a receiver of electrons under anaerobic conditions, so forms toxic metabolites that damage bacterial DNA;
also active against some species of protozoa, including Giardia, Entamoeba histolytica and Trichomonas vaginalis;
absorbed orally and can be administered parenterally;
widely distributed in the tissues, crossing the blood–brain barrier and penetrating into abscesses;
metabolized in the liver and excreted in the urine;
well‐tolerated, except that it cannot be taken with alcohol.
Tetracyclines act by inhibition of protein synthesis by locking tRNA to the septal site of mRNA.
They are active against many Gram‐positive and some Gram‐negative pathogens, Chlamydia, Mycoplasma, Rickettsia and treponemes, Plasmodium and Entamoeba histolytica.
Doxycycline is absorbed orally, has a long half‐life and is widely distributed; adequate therapeutic levels may be obtained by a once‐daily dosage.
The newer tetracyclines such as tigecycline are used to treat multi‐resistant Gram‐negative infections.
Sulphonamides and trimethoprim
Sulphonamides and trimethoprim act by inhibiting the synthesis of tetrahydrofolate. They are used in combination in the treatment of bacterial infections and also have an important role in the management of Pneumocystis jiroveci and protozoan infections including malaria. Sulphonamides can be given intravenously and are well‐absorbed when given orally. They are widely distributed in the tissues and cross the blood–brain barrier. They are metabolized in the liver and excreted via the kidney. Trimethoprim may be used int het treatment of sensitive UTIs.
8 Antimicrobial use and stewardship
A holistic approach in antibiotic therapy
Antibiotics alone are not the solution to an infection problem. The patient must be managed in their personal context. Shock, which often accompanies severe sepsis, must be addressed to ensure good tissue perfusion and avoid renal failure. Thus, it is essential to address fluid balance as soon as possible.
