Part 1 Foundations of Endocrinology
CHAPTER 1 Overview of endocrinology
Key topics
A brief history of endocrinology and diabetes
The role of hormones
Classification of hormones
Control systems regulating hormone production
Endocrine disorders
Key points
To be capable of defining endocrinology
To understand what endocrinology means as a basic science and a clinical specialty
To appreciate the history of endocrinology
To understand the classification of hormones into peptides, steroids and amino acid derivatives
To understand the principle of how feedback mechanisms regulate hormone levels in the circulation
This chapter introduces endocrinology and diabetes including some of the basic principles that underpin the following chapters
Box 1.1The endocrine and nervous systems are the two main communication systems in the body
| Monitor internal and external environments |
Ensure homeostasis |
| Allow appropriate adaptive changes |
| Communicate via chemical messengers |
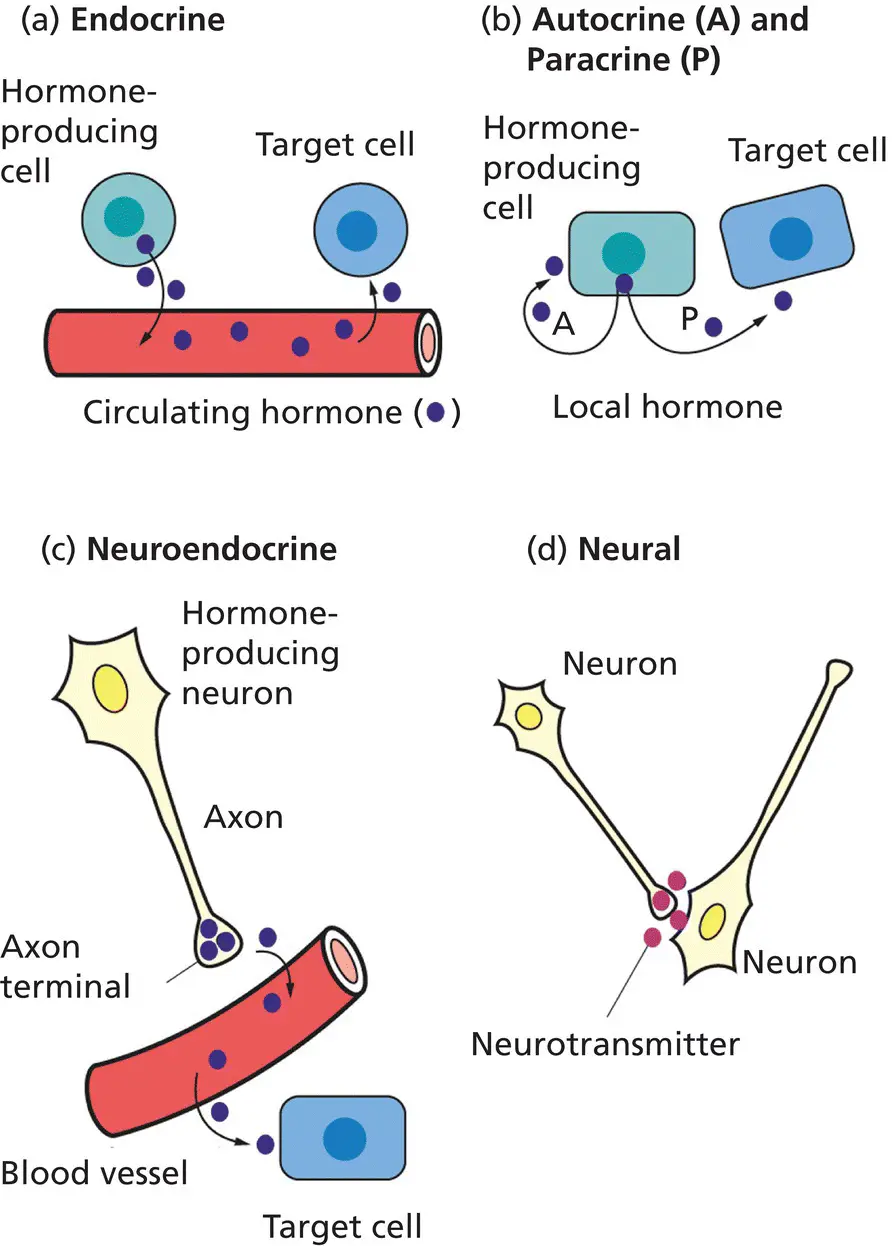
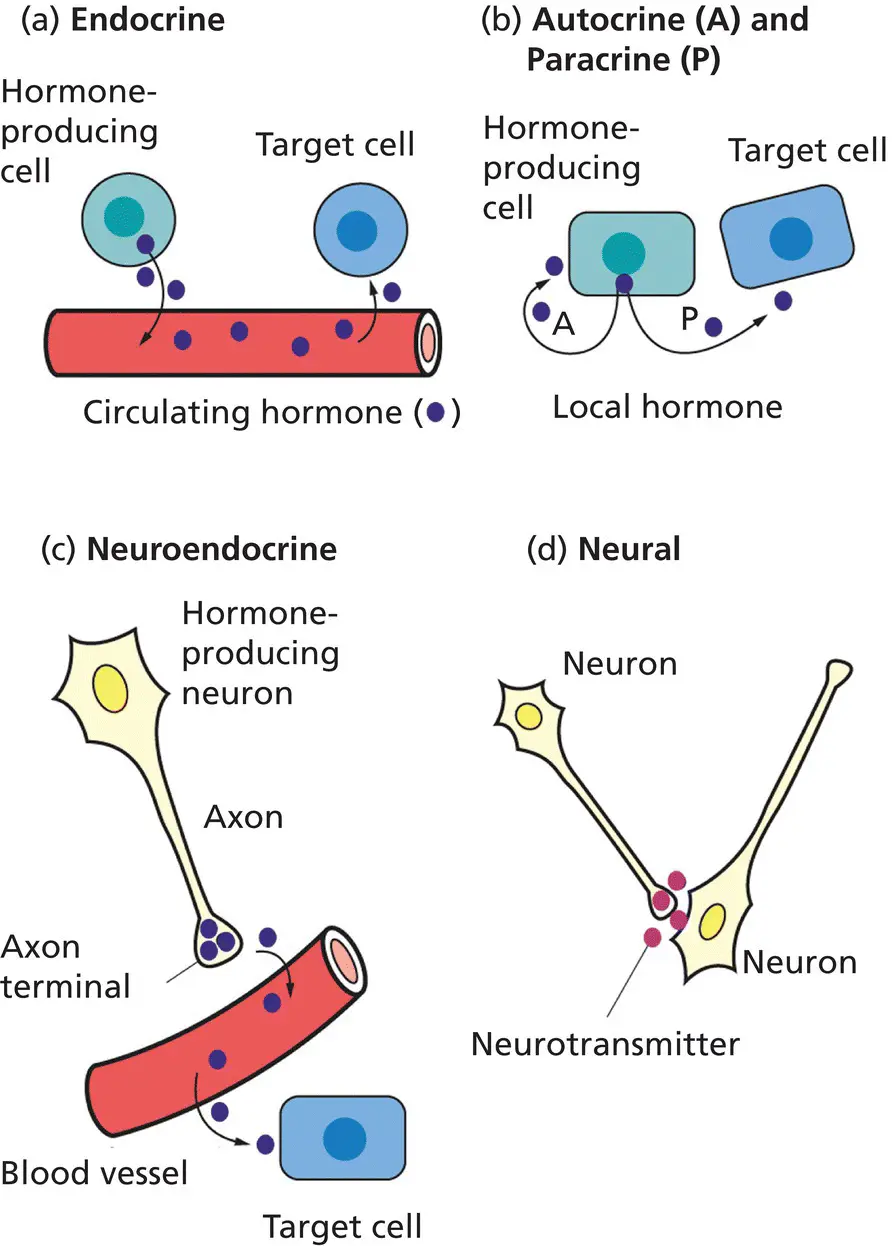
Figure 1.1 Chemical signalling in the endocrine and neural systems. (a) In endocrine communication, the producing cell secretes hormone into the blood vessel, where it is carried, potentially over large distances, to its target cell. (b) Sometimes hormones can act on the cell that produces them (autocrine, A) or nearby cells (paracrine, P) without the need for transport via the circulation. For instance, glucagon from α‐cells and somatostatin from δ‐cells can regulate insulin secretion by adjacent β‐cells within the pancreatic islet. (c) In neuroendocrine communication, neurons can secrete hormones into the surrounding blood vessels to reach a more distant target. A good example is hypothalamic regulation of the anterior pituitary. (d) In pure neural communication, neurons activate other neurons via neurotransmitters released from axonic terminals into the synaptic space. Conceptually, neurotransmitters are similar to hormones and in some instances, such as for norepinephrine/noradrenaline, can actually be the same chemical.
