1.14 Red cell preservation
The role of 2,3‐diphosphoglycerate in oxygen transport by red cells was discovered in the mid‐1960s [37, 38]. It had been known previously that this compound was better maintained at higher pH, whereas adenosine triphosphate, which appeared to be involved in red cell survival, was maintained better at a lower pH. The addition of adenine was shown to improve adenosine triphosphate maintenance and prolong red cell survival and storage for transfusion [39]. The next major advance in red cell preservation was the development of preservative solutions designed to be added after removal of most of the original anticoagulated plasma, thus further extending the storage period of red cells [40].
1.15 Leukocyte antigens and antibodies
In 1926, Doan [41] described the sera of some individuals that caused agglutination of the leukocytes from others. Subsequent studies established the presence of leukocyte antibodies, the presence of these antibodies in the sera of polytransfused patients, the occurrence of white cell agglutinins in response to fetomaternal immunization, and the alloimmune and autoimmune specificities associated with these antibodies. These studies, along with studies of the murine histocompatibility system, led to the description of the major histocompatibility system (human lymphocyte antigens) [42] in humans and the understanding that there are separate antigenic specificities limited to neutrophils as well [43]. These studies also defined the causative role of leukocytes in febrile nonhemolytic transfusion reactions [44]. Strategies were sought to prevent these reactions by removing the leukocytes from blood [45, 46], one of the first methods being reported by Fleming [46], who discovered penicillin.
1.16 Platelet collection, storage, and transfusion
The relationship between bleeding and thrombocytopenia had been known for some time, but the development of the plastic bag system for blood collection made platelets available for transfusion. Several years of work by many investigators—predominantly at the National Cancer Institute during the 1960s—developed the methods for preparing platelets and established that platelet transfusion to patients with thrombocytopenia reduced mortality from hemorrhage [47]. Initially, platelets had to be transfused within a few hours after the whole blood was collected, and thus large‐scale application in the general medical care setting was impractical. The seminal report by Murphy and Gardner [48] showing that room temperature allowed platelets to be stored for several days revolutionized platelet transfusion therapy.
Plastic bags were used to remove whole blood, separate the plasma from the red cells, retain the plasma, and return the red cells, thus making it possible to obtain substantial amounts of plasma from one donor [49]. This initiated the concept of attempting to obtain only selected portions of whole blood to collect larger amounts of plasma or cells. The centrifuge developed by Cohn for plasma fractionation was modified by Jack Latham and became a semiautomated system for plasmapheresis [50] and subsequently was used for platelet collection as well [51, 52]. At the National Institutes of Health Clinical Center, an IBM engineer worked with hematologists to develop a centrifuge that enabled collection of platelets or granulocytes from a continuous flow of blood through the instrument [53, 54]. Later versions of these instruments have become widely used for plateletpheresis and leukophoresis.
1.18 Granulocyte transfusions
As the benefits of platelet transfusion for thrombocytopenic patients were recognized, interest developed in using the same strategy to provide granulocyte transfusion to treat infection in patients with neutropenia. Initial attempts involved obtaining granulocytes from patients with chronic myelogenous leukemia [55, 56]. Transfusion of these cells had clinical benefits [57], and this led to a decade of effort to develop methods to obtain granulocytes from normal donors [58]. At best, these methods produced only modest doses of granulocytes; improvements in antibiotics and general patient care have supplanted the need for granulocyte transfusions except in very limited circumstances (see Chapters 10and 11).
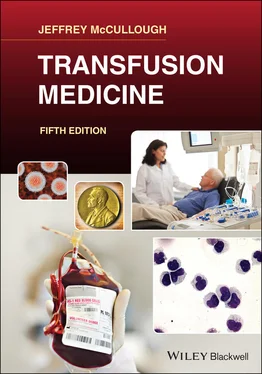
Blood banking and transfusion medicine developed slowly during the 1950s but much more rapidly between the 1960s and the 1980s. Some of the important advances mentioned in this chapter were understanding blood groups and the identification of hundreds of specific red cell antigens; the development of the plastic bag system for blood collection and separation; plasma fractionation for the production of blood derivatives, especially factor VIII; improved red cell preservation; platelet preservation and transfusion; understanding hemolytic and febrile transfusion reactions; expanded testing for transmissible diseases; and the recognition of leukocyte and platelet antigen systems. Blood collection and storage is now a complex process operated much like the manufacturing of a pharmaceutical. Transfusion medicine is now the complex, sophisticated medical–technical discipline that makes possible many modern medical therapies.
1 1. Greenwalt TJ. The short history of transfusion medicine. Transfusion 1997; 37:550–563.
2 2. Oberman HA. The history of blood transfusion. In: Petz LD, Swisher SN, eds. Clinical Practice of Blood Transfusion. New York: Churchill Livingstone, 1981, pp. 11–32.
3 3. Kilduffe RA, de Bakey M. The Blood Bank and the Technique and Therapeutics of Transfusions. St. Louis, MO: CV Mosby, 1942.
4 4. Lyons AS, Keiner M. Circulation of the blood. In: Lyons AS, Petrucelli RJ II, Abrams NH, eds. Medicine: An Illustrated History. New York: Harvey N Abrams, 1978, pp. 437–459.
5 5. Mollison PL, Engelfriet P. Blood transfusion. Sem Hematol 1999; 36:48–58.
6 6. Lower R. A treatise on the heart on the movement and color of the blood and on the passage of the chyle into the blood. In: Franklin KJ, ed. Special Edition, The Classics of Medicine Library. Birmingham, AL: Gryphon Editions Inc., 1989.
7 7. Farr AD. The first human blood transfusion. Med Hist 1980; 24:143–162.
8 8. Blundell J. Successful case of transfusion. Lancet 1928–1929; 1:431–432.
9 9. Huestis DW. The first blood transfusion in Russia (1832). Transfusion 2004; 44:1367–1369.
10 10. Kuhns WJ. Historical milestones—blood transfusion in the Civil War. Transfusion 1965; 5:92–94.
11 11. Landsteiner K. On agglutination of normal human blood. Transfusion 1961; 1:5–8.
12 12. Isohemagglutination: recommendation that the Jansky classification be adopted for universal use. JAMA 1921; 76:130–131. Miscellany.
13 13. Hektoen L. Iso‐agglutination of human corpuscles. JAMA 1907; 48:1739–1740.
14 14. Ottenberg R. Studies in isohemagglutination, I: transfusion and the question of intravascular agglutination. J Exp Med 1911; 13:425–438.
15 15. Crile GW. Technique of direct transfusion of blood. Ann Surg 1907; 46:329–332.
16 16. Doan C. The transfusion problem. Physiol Rev 1927; 7:1–84.
17 17. Braxton‐Hicks J. Case of transfusion: with some remarks on a new method of performing the operation. Guys Hosp Rep 1869; 14:1–14.
18 18. Lewisohn R. The citrate method of blood transfusion after ten years. Boston Med Surg J 1924; 190:733.
19 19. Weil R. Sodium citrate in the transfusion of blood. JAMA 1915; 64:425.
20 20. Robertson O. Transfusion with preserved red blood cells. Br Med J 1918; 1:691.
21 21. Jorda JD. The Barcelona blood transfusion service. Lancet 1939; 1:773.
Читать дальше