It is important to ensure that sufficient antibiotic reaches the site of infection. This means it is important to understand where the organisms are and how the antibiotic is absorbed and distributed in the body. For example, for effective treatment of meningitis it is essential that the antibiotic crosses the blood–brain barrier well. This factor, called pharmacokinetics, allows treatment plans based on knowing antibiotic absorption, distribution and protein binding of drugs. Some agents such as aminoglycosides are polar and largely located in the extracellular fluid. They do not penetrate so well into lung or bone and this may limit their application in some infections.
In the development of new antibiotics the way in which the new agent is absorbed and distributed throughout the body is studied by careful sampling.
This is achieved by serial measurement of the concentration of an antibiotic in the serum or at the site of infection (e.g. in the CSF for meningitis).
This may be necessary in the following.
To assist in the management of an infection with intermediate susceptibility (if inhibition of an organism occurs only at high antibiotic concentrations, it is important to ensure sufficient concentrations are found at the site of infection, e.g. in Pseudomonas meningitis, antibiotic concentrations should be measured in the CSF).
To reduce the risk of toxicity, which is important where the therapeutic index is low. Serum levels of e. g. aminoglycosides should be measured in serum taken at key times in relation to intravenous or intramuscular dosage, which allows the dose to be adjusted according to normograms. Also there should be careful adherence to guidelines, e.g. for a high peak the dosage may be reduced, or for a high trough level the medication is given less frequently).
7 Antibacterial agents – pharmacology and modes of action
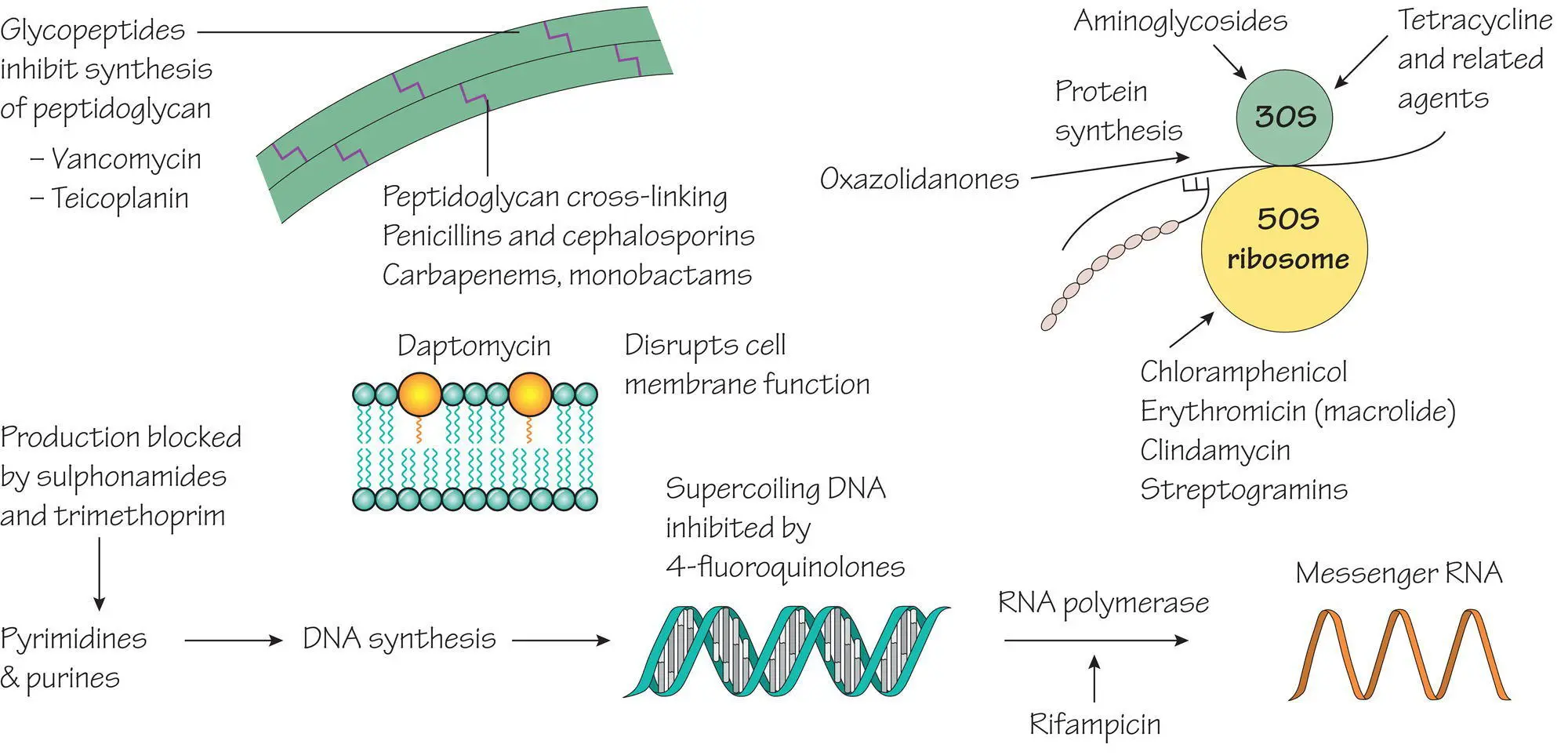
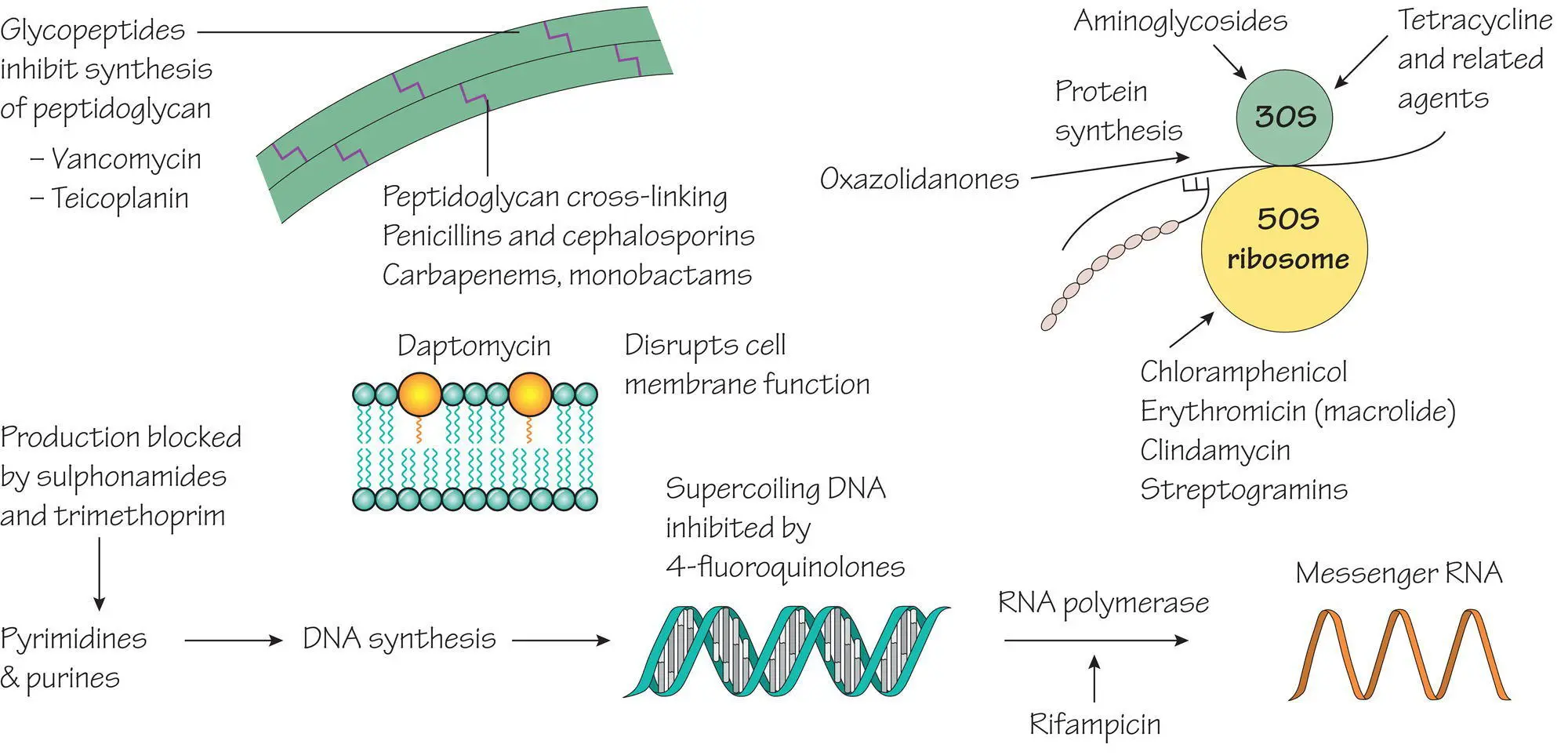
Penicillins, Cephalosporins, monobactams and carbapenems all have a beta‐lactam ring and work by inhibiting peptidoglycan cross‐linkage
Penicillins work by inhibiting peptidoglycan cross‐linkage. Modifications to the penicillins have extended their antibacterial spectrum and improved absorption. Penicillins now include:
natural penicillins (e.g. benzylpenicillin, penicillin V);
penicillinase‐resistant penicillin (e.g. flucloxacillin);
aminopenicillins (e.g. ampicillin‐like agents);
expanded‐spectrum penicillins (e.g. piperacillin);
penicillins combined with β‐lactamase inhibitors (e.g. amoxicillin and clavulanate, known as co‐amoxiclav).
