1 ...8 9 10 12 13 14 ...29 Some abbreviations used in prescriptions
| Abbreviation |
Latin |
English |
| a.c. |
ante cibum |
Before food |
| ad lib. |
ad libitum |
To the desired amount |
| b.d. or b.i.d. |
bis in die |
Twice a day |
| c. |
cum |
With |
| o.m. |
omni mane |
Every morning |
| o.n. |
omni nocte |
Every night |
| p.c. |
post cibum |
After food |
| p.r.n. |
pro re nata |
Whenever necessary |
| q.d. |
quaque die |
Every day |
| q.d.s. |
quaque die sumendum |
Four times daily |
| q.i.d. |
quater in die |
Four times daily |
| q.q.h. |
quater quaque hora |
Every four hours |
| R. |
recipe |
Take |
| s.o.s. |
si opus sit |
If necessary |
| stat. |
statim |
At once |
| t.d.s. |
ter die sumendum |
Three times daily |
| t.i.d. |
ter in die |
Three times daily |
Chapter 1 Introduction to pharmacology
Ian Peate
The aim of this chapter is to provide the reader with an introduction to therapeutic pharmacology and the key issues surrounding medicines management.
After reading this chapter, the reader will be able to:
1 Discuss the importance of patient assessment in association with medicines management
2 Understand the role of the Code and other professional duties
3 Appreciate the importance of the proficiencies of pre‐registration nurse education related to medicines management
4 Acknowledge and respect patient preference
1 What is the nursing process?
2 Describe the keys skills that are associated with patient assessment.
3 Discuss the role and function of the Nursing and Midwifery Council.
4 What does medicines optimisation mean?
5 Discuss risk management strategies in medicines management.
There has been a vast increase in the use of therapeutic agents for medical treatment. The administration of medicines is a common yet important clinical activity. The way in which a medicinal product is administered can determine whether the patient gains any therapeutic benefit or if they will experience any adverse effects from their medicines. The volume and complexity of medication administration contributes to the actual and potential risk of medication errors, which will have a negative impact on a person's health and wellbeing.
The key requirement of a healthcare provider is to ‘do no harm’, and this is particularly important when the nurse is working with people who have been prescribed medication. The administration of medicines is but one part of the nurse's role; an understanding of pharmacology is essential if the nurse is to provide care that is safe and effective. As well as an understanding of pharmacology, the nurse is also required to work with patients and their families in explaining how to administer the medication, explaining the anticipated effects, the action(s) of the medications and the potential adverse reactions or side effects.
When a patient is admitted to a healthcare facility (regardless of the setting), an initial assessment must be undertaken which has to include a detailed medication history. Information must be obtained from the patient (and, if appropriate, the patient's family), and information may also be collected from the patient's pharmacy and/or the general practitioner with their permission. In addition, any medications that have been brought in by the patient must be documented and kept in a safe location. At all times, local policy and procedure must be adhered to.
