This is the epithelial tissue located in the sulcus, and it extends from the free gingival margin to the most coronal portion of the junctional epithelium. It is a nonkeratinized stratified squamous epithelium.
The junctional epithelium extends apically from the base of the gingival sulcus following the tooth structure, and it is a nondifferentiated stratified squamous epithelium. 23In healthy situations with no history of periodontal disease or gingival deformities, the deepest portion of the junctional epithelium is located around the CEJ. It has a triangular shape with the base at the bottom of the sulcus and a vertex located apically. The base of the junctional epithelium has a layer 20 to 30 cells thick, which decreases in number to become a bilayer at the level of the CEJ. 24The junctional epithelium is attached to the tooth surface through hemidesmosomes, while the connections in between the epithelial cells are established by desmosomes, adherents, gaps, and tight junctions. 25
The gingival epithelial tissue lies over connective tissue establishing finger-type indentations of epithelial tissue termed ridges . This connective tissue subjacent to the epithelium of the attached gingiva is known as lamina propria. The lamina propria is a highly vascularized tissue with two known portions: the papillary layer, which is the most superficial, and the reticular layer. In the papillary layer, the interphase between the connective tissue of the lamina propria and the epithelium follow a wavy morphology with projections of connective tissue called papillae and epithelial ridges known as rete pegs. The interface between the sulcular epithelium, the junctional epithelium, and the connective tissue is characterized by the absence of rete pegs. The lamina propria consists of 57% to 60% connective tissue fibers/fibrous proteins, 5% to 8% cells, and 35% other components such as blood vessels, nerves, and ground substance of the intercellular matrix. 5,26
