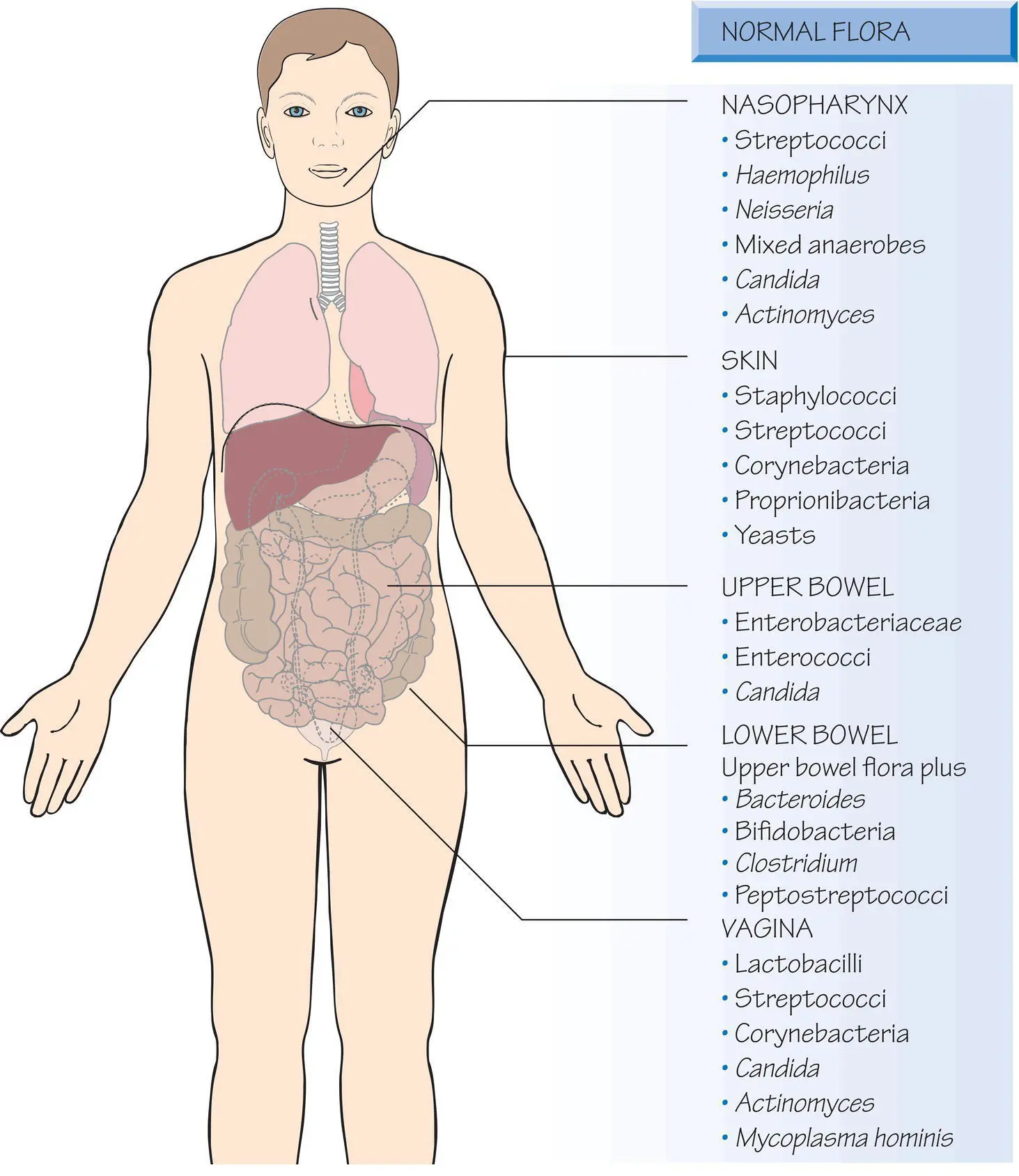
3 The ‘normal’ flora in health and disease
The innate immune system is a natural barrier to infection that can be overcome as a result of organism pathogenicity ( Chapter 4), trauma or medical intervention. It is complemented by the normal flora that acts to compete with invading pathogenic organisms.