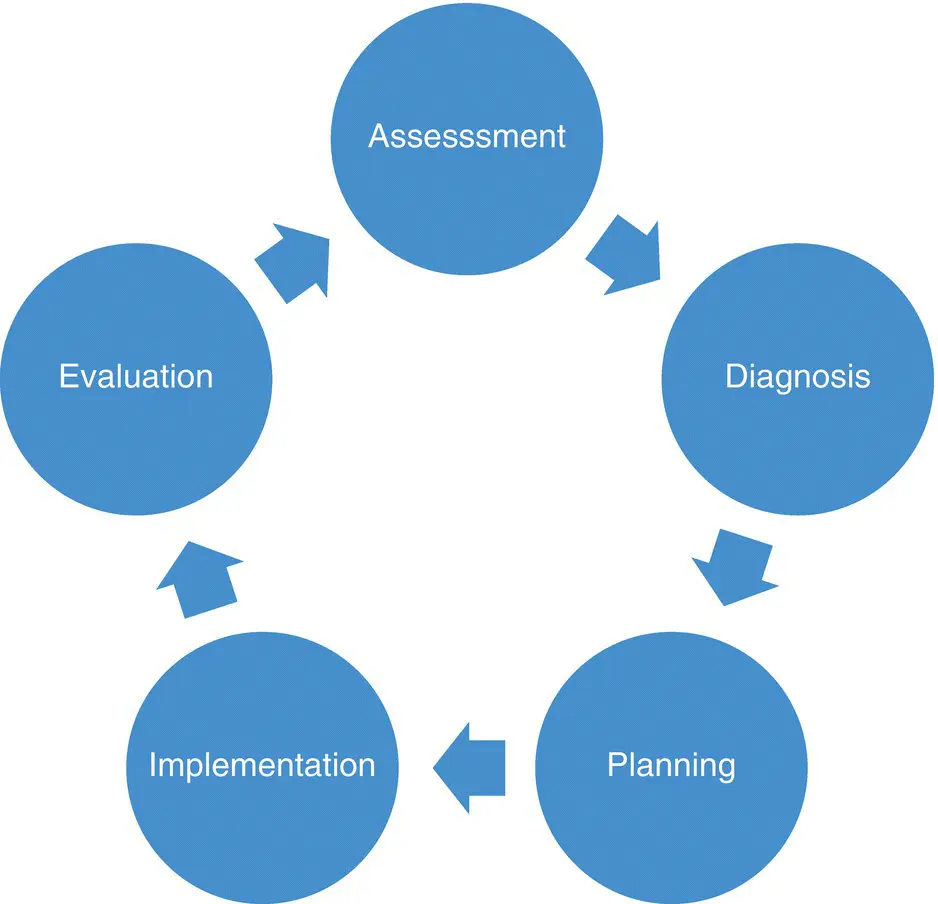
Assessment is the first stage in the planning of care, it is associated with the process of gathering information in order to make decisions about appropriate interventions (Ballantyne, 2015). During the assessment stage, the patient's story is listened to and the nurse–patient relationship is strengthened, ensuring that the patient is truly at the heart of all that is done. The nursing process is a systematic, developing, dynamic approach, that is cyclical in nature, and as such assessment must not be seen as a one‐off activity: it is not linear by nature; it is ongoing.
When assessing needs – and this also relates to assessing needs and the use of medications – data is gathered, analysed and organised, and the data is acted upon as critical thinking skills and the mobilisation of resources are used to achieve goals and outcomes that have been set, when possible, in partnership with the patient (Stonehouse, 2017).
Having undertaken patient assessment, a diagnosis is formulated, a plan of care is devised relating to the needs that have emerged following assessment, care is provided using a holistic approach, and finally all that has been done is evaluated to establish efficacy. See Figure 1.1: a systematic approach to care.
The safety and success of medicines administration is based on ongoing nursing assessment. All healthcare providers have a professional duty to ensure that they offer care that is safe and effective (Nursing and Midwifery Council (NMC), 2018b,2018c). As well as professional obligations, there are also requirements that must be given due diligence in order to ensure that patient safety is paramount. There is much legislation regarding medicines (see Chapter 3), and the nurse must also adhere to the laws of the country in which they are working.
The skills of assessment require the nurse to undertake a physical and psychological assessment of the person's needs. The nurse obtains a patient history and carries out a physical examination (if required) to identify needs. There are a number of components associated with assessment. Assessment requires the nurse to:
observe the patient
undertake a clinical examination
gather data
communicate
undertake various measurements.