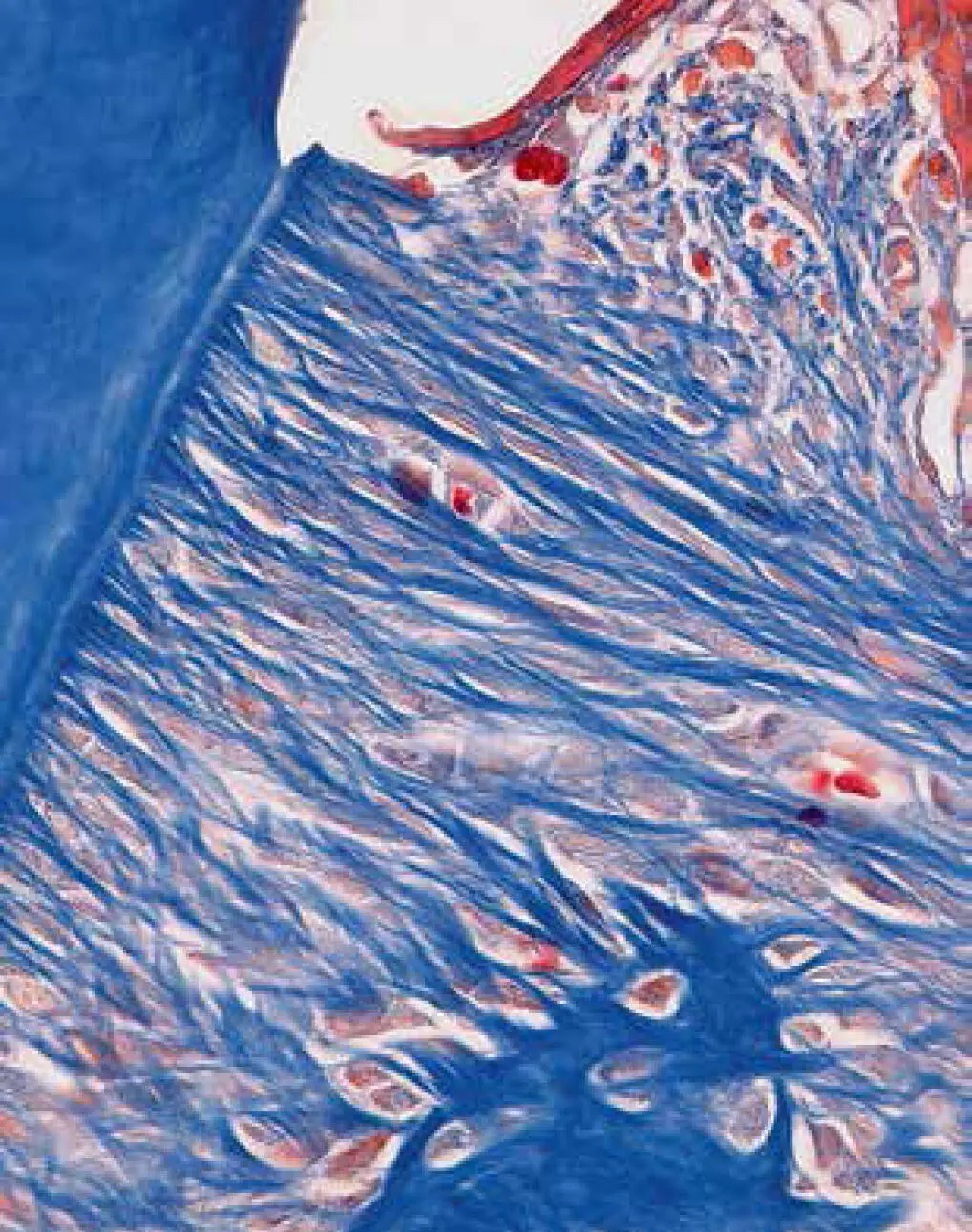
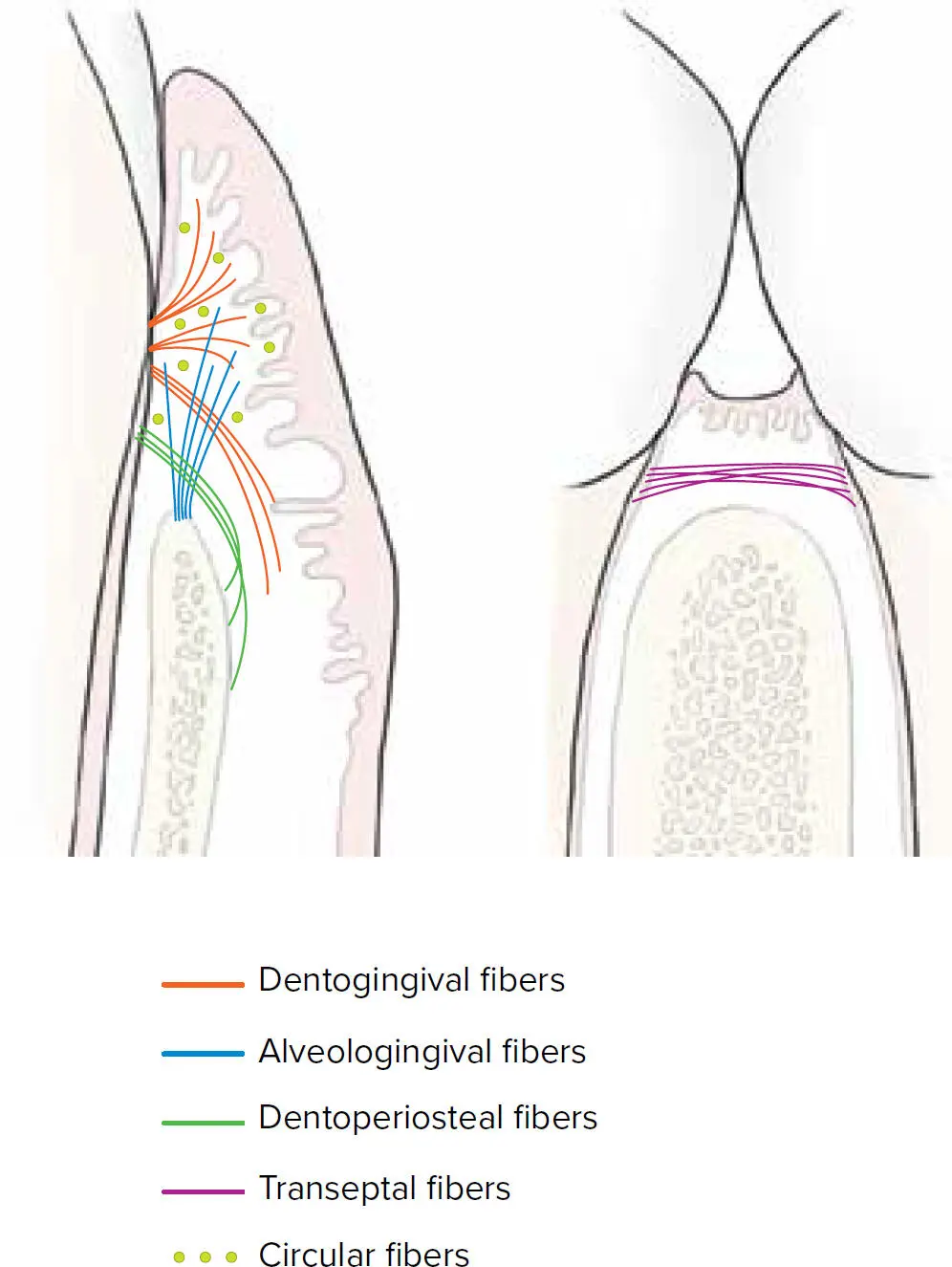
The main cell type in the lamina propria is the fibroblast, which is the main cell responsible for the formation and remodeling of the connective tissue. The main fibers of the lamina propria are comprised by collagen type I, III, IV, and V, with minor presence of elastic fibers and oxytalan fibers. The fibers in the gingiva follow a specific orientation and are classified into different bundles. The main connective tissue fibers are dentogingival, alveologingival, circular, dentoperiosteal, and transseptal ( Table 1-4and Figs 1-3 and 1-4). 5,27,28In addition, secondary connective tissue fibers are periosteogingival, interpapillary, transgingival, intercircular, semicircular, and intergingival. 29The main as well as the secondary fibers are part of the connective tissue attachment.
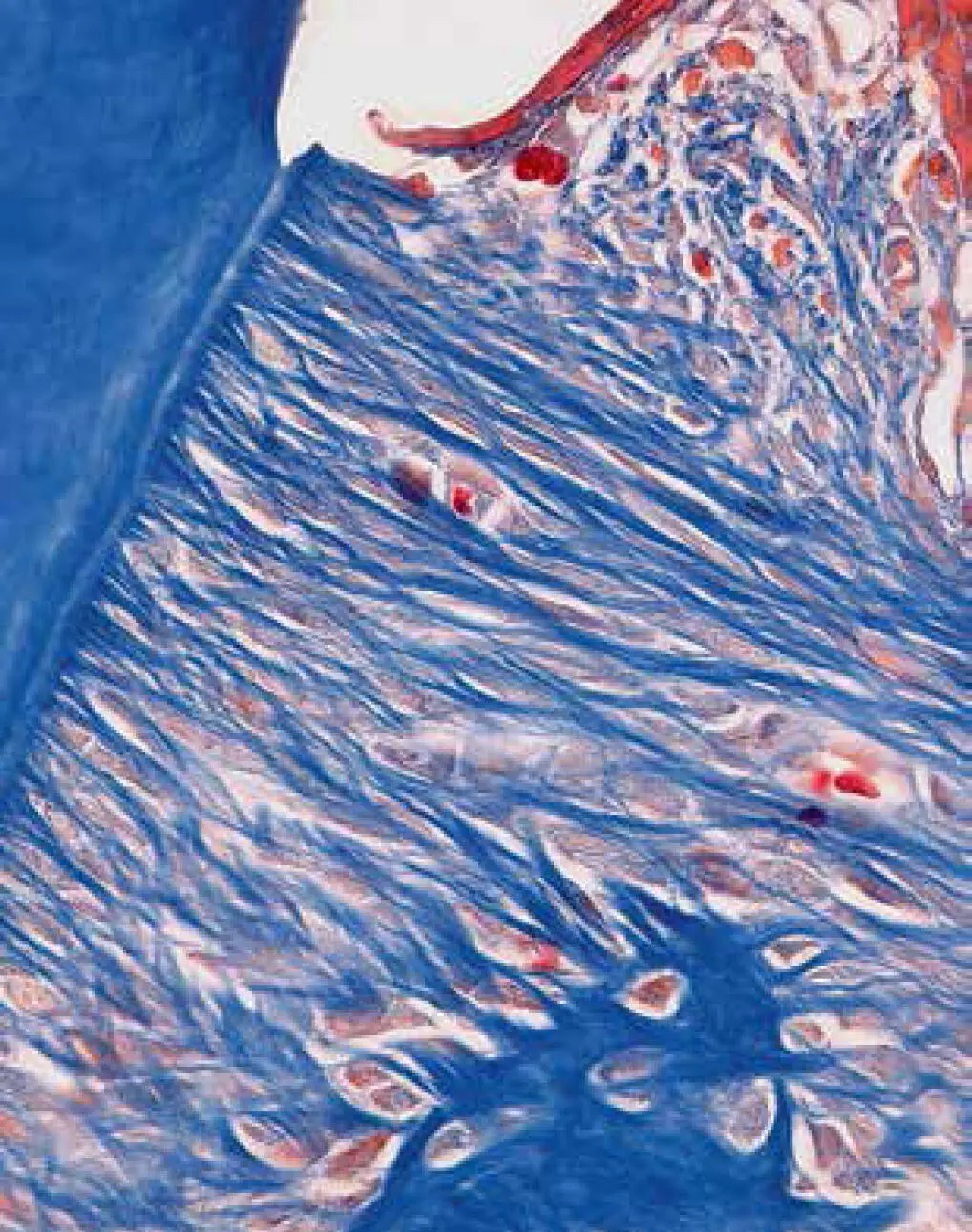
Fig 1-3 Dentogingival fibers in a mouse model (100× magnification).