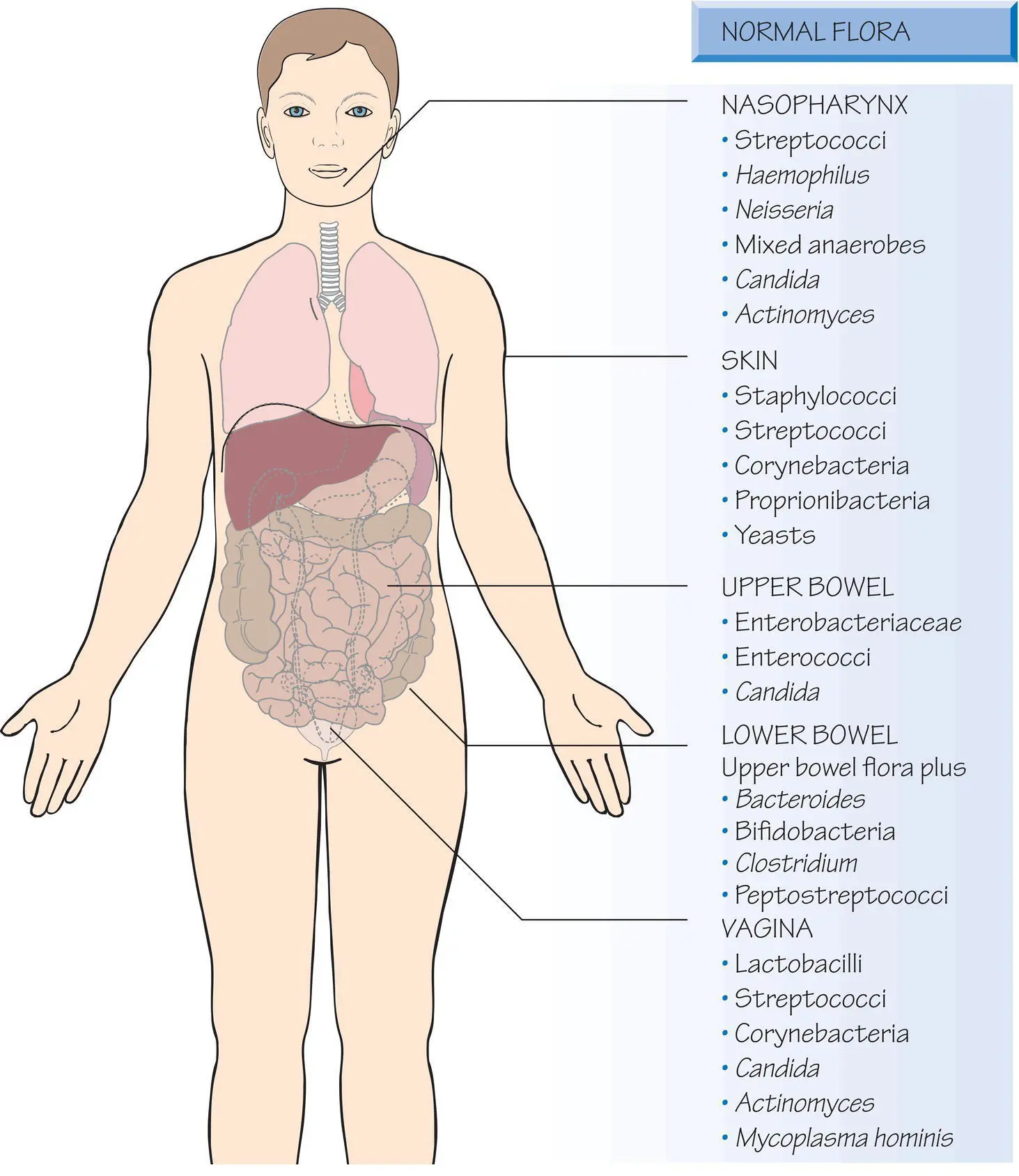
The body is colonized by a wide range of species known as the normal flora that outnumber human cells in the body. The normal flora provides protection by competing with pathogens for colonization sites and producing antibiotic substances (bacteriocins) that suppress other bacteria. Anaerobic bacteria produce toxic metabolic products and free fatty acids that inhibit other organisms. In the female genital tract lactobacilli produce lactic acid that lowers the pH, so preventing colonization by pathogens.