All organisms need to be able to analyze and respond to their surroundings in order to provide a constant internal environment. Maintaining this internal constancy is called homeostasis. For an organism comprised of a single or a few cells homeostasis is relatively easy as no cell is more than a short diffusion distance from the outside world or its neighbours. This simplicity has been lost with the evolution of more complex, larger, multicellular organisms. Diffusion alone is inadequate in larger animal species where discrete functions localize to specific organs. In humans, there are ∼10 14cells of more than 200 different types. With this compartmentalized function comes the need for effective communication to disseminate information throughout the whole organism – only a few cells face the outside world, yet all need to respond to it. Two communication systems facilitate this: the endocrine and nervous systems ( Box 1.1).
Whereas gastrointestinal cells tend to secrete chemicals into ducts, the specialized cells that make up the glands and tissues of the endocrine system release their chemical messengers, called hormones, into the extracellular space, from where they enter the bloodstream. Historically, this blood‐borne transit of hormones was what defined ‘endocrinology’; however, the principle is identical for hormone action on a neighbouring cell (called a paracrine effect) or, indeed, the endocrine cell itself (an autocrine or intracrine effect) ( Figure 1.1).
The nervous and endocrine systems interact. Endocrine glands can be under nervous control; the adrenal medulla is an excellent example ( Chapter 6). Conversely, neural cells can themselves release hormones into the bloodstream. This is particularly relevant in the hypothalamus ( Chapter 5). Indeed, this interplay between the body's two main communication systems has led to the composite specialty of ‘neuroendocrinology’ ( Figure 1.1).
A brief history of endocrinology and diabetes
The term ‘hormone’, derived from the Greek word ‘hormaein’ meaning ‘to arouse’ or ‘to excite’, was first used in 1905 by Sir Ernest Starling in his Croonian Lecture to the Royal College of Physicians. However, endocrinology is built on foundations that are far older. Although Aristotle described the pituitary, gigantism, caused by excess growth hormone (GH) from the somatotrophs of the anterior pituitary, was referred to in the Old Testament. It was only two millennia or so later in the 19th century that the gland’s anterior and posterior components were appreciated by Rathke, and Pierre Marie connected GH‐secreting pituitary tumours to acromegaly and excess growth.
Diabetes was recognized by the ancient Egyptians. Areateus later described the disorder in the second century AD as ‘a melting down of flesh and limbs into urine’. Consequently, diabetes comes from the Greek word meaning ‘siphon’. The pancreas was only implicated relatively recently when Minkowski realized in 1889 that the organ’s removal in dogs mimicked diabetes in humans.
The roots of reproductive endocrinology are equally long. The Bible refers to eunuchs and Hippocrates recognized that mumps could result in sterility. Oophorectomy in sows and camels was used to increase strength and growth in ancient Egypt. The dependence of endocrinology on technology is also long standing. It took the invention of the microscope in the 17th century for Leeuwenhoek to visualize spermatozoa and later, in the 19th century, for the mammalian ovum to be discovered in the Graafian follicle.
During the last 500 years, many endocrine organs and systems (‘axes’) have been identified and characterized. In 1564, Bartolomeo Eustacio noted the presence of the adrenal glands. Almost 300 years later (1855), Thomas Addison, one of the forefathers of clinical endocrinology, described the consequences of their inadequacy. Catecholamines (epinephrine/adrenaline and norepinephrine/noradrenaline) were identified at the turn of the 19th century, in parallel with Oliver and Schaffer’s discovery that these adrenomedullary substances raised blood pressure. This followed shortly after the clinical features of myxoedema were linked to the thyroid gland, when, in 1891, physicians in Newcastle‐upon‐Tyne treated hypothyroidism with sheep thyroid extract. This was an important landmark, but long after the ancient Chinese recognized that seaweed, as a source of iodine, held valuable properties in treating swelling of the thyroid gland (‘goitre’).