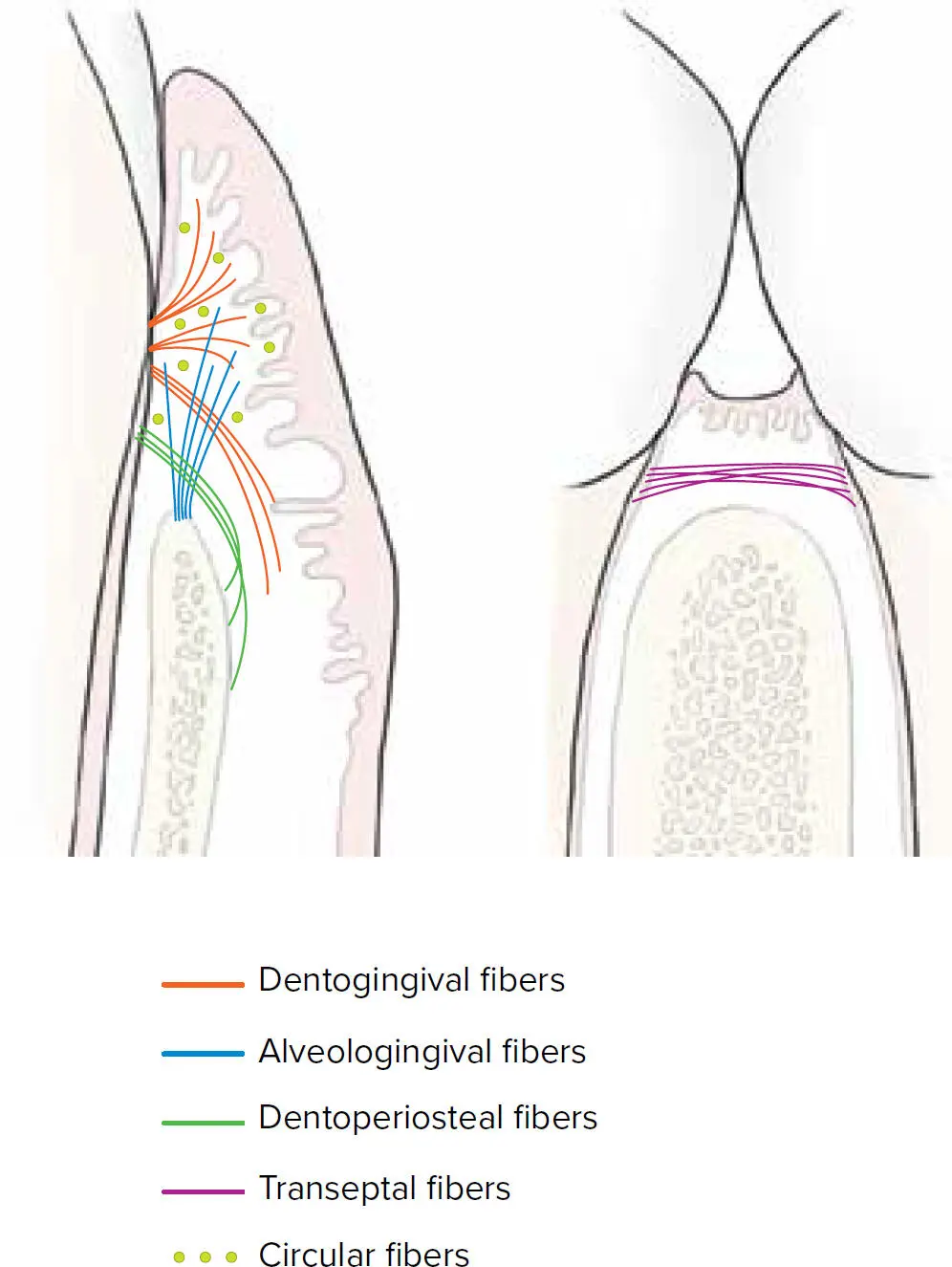
Fig 1-4 Gingival fibers.