Antibiotics can kill normal flora allowing colonization and subsequent infection by naturally resistant organisms, such as Candida albicans or carbapenemase‐producing Enterobacteriaceae. Hospital patients and especially those in high dependency areas are at particular risk due to frequent antibiotic prescription and their underlying disease. The infective dose of primary pathogens, e.g. Salmonella typhi , is lowered by concomitant antibiotic use. Antibiotics may upset the balance between organisms in the gut allowing one to proliferate disproportionately. Clostridium difficile carrying natural resistant determinants can overgrow and produce severe diarrhoeal disease and spread widely in hospitals and elderly care facilities (see Chapter 24).
Physical and chemical barriers
The skinis a physical barrier; secreted sebum and fatty acids inhibit bacterial growth. Many pathogens can penetrate the skin by the bite of a vector (e.g. Aedes aegypti that transmits dengue) or by invasion through intact skin (e.g. Leptospira and Treponema ). Some organisms colonize mucosal surfaces and invade by this route (e.g. Streptococcus pneumoniae into the lungs and sinuses).
Mechanisms and consequences of deficiency
| Component |
Compromise |
Consequence |
| Normal flora |
| Pharynx |
Antibiotics |
Oral Candidiasis |
| Intestine |
Antibiotics |
Pseudomembranous colitis; colonization with antibiotic‐resistant organisms |
| Vagina |
Antibiotics |
Vaginal Candidiasis |
| Skin |
Burns, vectors |
Cutaneous bacterial infection, systemic viral, bacterial, protozoal and metazoal infection |
| Turbinates and mucociliary clearance |
Kartagener’s syndrome, cystic fibrosis, bronchiectasis |
Chronic bronchial sepsis |
| Lysozyme in tears |
Sjögren’s syndrome |
Ocular infection |
| Urinary flushing |
Obstruction |
Recurrent urinary infection |
| Phagocytes, neutrophils, macrophages |
Congenital, iatrogenic, infective |
Chronic pyogenic infection, increased susceptibility to bacterial infection |
| Complement |
Congenital deficiency |
Susceptibility to capsulated bacterial infection, especially Neisseria spp. See Chapter 66. |
If skin integrity is broken by intravenous cannulation or by medical or non‐medical injection, blood‐borne viruses, such as hepatitis B or the human immunodeficiency virus (HIV) may gain access. Eczema or burns, permit colonization and invasion by pathogens (e.g. Streptococcus pyogenes or Pseudomonas aeruginosa ).
Mucociliary clearance mechanismsprotect the respiratory tract. Air is humidified and warmed as it is drawn in by passing over the turbinate bones and through the nasal sinuses. Any particles settle on the sticky mucus of the respiratory epithelium and are transported by the cilial ‘conveyor belt’ to the oropharynx where they are swallowed. As a result, only particles with a diameter of less than 5 μm reach the alveoli, so the respiratory tract is dynamically sterile below the carina.
In chronic obstructive pulmonary disease and bronchiectasis, excessive mucus or anatomical derangement means that bacteria are not cleared and patients suffer recurrent respiratory infections with organisms such as Haemophilus or Pseudomonas . The thickened mucus associated with cystic fibrosis creates a similar problem.
Intubation in intensive care bypasses this barrier and allows a direct path to the lungs, facilitating ventilator associated pneumonia. Tobacco smoking, air pollution and cooking on open fires can paralyse the cilia, making those individuals exposed, especially children, to be at increased risk of both infection and severe disease.
Secreted antibacterial compoundsinclude mucus, which contains polysaccharides of similar antigenic structure to the underlying mucosal surface; organisms bind to the mucus and are removed. Other antibacterial compounds secreted by the body include lysozyme in tears, which degrades Gram‐positive bacterial peptidoglycan; lactoferrin in breast milk, which binds iron and inhibits bacterial growth; and lactoperoxidase, a leucocyte enzyme, which produces superoxide radicals that are toxic to microorganisms.
Gastric acidkills ingested organisms and acid suppression increases the risk of intestinal infection. This is a particular risk in intensive care units and is compounded by the use of antibiotics.
Urinary flushingprotects the urinary tract, with the flushing action of urinary flow keeping the tract sterile, except near the urethral meatus. Obstruction by stones, tumours, benign prostatic hypertrophy or scarring of the urethra or bladder may cause a reduction of urinary flow and stasis, increasing the risk of subsequent bacterial urinary infection. Urinary catheterization results in chronic colonization of the bladder, which may be followed by sepsis (see Chapter 60). The chronic colonization can make confirming the diagnosis of infection challenging.