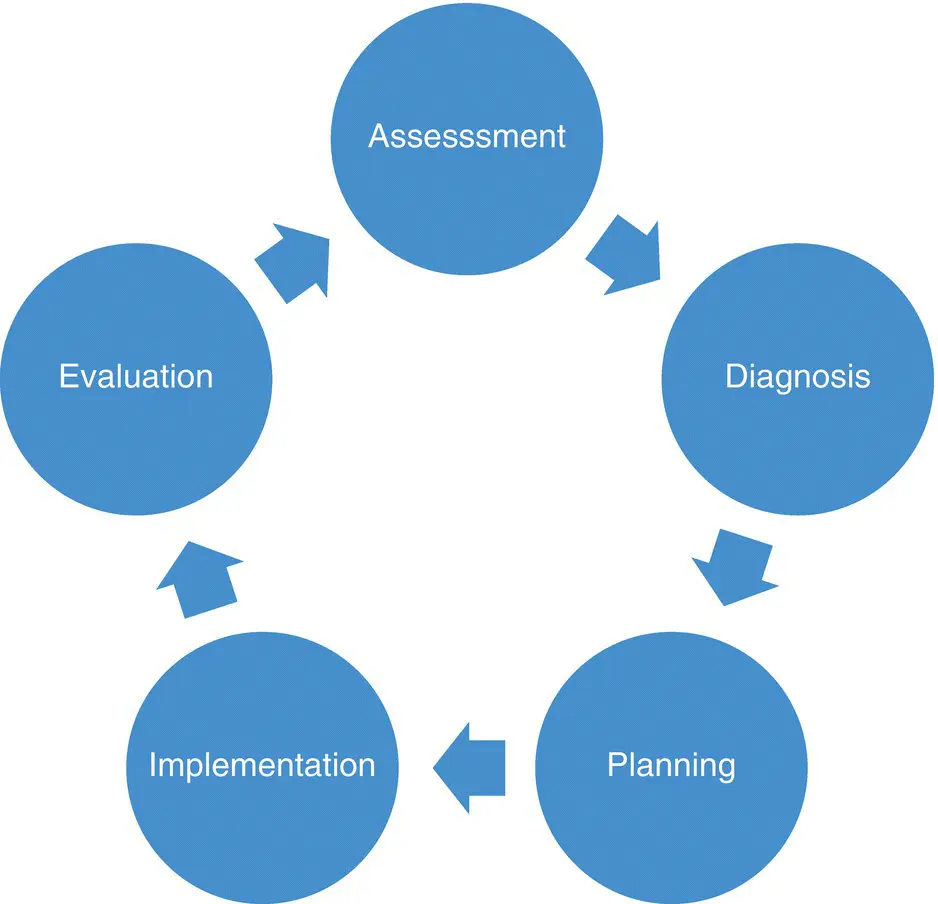
Figure 1.1 A systematic approach to care provision.
Clinical judgment is used to determine the type of assessment required. It is important during the assessment phase to ensure the use of a framework to guide the process as this will help to provide structure and order.
The NMC has suggested that newly qualified nurses will be able to go on a prescribing course soon after their initial pre‐registration education; in order to do this, there is a need to include more prescribing theory in undergraduate nursing programmes allowing nurses to prescribe from a limited formulary. It is important to note that nurses will not prescribe at the point of entry to the register (when their pre‐registration nurse education is complete), but will complete a post‐registration qualification in order to prescribe (NMC, 2018b).
All nursing professionals must practise in line with the requirements of The Code (NMC, 2018a), the professional standards of practice and behaviour that nurses, midwives and nursing associates are required to uphold.
The NMC is the nursing and midwifery regulator for England, Wales, Scotland, Northern Ireland and the Islands. It exists to protect the public and it does this in a number of ways. The NMC sets the standards of education, training and conduct that nurses and midwives are required to adhere to so as to deliver high‐quality healthcare. The NMC ensures that nurses and midwives keep their skills and knowledge up to date (through revalidation; NMC, 2017) and uphold the standards of the Code (NMC, 2018a). Where an allegation is made about a nurse's standard of practice or behaviour, the NMC have processes in place to investigate those allegation: they take action if concerns are raised about a nurse's fitness to practice.
Читать дальше