Oral absorption varies: benzylpenicillin (penicillin G) is unstable in the presence of gastric acid and must be given intravenously, but penicillin V is stable and can be given orally. The aminopenicillins and flucloxacillin are also absorbed orally, while most of the remaining agents must be given intravenously.
Penicillins are secreted by the kidney and have a short half‐life. They are distributed in extracellular fluid, but do not cross the blood–brain barrier unless the meninges are inflamed.
Cephalosporins are closely related to penicillins. They are all active against Gram‐positive organisms and later compounds have activity against Gram‐negative bacteria including Pseudomonas .
The monobactams are related to penicillins and cephalosporins. They have a broad spectrum of activity, including against anaerobes. Imipenem and meropenem have antipseudomonal effects. They must be given intravenously.
Imipenem and meropenem have antipseudomonal effects and are active against bacteria producing extended spectrum β‐lactamases. They must be given intravenously.
Aminoglycosides act by preventing translation of mRNA into proteins. They are given parenterally, are limited to the extracellular fluid and are excreted in the urine. Aminoglycosides are toxic to the kidney and eighth cranial nerve at amounts close to therapeutic levels, which necessitates careful monitoring of serum concentrations.
The glycopeptides (vancomycin and teicoplanin) have the following characteristics.
They inhibit peptidoglycan cross‐linking in Gram‐positive organisms only.
Resistance to them is rare but sometimes found in enterococci (glycopeptide‐resistant enterococci – GRE) and rarely in some Staphylococcus aureus.
Administration is intravenous or intraperitoneal; they are not absorbed orally. The exception is the oral use of vancomycin to treat pseudomembranous colitis (see Chapter 24).
They are distributed in the extracellular fluid, but do not cross the blood–brain barrier unless there is meningeal inflammation.
Excretion is via the kidney.
Daptomycin, a new agent with a long half‐life, is very active against Gram‐positive organisms demonstrating more rapid killing in vitro . Its mode of action is uncertain.
Quinolones act by inhibiting bacterial DNA gyrase.
The early quinolones did not attain high tissue levels and were used only for urinary tract infections.
Fluorine modification (fluoroquinolones) has made them active against Gram‐negative pathogens including Chlamydia.
Ciprofloxacin has activity against Pseudomonas spp.
Quinolones are well absorbed orally, are widely distributed and penetrate cells well.
Newer agents (e.g. moxifloxacin) are active against Gram‐positive pathogens, including Streptococcus pneumoniae and Mycobacterium tuberculosis.
The macrolides (erythromycin, azithromycin and clarithromycin) bind to the 50S ribosome, interfering with protein synthesis; they are active against Gram‐positive cocci, many anaerobes (but not Bacteroides ), Mycoplasma and Chlamydia . They are absorbed orally, distributed in the total body water, cross the placenta, are concentrated in macrophages, polymorphs and the liver and are excreted in the bile. Erythromycin may cause nausea. The newer macrolides (e.g. azithromycin) have more favourable pharmacokinetic and toxicity profiles.
Pristinamycin is a bactericidal semisynthetic streptogramin consisting of quinupristin and dalfopristin. It acts by preventing peptide bond formation, which results in release of incomplete polypeptide chains from the donor site. It is active against a broad range of Gram‐positive pathogens and some Gram‐negatives, such as Moraxella , Legionella , Neisseria meningitidis and Mycoplasma . It is used mainly for the treatment of resistant Gram‐positive infections (e.g. GRE and glycopeptide‐intermediate S. aureus [GISA]).
The oxazolidinones (e.g. linezolid) inhibit protein synthesis at the 23S component of the 50S ribosomal subunit. They are most active against Gram‐positive bacteria and are used mainly for the treatment of resistant Gram‐positive infections. Linezolid is well‐absorbed orally and concentrated in the skin.
The main features of metronidazole are that it is:
active against all anaerobic organisms;
Читать дальше