Antibiotic treatmentAntibiotic administration can change the bacterial flora, especially mucosal anaerobes making the patient more vulnerable to colonization with potentially pathogenic or antibiotic resistant organisms. Once established these replace the normal flora and may go on to cause infection at a later time.
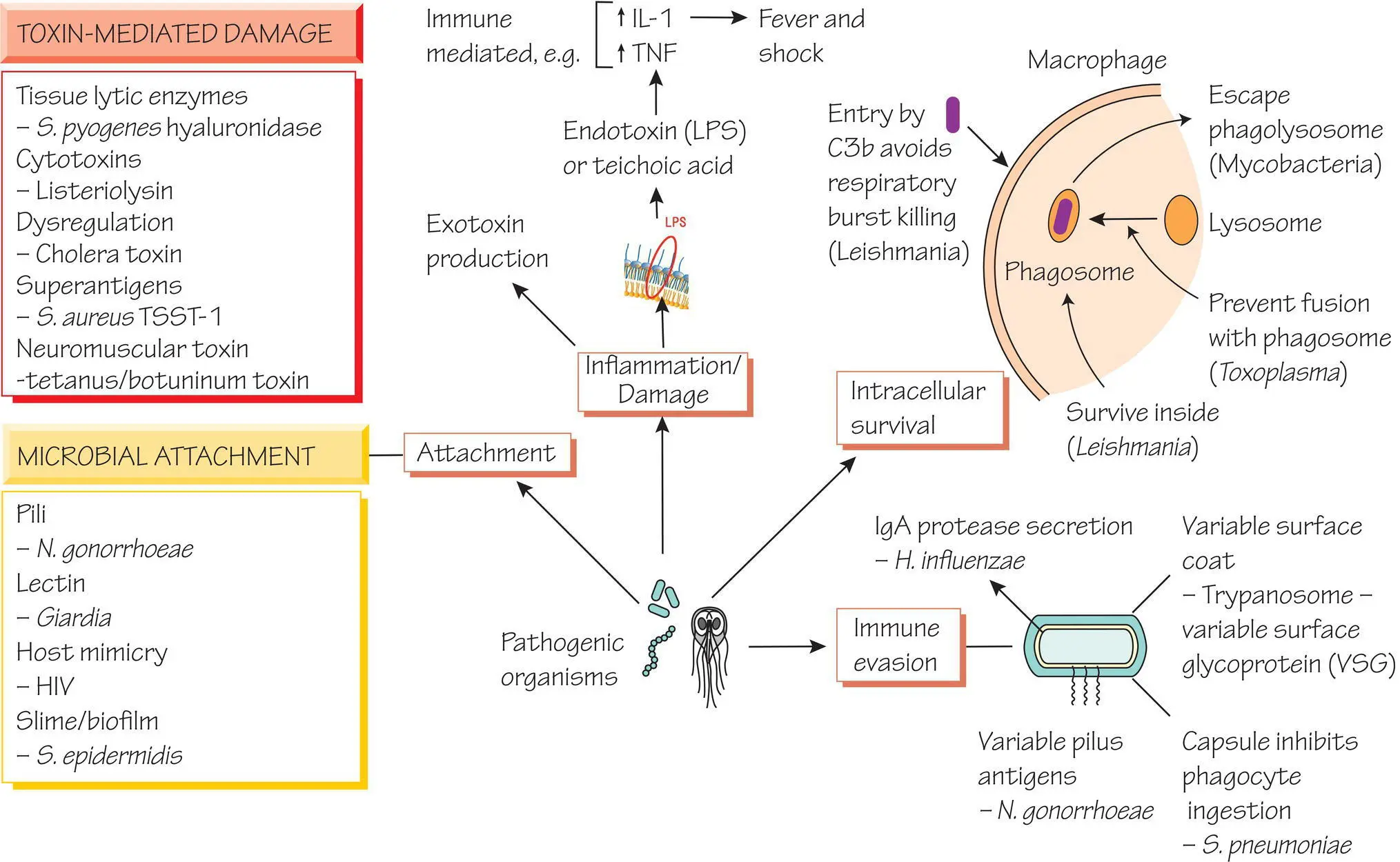
4 Pathogenicity and pathogenesis of infectious disease
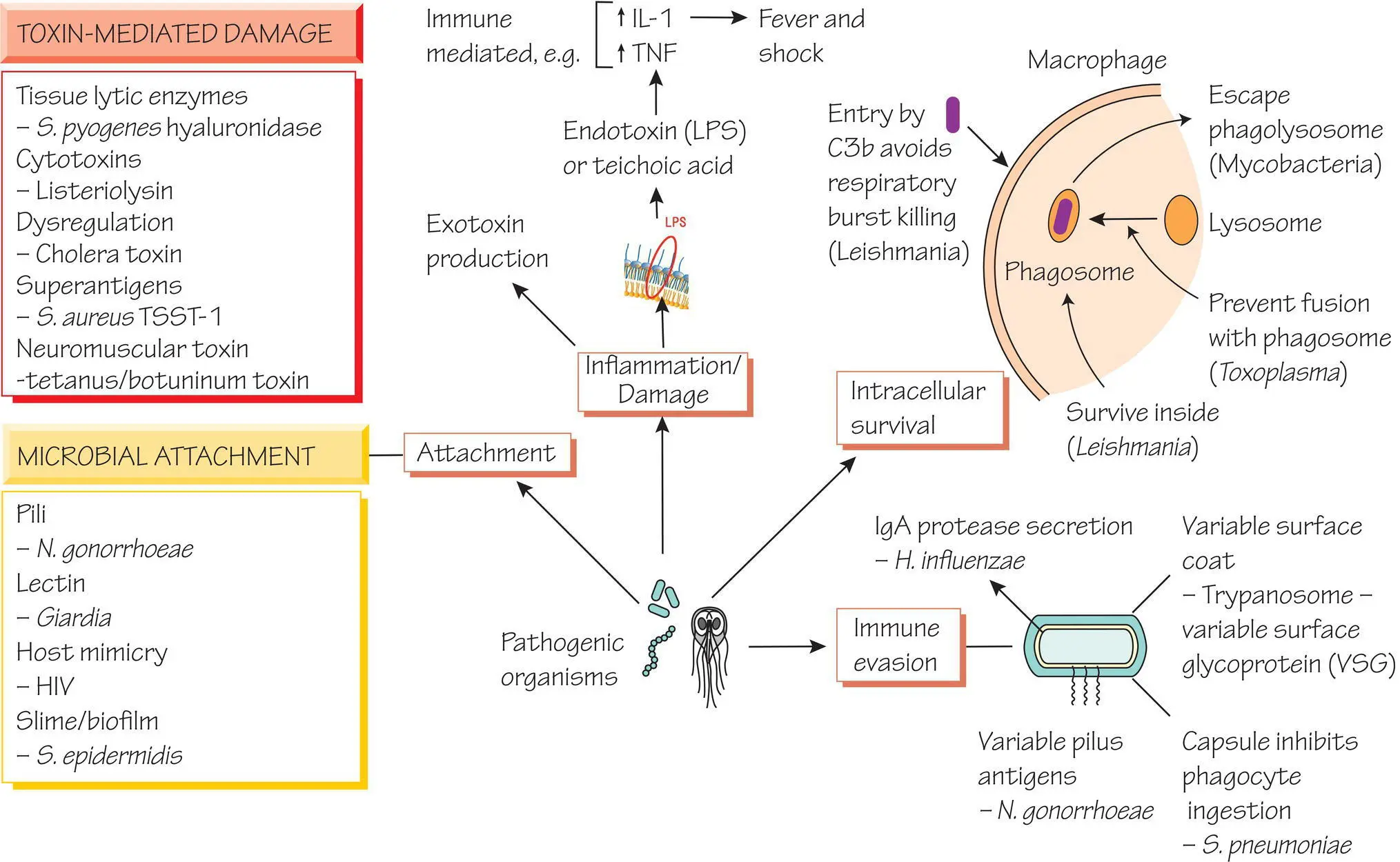
Humans encounter bacteria, viruses and parasites that do not cause disease. An infection occurs when an organism invades the body and causes ill‐health.
| Term |
Definition |
| Pathogen |
An organism capable of causing disease |
| Commensal |
An organism that is part of the normal flora |
| Pathogenicity |
The capacity to cause disease |
| Virulence |
The capacity to cause severe disease |
The capsule of Streptococcus pneumoniae is a pathogenicity determinant because acapsulate strains do not usually cause disease, but some capsular types cause more serious disease, i.e. they are more virulent ( Chapter 19). The term parasite is often used to describe protozoan and metazoan organisms (see Chapters 49– 52), but this is confusing as these organisms may be either pathogens or commensals.
Читать дальше