Antibiotics alone are unlikely to sterilize an abdominal abscess and surgical intervention to drain the lesion is almost always required. The timing of this intervention may depend on controlling infection, and then resuscitation so that the patient can have the abscess drained.
Patients in the community usually require treatment with oral antibiotics. Where parenteral therapy is absolutely required e.g., treatment of osteomyelitis, it may be necessary to refer patients to out‐patient parenteral antibiotic therapy services (OPAT) so that they can go home when infection is adequately controlled.
Antibiotics are not the only drugs that patients have to take. The aging population of patients have multi‐morbidity, so the possibility for drug–drug interaction is increasing. Careful consideration of concomitant medication is required. In addition to medically prescribed drugs, patients may take over the counter drugs that can impact antibiotics. For example, hepatotoxicity from anti‐tuberculosis drugs can be worsened by paracetamol or alcohol use.
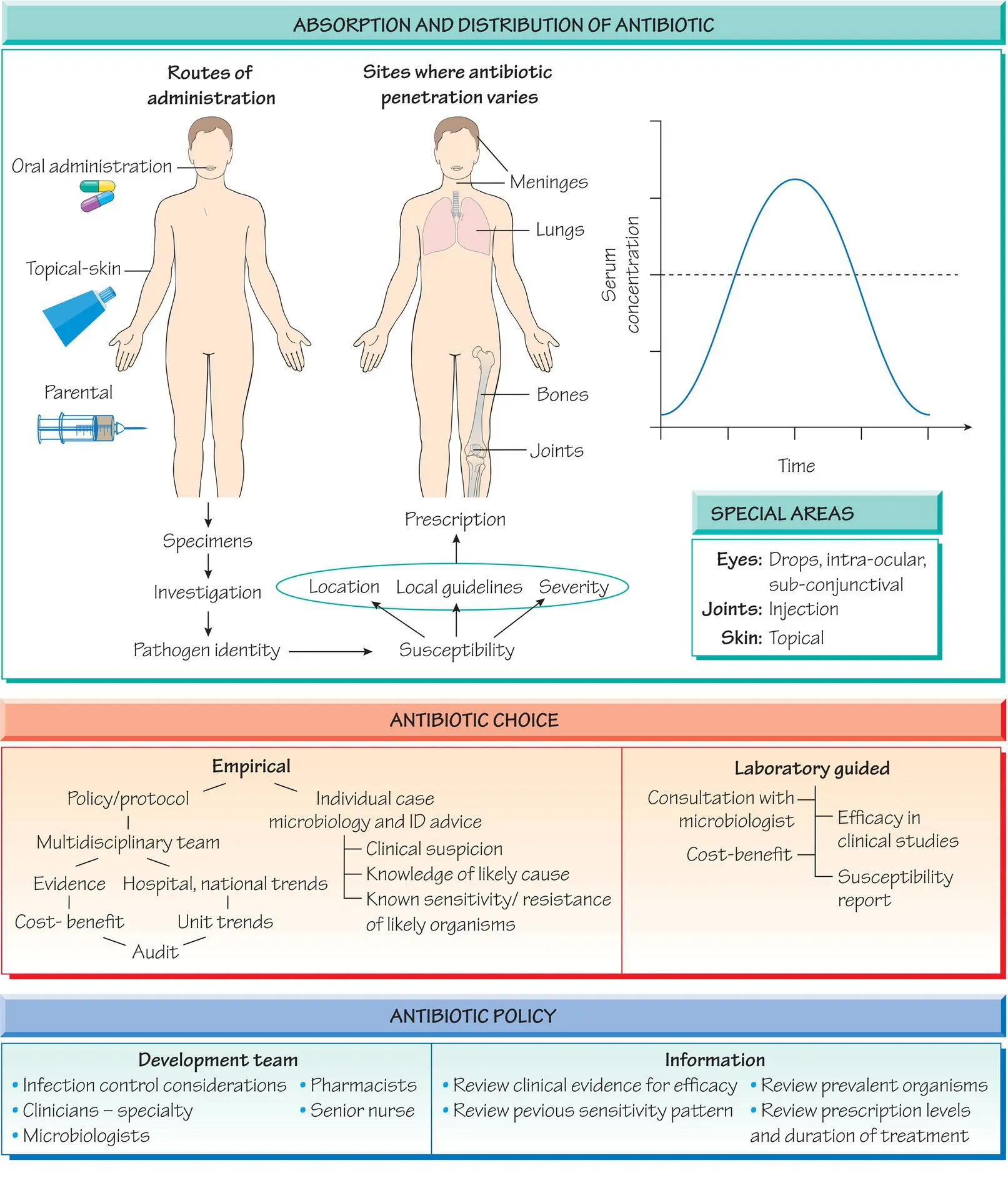
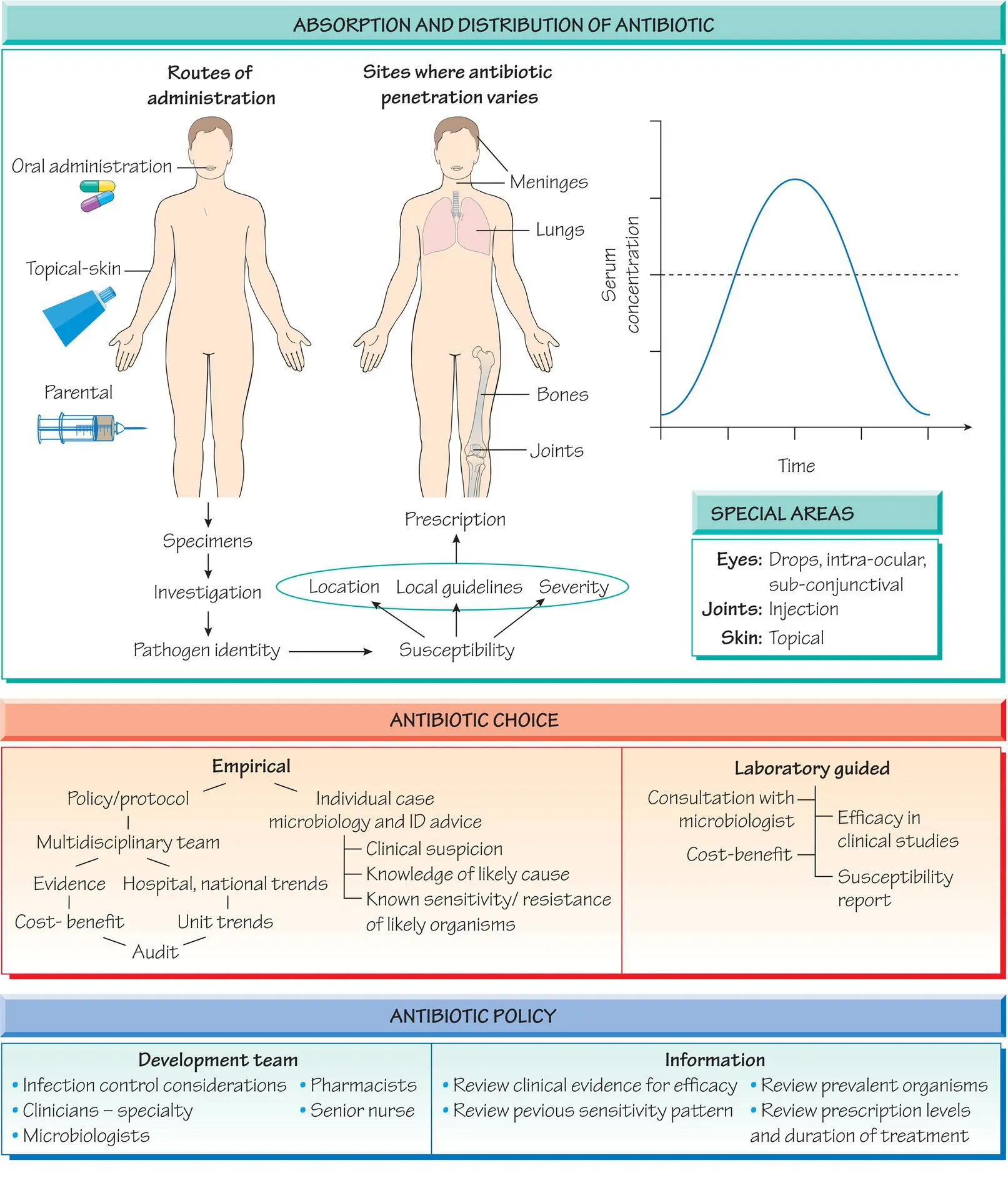
Antibiotic prescribing policies
Hospitals and care groups should have an agreed antibiotic policy. It should indicate the approach to management of infections of different severity and guide prescribers, pointing them to the best therapies for a given condition. By directing choices, it may help unnecessary use, thus reducing the risk of C. difficile enterocolitis previously associated with quinolone and cephalosporins. Policies may reserve antibiotics to infection specialists to ensure that investigation and treatment is indicated. For example, anti‐tuberculosis drugs may be reserved to respiratory and infection specialists so that it is managed by experts, reported to public health agencies, and community follow‐up put in place. Policies also allow antibiotic choices to be changed regularly in response to changes in the resistance profile and to reduce the accumulation of resistance determinants.
