Self‐expression – The expression of one's opinions and feelings must be learned and stimulated without being held back by strict or oppressive rules.
Realistic limits – In order to live in a society with others, it is necessary for children to learn certain rules. They must understand when to subdue their autonomy or self‐expression when dealing with others and be capable of doing so. Children also have to learn to tolerate and adequately deal with frustrations (Young & Klosko, 1994; Young et al., 2003).
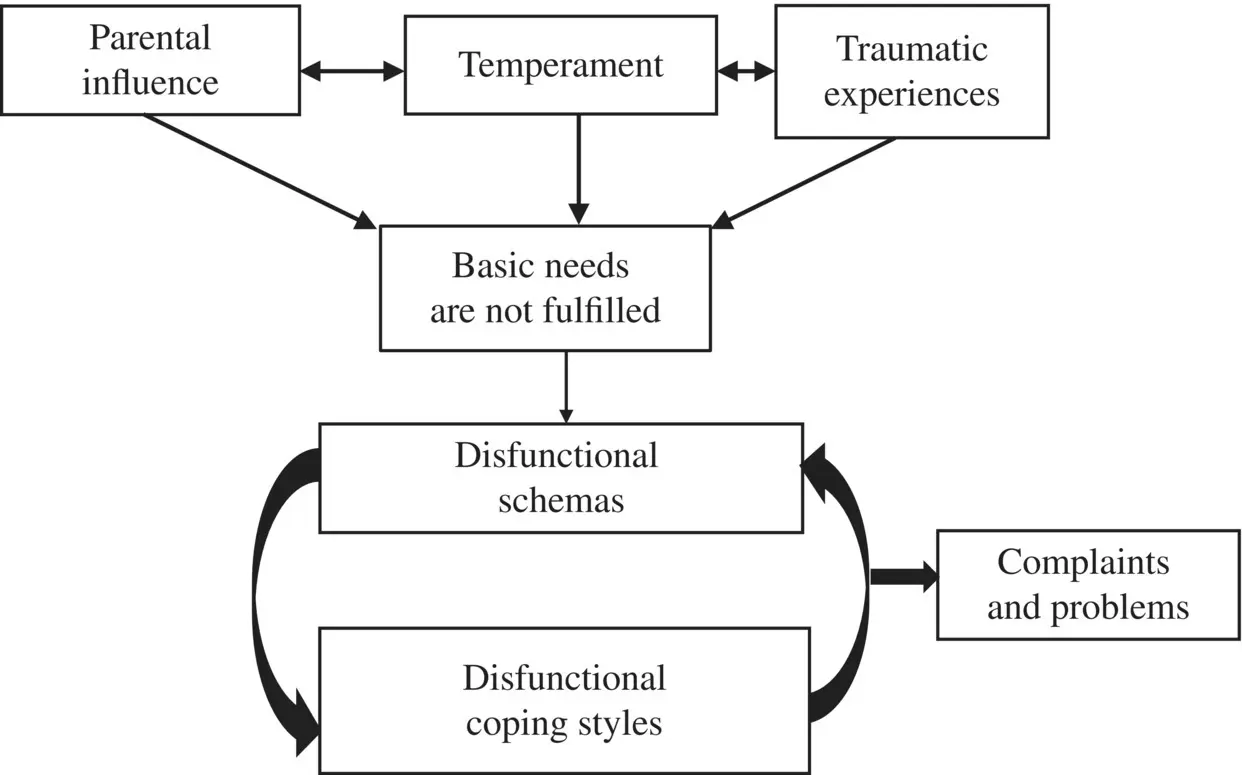
When these needs are not met, whether solely due to shortcomings in the child's environment, or in combination with traumatic events (such as emotional, physical, or sexual abuse, or being bullied), this can form—in interaction with the temperament of the child—dysfunctional schemas and coping strategies (see Figure 2.1). The dysfunctional schemas that are formed during childhood development are called “early maladaptive schemas.” Given the circumstances in which the child grew up, they are usually understandable (e.g., a child growing up in an environment where there is a lot of threat of abandonment has an increased risk to develop an abandonment schema). Young describes 18 different early maladaptive schemas (see Appendix I) and three groups of coping strategies (see Appendix J) (Young et al., 2003).
