerous lesions. The pathogenesis of malignant change is not known, but some have speculated that it is induced by the long‐standing chronic inflammation (Bodner et al. 2011 ; Jain et al. 2013 ). This would explain the higher frequency of malignant change in radicular cysts, and is in keeping with the now well‐established association between carcinogenesis and inflammation (Crusz and Balkwill 2015 ).
Treatment
Radicular cysts may be removed by conservative surgery involving simple curettage of the lesion. Often this is carried out by an apicectomy procedure involving removal of the cyst and the root apex and sealing of the apical portion of the root canal. Occasionally the offending tooth may be removed, but if the cyst is not curetted, then a residual cyst may arise.
Many periapical radiolucencies are treated non‐surgically by endodontic procedures that remove the necrotic pulp and disinfect and seal the root canal. In this way, about 95% or more of apical lesions heal or do not progress. In this case, however, the lesion is not removed for histological examination and, as discussed above, the majority will be periapical granulomas. In this respect, the lesion heals because the causative root canal infection has been removed and it is not necessary to make any distinction between periapical granulomas and cysts, nor between true cysts and pocket cysts (Ricucci et al. 2020 ).
Useful analyses or reviews on the non‐surgical treatment of periapical lesions have been presented by Natkin et al. (1984 ), Nair (2003 , 2004 , 2006 ), Santos‐Junior et al. (2019 ), and Ricucci et al. (2020 ), and in systematic reviews by Sathorn et al. (2005 ), Torabinejad et al. (2005 ), and Glynis et al. (2021 ).
4 Inflammatory Collateral Cysts
CHAPTER MENU
Classification and Terminology of Inflammatory Collateral Cysts
Clinical Features Frequency Age Sex Site Clinical Presentation
Radiological Features Radiological Differential Diagnosis
Pathogenesis Relationship of the Paradental Cyst to the Dentigerous Cyst
Histopathology
Treatment
Inflammatory collateral cysts are cysts of inflammatory origin that are found towards the buccal aspect of the roots of partially or recently erupted teeth. They arise as a result of inflammation in the pericoronal tissues, but the pathogenesis and the epithelium of origin remain uncertain. Although it is possible for a collateral cyst to arise on any erupting tooth, the vast majority are associated with mandibular molars, with about 60% on third molars and most of the remainder seen on the buccal aspect of first or second molars. Thus, two main types of inflammatory collateral cyst are recognised: the paradental cyst , found predominantly on mandibular third molars, and the mandibular buccal bifurcation cyst , found on first or second molars (Speight and Soluk Tekkeşin 2022b ). In some respects the collateral cysts remain controversial, since it is clear that in some quarters their very existence is questioned. There are a number of papers reporting lesions associated with impacted third molars that do not include a single case of paradental cyst (Curran et al. 2002 ; Stathopoulos et al. 2011 ), while other series of pericoronal lesions on mandibular third molars have suggested that more than 50% may be paradental cysts (Costa et al. 2014 ). One reason for these discrepancies may be the very nature of the cyst itself. The lesion presents as a ballooning of the pericoronal tissues to form a pocket (Ackermann et al. 1987 ; Slater 2003 ) that some may not regard as a true cyst, while others regard it as a simple variant of a dentigerous cyst. Nevertheless, the clinical and radiological features are those of a cystic lesion and the inflammatory collateral cysts are widely accepted as an entity and are included in the World Health Organization (WHO) classification of jaw cysts (WHO 2022a ; Speight and Soluk Tekkeşin 2022b ).
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions»
Представляем Вашему вниманию похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Shear's Cysts of the Oral and Maxillofacial Regions» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.