The factors that drive antibiotic choice include:
Organism: identification of the organism predicts the natural history of the infection, thereby allowing treatment optimization. Different species have recognized patterns of susceptibility e.g., S. aureus often possesses a beta‐lactamases making it resistant to penicillin but susceptible to flucloxacillin or cephalosporins. A minority are resistant to meticillin.
Susceptibility pattern: Streptococcus pyogenes is invariably susceptible to penicillin, but other organisms such as Acinetobacter and Pseudomonas are often multi‐drug resistant, so antibiotics should be chosen with care to cover the usual resistance pattern until the results of drug susceptibility tests are available.
Infection site: sufficient concentrations of antimicrobial may be difficult to achieve in some sites such as abscesses, bone, the CSF or areas with poor blood supply and some sites with low pH inhibit certain antibiotics (e.g., aminoglycosides).
Severity of infection: severe infections require antibiotics to be given by the parenteral route.
History of allergy: a previous allergic response may limit the choice of antibiotic.
Likelihood of unwanted effects: Some patients are especially vulnerable to complications. For example, aminoglycosides should be used with care in patients with pre‐existing renal disease.
Antibiotics are usually taken orally in mild infections, but intravenous therapy is usually required in severe infections, such as septicaemia, to ensure adequate antibiotic concentrations are achieved. Intravenous therapy may also be required for patients unable to tolerate oral therapy. Topical administration is suitable for skin infections where high concentrations can be achieved. More rarely, antibiotics are given per rectum (e.g. metronidazole for surgical prophylaxis) or intravaginally as pessaries. Children require palatable liquid formulations to maximize adherence.