The schemas and coping styles form a sort of alternative for the personality disorder diagnostic system in the DSM‐5 (American Psychiatric Association [APA], 2013). For BPD, so many schemas have been found that a treatment based solely on a schema conceptualization would be very complex. Moreover, the 18 schemas and three coping styles lead to 54 possible combinations, further complicating the task to understand the patient's problems with this model.
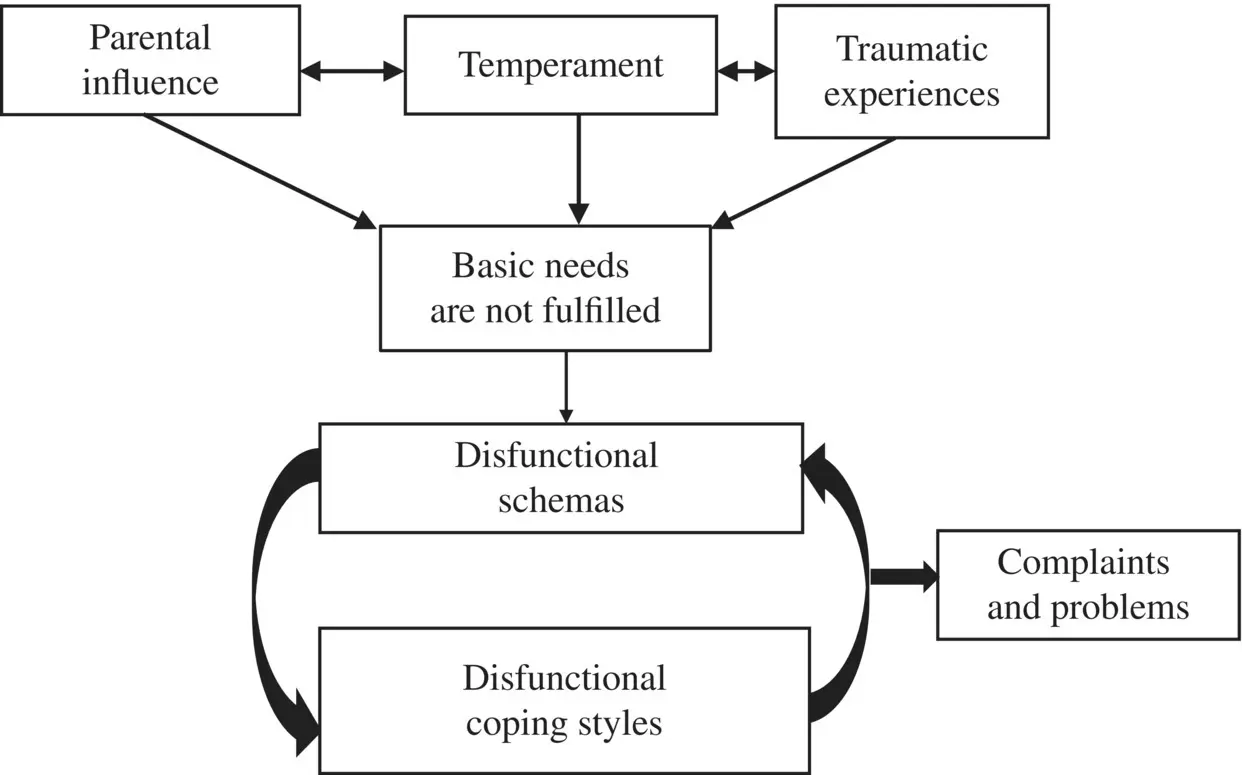
Figure 2.1 The development of dysfunctional schemas
Patients with BPD often have so many different schemas present at the same time that both patient and therapist cannot see the wood for the trees. Because shifts in behavior and feelings take place so quickly, it is difficult for the patient herself, let alone for those around her, to understand what is taking place. This further exacerbates an already complex problem. These sudden shifts in patterns of feeling, thinking and behavior, which are so common in BPD, have inspired the development of the concept of a “schema mode” (also called “mode” or “schema state”) (McGinn & Young, 1996). A schema mode is a set of schemas and processes, which, in certain situations, determine the thoughts, feelings, and actions of the patient at the cost of other schemas. In other words, when the BPD patient is relatively relaxed and comfortable, one sees a totally different side of her personality as opposed to when she feels threatened. Under normal circumstances, one sees a relatively quiet patient who appears to have few emotions. However, when, for example, the threat of abandonment by an important figure is posed, one sees a “young child” being very upset and completely inconsolable. A patient with BPD can switch from one strong mood or emotion to another in a very short period of time. According to the schema mode model, this is due to the patient's continual and uncontrolled shifts from one mode to the other.