TABLE 1-4 Main connective tissue fibers 5,28
|
Subclassification |
Origin |
Direction |
| Dentogingival fibers |
Subgroup A |
Cementum |
Free gingiva |
| Subgroup B |
Cementum |
Attached gingiva |
| Subgroup C |
Sweep down and across the crest |
NA |
| Alveologingival fibers |
NA |
Periosteum |
Free gingiva and attached gingiva |
| Circular fibers |
NA |
Encircle each tooth within the connective tissue |
| Dentoperiosteal fibers |
NA |
Cementum apical to the dentogingival fibers |
Crest of the alveolar bone. Some fibers may insert into muscles of the vestibule. |
| Transseptal fibers |
NA |
Cementum |
Cementum of adjacent tooth |
NA, not applicable.
The interface between the connective tissue and the epithelium is a specialized form of extracellular matrix named the basement membrane or basal membrane . The basal membrane consists of a highly crosslinked matrix of collagen and glycoproteins such as laminin, perlecan, and entactin, and it is composed of several layers. Under electron microscopy, three components can be differentiated: the lamina lucida, the lamina densa, and the lamina reticularis. 27
The interdental gingiva or papilla refers to the soft tissue that occupies the space between the teeth and consists of an epithelium with a subjacent dense connective tissue. The shape of this interdental gingiva is determined by the morphology of the teeth and the CEJ. In anterior sites, it presents with a pyramidal shape, whereas in posterior sites, it presents with a concave shape. The epithelium that covers this concave portion is known as the col epithelium . 28,30
SUPRACRESTAL TISSUE ATTACHMENT
The junctional epithelium and connective tissue attachment together are known as the supracrestal attached tissues (formerly referred to as biologic width). 2,31The dimensions of these structures were investigated by Gargiulo et al 32and Vacek et al 33in human cadavers reporting an average distance of 2.04 mm and 1.91 mm, respectively ( Table 1-5).
TABLE 1-5 Classic studies on the dimensions of supracrestal tissue attachment and sulcus
|
Sulcular epithelium (mm) |
Junctional epithelium (mm) |
Connective tissue (mm) |
| Gargiulo et al 32 |
0.69 |
0.97 |
1.07 |
| Vacek et al 33 |
1.34 |
1.14 |
0.77 |
A meta-analysis by Schmidt et al 34in 2013 concluded that the biologic width ranges from 2.15 mm to 2.30 mm, with posterior teeth having longer junctional epithelium and the dimension of connective tissue attachment being larger in buccal and lingual surfaces compared with interproximal sites. 34
Peri-Implant Attachment Apparatus
The replacement and restoration of the missing dentition by means of dental implants has become a routine procedure in daily practice. As such, a plethora of systems with different macro- and microstructures are available on the market. However, independently of the design, the proper functioning of dental implants is primarily based on the process of osseointegration. This phenomenon is defined as the direct contact between the surface of a loaded implant and vital bone.
Considerable differences exist between the structures giving support to dental implants and natural dentition, the most important being the lack of PDL for osseointegrated implants. However, at the most coronal portion, some similarities can be found. Similar to the supracrestal attached tissues in the natural dentition, implants also present in their most coronal portion with a sulcus epithelium, junctional epithelium, and connective tissue. 35In 1991 in an animal model, Berglundh et al 35described the differences in the arrangement of collagenous fibers in the connective tissue between teeth and implants. Essentially, while the collagenous fibers run perpendicular to the axis of the tooth, they run parallel to the surface of an implant. The composition of the connective tissue also seems to differ between implants and teeth. As such, more collagen and fewer cells have been found around dental implants in comparison with teeth. 35Moon et al 36also described that although generally a reduced number of cells have been found in the periimplant tissue, a cell-rich zone is present in the connective tissue adjacent to the implant-abutment surface with high concentration of fibroblasts.
Читать дальше