Picking an antibiotic can be hard as patients do not present with ‘ S. aureus ’ infection, but a disease syndrome. To overcome that problem physicians can:
follow the local antibiotic treatment guidelines or contact the infection specialist for advice;
use rapid diagnostics that may indicate, for example, the causative organism or resistance pattern;
list the potential pathogens in order of likelihood;
list the susceptibilities of the organisms likely to be present bearing in mind local epidemiology (knowledge of ongoing outbreaks);
bear in mind the susceptibility pattern of pathogens in the local environment and the travel history of the patient;
determine the route of administration based on severity and patient circumstance (e.g., outpatient);
take factors such as renal function and concomitant medications into account;
consider the impact of the infection site on the pharmacokinetics, e.g. crossing the blood–brain barrier in meningitis;
consider the duration, as treatment after cure risks adverse events for no benefit and supports the emergence of resistance.
9 Emergence and detection of resistance
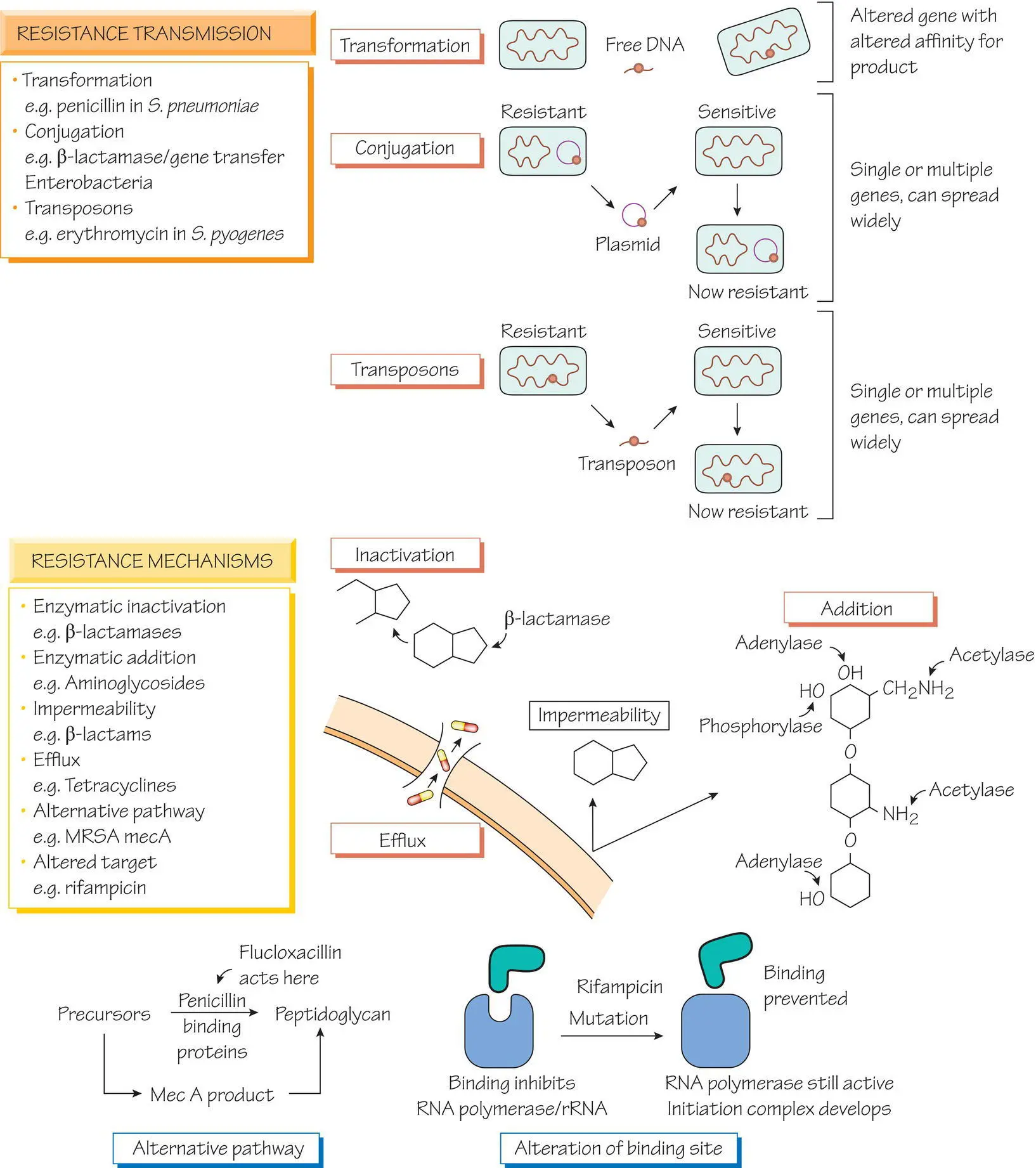
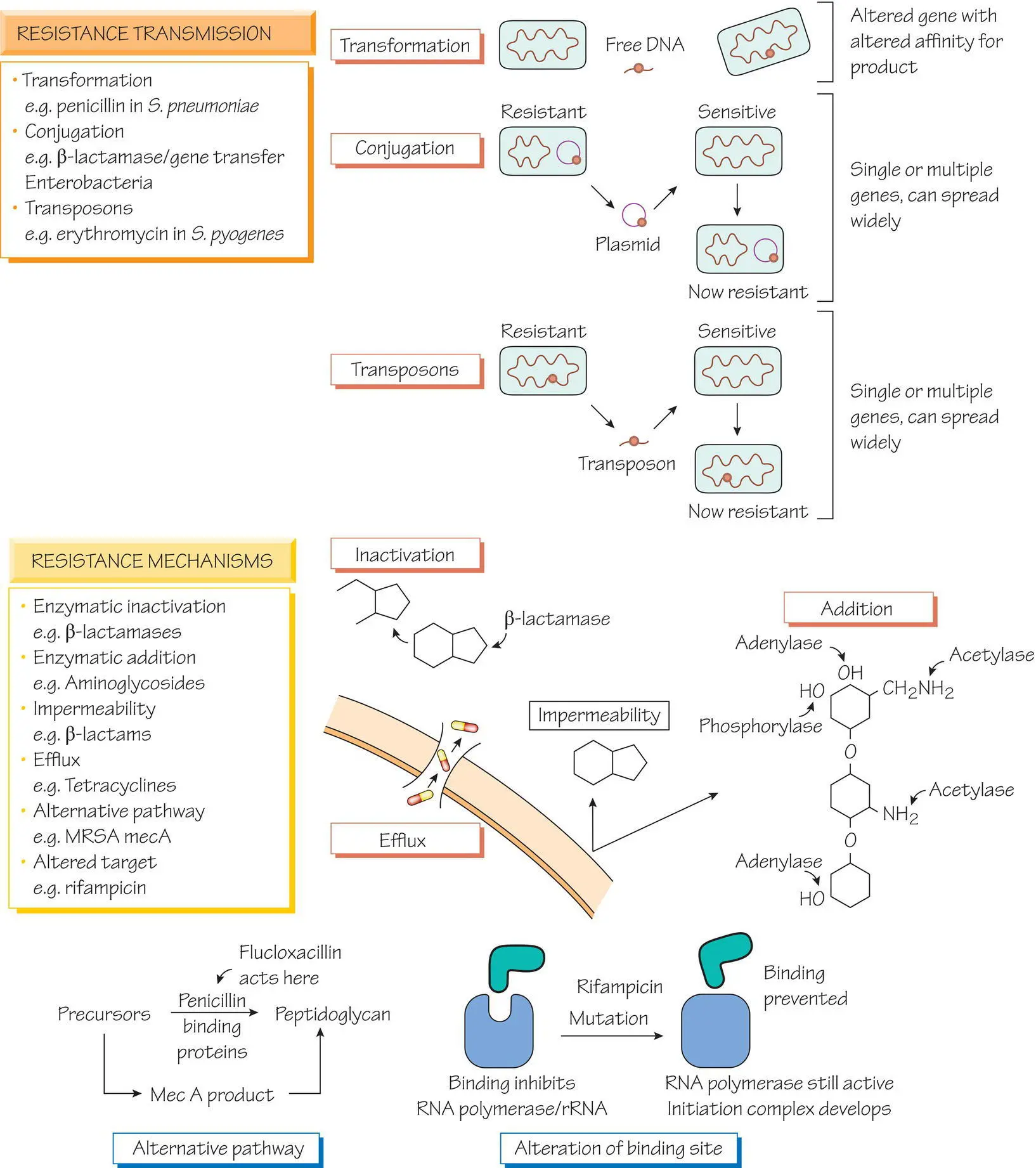
Resistance occurs when a previously susceptible organism is no longer inhibited by an antibiotic at a concentration that can be safely achieved in clinical practice. Resistance can develop quickly because:
Читать дальше