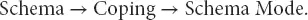
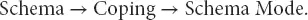
It is important to understand that schema modes are related to schema's, and that there is no fundamental difference between schema theory and schema mode theory. The schema model as formulated by Young et al. (2003) states that when an early maladaptive schema is triggered, or is threatened to be triggered, people use specific ways of coping to deal with this activation, as the activation is usually experienced as highly unpleasant and signaling threat. The ways of coping are grouped in three coping styles: overcompensation, avoidance, and surrender—analogous to the primitive coping under high stress common to mammals (fight, flight, freeze). The combination of a schema that is (threatened to be) triggered and a coping response is a schema mode. In other words:
Two studies have actually supported this model, in that they demonstrated that coping indeed determines how modes are related to schemas (in statistical terms: the coping style mediates the relationship between schemas and modes) (Rijkeboer & Lobbestael, 2012; van Wijk‐Herbrink et al., 2018). The last study even went one step further, demonstrating that the very same early maladaptive schemas can underlie internalizing as well as externalizing psychopathology, and that it depends on the type of coping, hence the schema modes, whether a (threatened) schema activation results in internalizing or externalizing psychopathology:

Thus, in the phase of case conceptualization (see Chapter 3) it is meaningful to combine the mode model as described below with the specific schemas that give “color” to the mode of your individual patient. When patient A is in the abandoned/abused child mode she might feel stupid (schema defectiveness/shame) and distrustful (schema mistrust/abuse) while patient B might feel abandoned (schema abandonment/instability) and dependent (schema dependence/incompetence).
Young suggested that the following five modes are characteristic of BPD: the detached protector, the abandoned/abused child, the angry/impulsive child, the punitive parent, and the healthy adult (actually, a weak healthy adult mode). Recently an extra important mode has been added to the model: the happy child mode, which is also weak in BPD. In some cases, we also see an undisciplined or impulsive child, which we will describe in combination with the angry child. These modes can be renamed to make them more applicable to the patient's situation (see Figure 2.2).
In clinical practice we advise to make a more extensive case conceptualization in which the origins of the schemas and modes in the youth and the current problems are described. In each mode the specific schema's that give “color” to the mode of your individual patient are added (see Figure 2.3for an example).
We must strongly emphasize that this heuristic model does not infer that BPD is a multiple personality disorder. Giving names to the different modes is a means of helping the patient to better understand and identify with the mode and does not have any reference to identities or persons.
The following are descriptions of the different modes most prominent in BPD. The modes are also demonstrated in a recent audiovisual production (ST step by step, van der Wijngaart & van Genderen, 2018). Chapter 9further describes treatment and how therapists can best address the different modes.

Figure 2.2 Borderline personality disorder: six modes
When the patient is in the detached protector mode, the patient seems relatively mature and calm (See ST step by step 5.08). A therapist could assume the patient is doing well. In fact, the patient uses this protective mode in order to avoid experiencing or revealing her feelings of fear (abandoned/abused child), inferiority (punitive parent), or anger (angry/impulsive child).
Читать дальше