These early aspects of clinical endocrinology and diabetes tended to rely on recognition and description. Since then our understanding has advanced through:
Successful quantification of circulating hormones
Molecular unravelling of complex hormone action
Mechanistic identification of pathophysiology underlying endocrine dysfunction
Molecular genetic diagnoses
Some of the landmarks from the last 100 years are shown in Box 1.2. Endocrinology and diabetes is notable for researchers who have been awarded the Nobel Prize for Medicine, Physiology or Chemistry for their landmark discoveries ( Table 1.1).
Box 1.2Some landmarks in endocrinology over the last century or so
| 1905 |
First use of the term ‘hormone’ by Starling in the Croonian Lecture at the Royal College of Physicians |
| 1909 |
Cushing removed part of the pituitary and saw improvement in acromegaly |
| 1914 |
Kendall isolated an iodine‐containing substance from the thyroid |
| 1921 |
Banting and Best extracted insulin from islet cells of dog pancreas and used it to lower blood glucose |
| Early 1930s |
Pitt‐Rivers and Harrington determined the structure of the thyroid hormone, thyroxine |
| 1935–1940 |
Crystallization of testosterone |
| 1935–1940 |
Identification of oestrogen and progesterone |
| 1940s |
Harris recognized the relationship between the hypothalamus and anterior pituitary in the ‘portal‐vessel chemotransmitter hypothesis’ |
| 1952 |
Gross and Pitt‐Rivers identified tri‐iodothyronine in human serum |
| 1955 |
The Schally and Guillemin laboratories showed that extracts of hypothalamus stimulated adrenocorticotrophic hormone (ACTH) release |
| 1950s |
Adams and Purves identified thyroid stimulatory auto‐antibodies |
| Gonadectomy and transplantation experiments by Jost led to the discovery of the role for testosterone in rabbit sexual development |
| 1955 |
Marcel Janbon and colleagues first recognized the hypoglycaemic effects of sulphonamide antibiotics during a typhoid epidemic in Marseilles in 1942. This led to the introduction of sulphonylureas into clinical practice |
| 1955 |
Sanger reported the primary structure of insulin |
| 1956 |
Doniach, Roitt and Campbell associated antithyroid antibodies with some forms of hypothyroidism – the first description of an autoimmune phenomenon |
| 1957 |
Growth hormone was used to treat children with short stature |
| 1966 |
First transplant of human pancreas to treat type 1 diabetes by Kelly, Lillehei, Goetz and Merkel at the University of Minnesota |
| 1969 |
Hodgkin reported the three‐dimensional crystallographic structure of insulin |
| 1969–1971 |
Discovery of thyrotrophin‐releasing hormone (TRH) and gonadotrophin‐releasing hormone (GnRH) by Schally’s and Guillemin’s groups |
| 1973 |
Discovery of somatostatin by the group of Guillemin |
| 1981–1982 |
Discovery of corticotrophin‐releasing hormone (CRH) and growth hormone‐releasing hormone (GHRH) by Vale |
| 1983 |
Cloning of gene encoding glucagon and two glucagon‐like peptides, including GLP‐1, by Bell and colleagues |
| 1994 |
Identification of leptin by Friedman and colleagues |
| 1994 |
First transplantation of pancreatic islets to treat type 1 diabetes by Pipeleers and colleagues in Belgium |
| 1999 |
Discovery of ghrelin by Kangawa and colleagues |
| 1999 |
Sequencing of the human genome – publication of the DNA code for chromosome 22 |
| 2000 |
Advanced islet transplantation using modified immunosuppression by Shapiro and colleagues to treat type 1 diabetes |
| 2005 |
GLP‐1 receptor agonists introduced into clinical practice |
| 2010 |
SGLT‐2 inhibitors entered clinical practice |
Table 1.1 Nobel prizewinners in endocrinology and diabetes or those whose discoveries have profoundly affected the specialty
Читать дальше