Free gingiva: The part of the gingiva that surrounds the tooth and is not directly attached to the tooth surface.
Gingival groove: A shallow, V-shaped groove that is closely associated with the apical extent of free gingiva and runs parallel to the margin of the gingiva. The frequency of its occurrence varies widely.
Gingival papilla: The portion of the gingiva that occupies the interproximal spaces. The interdental extension of the gingiva.
Hertwig epithelial root sheath (HERS): An extension of the enamel organ (cervical loop) Determines the shape of the roots and initiates dentin formation during tooth development. Its remnants persist as epithelial rests of Malassez in the periodontal ligament.
Lamina propria: In the mucous membrane, the connective tissue coat just beneath the epithelium and basement membrane. In skin, this layer is known as the dermis .
Mucogingival junction: The junction of the gingiva and the alveolar mucosa.
Osseointegration: A direct contact, at the light microscopic level, between living bone tissue and an implant.
Periodontal ligament (PDL): A specialized fibrous connective tissue that surrounds and attaches roots of teeth to the alveolar bone. Also known as the periodontal membrane .
Periodontium: The tissues that invest and support the teeth, including the gingiva, alveolar mucosa, cementum, periodontal ligament, and alveolar supporting bone. Also known as the supporting structure of the tooth .
Rete pegs: Ridge-like projections of epithelium into the underlying stroma of connective tissue that normally occur in the mucous membrane and dermal tissue subject to functional stimulation.
The periodontiumcomprises the supporting structures of the dentition. It is composed of four main elements: gingiva, cementum, periodontal ligament (PDL), and bone. Understanding this dynamic network of tissues is pivotal for the proper performance of the many procedures related to periodontal therapy. This chapter describes the different structures of the periodontium from microscopic and macroscopic points of view.
The attachment apparatus, also known as periodontal attachment , is an aggregate of tissues with the main function of anchoring teeth to the alveolus. It consists of cementum, alveolar bone, PDL, and gingiva. Several terms are highly relevant with this regard and are described by the American Academy of Periodontology (AAP) Glossary of Periodontal Terms (see sidebar). 1
Periodontium: Attachment Apparatus
PERIODONTAL LIGAMENT
The PDL is a specialized connective tissue located between the bony walls of the dental socket and the dental root. It surrounds the majority of the dental root and attaches the teeth to the alveolar bone. In the most coronal portion, the PDL is continued with the lamina propria of the gingiva. Characterized by its hourglass shape, this specialized connective tissue narrows at the middle part, with an average width ranging from 0.2 to 0.4 mm. 3The PDL space decreases with age and increases under excessive load.
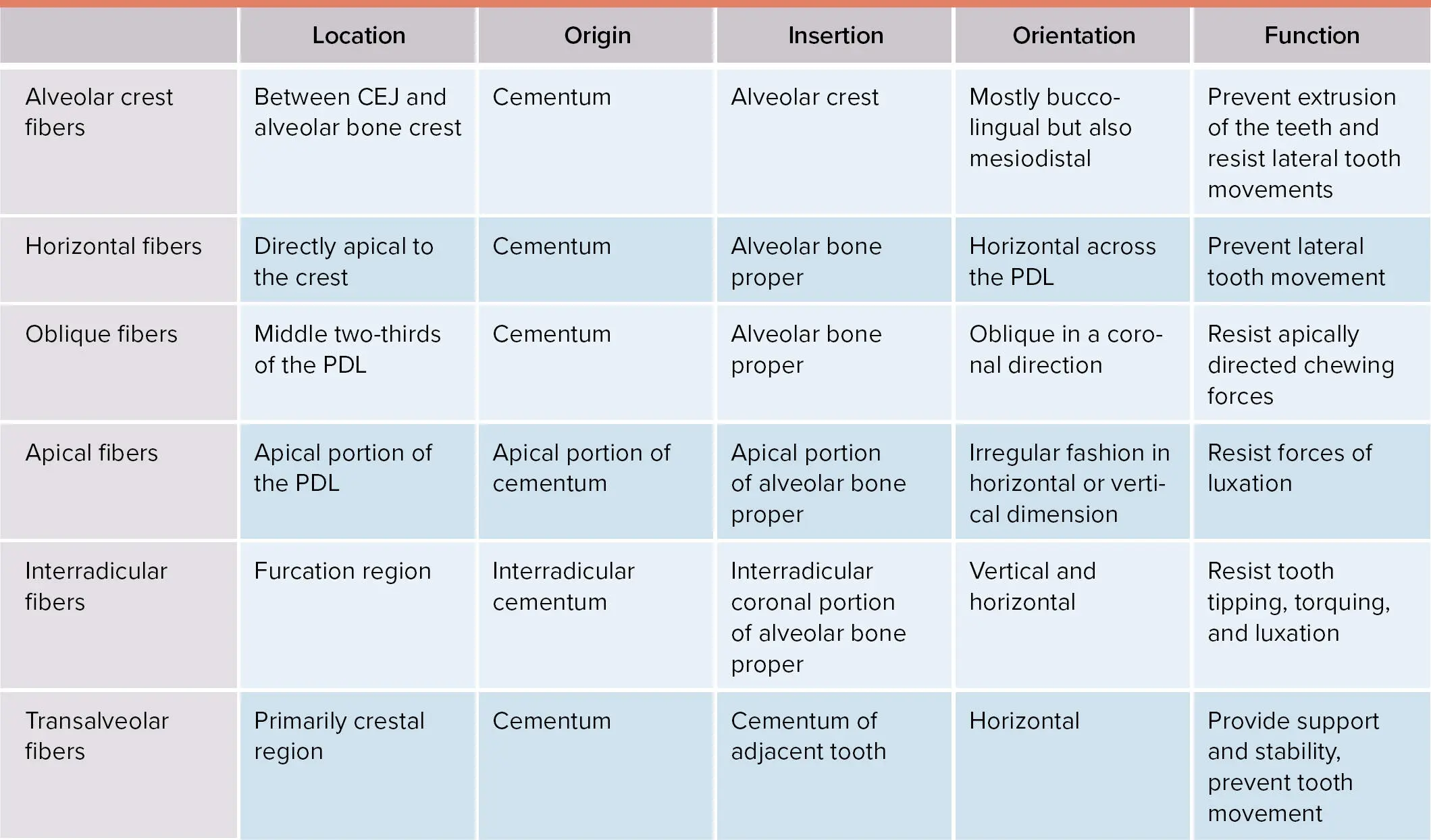
The PDL develops in a cell population from the dental follicle. As the crown approaches the oral mucosa, fibroblasts produce collagen fibrils without organized orientation. Later, prior to tooth eruption, the fibroblasts adopt an oblique orientation adjacent to the cementum. Finally, after this fibroblast arrangement, fibers with organized orientation are developed at the cementum surface as well as at the alveolar bone proper. These fibers will continue elongating until they reach each other at the middle portion of the PDL. The orientation of the fibers will be determined by the location within the PDL ( Table 1-1). 4,5
TABLE 1-1 Principal periodontal ligament fibers 4,5
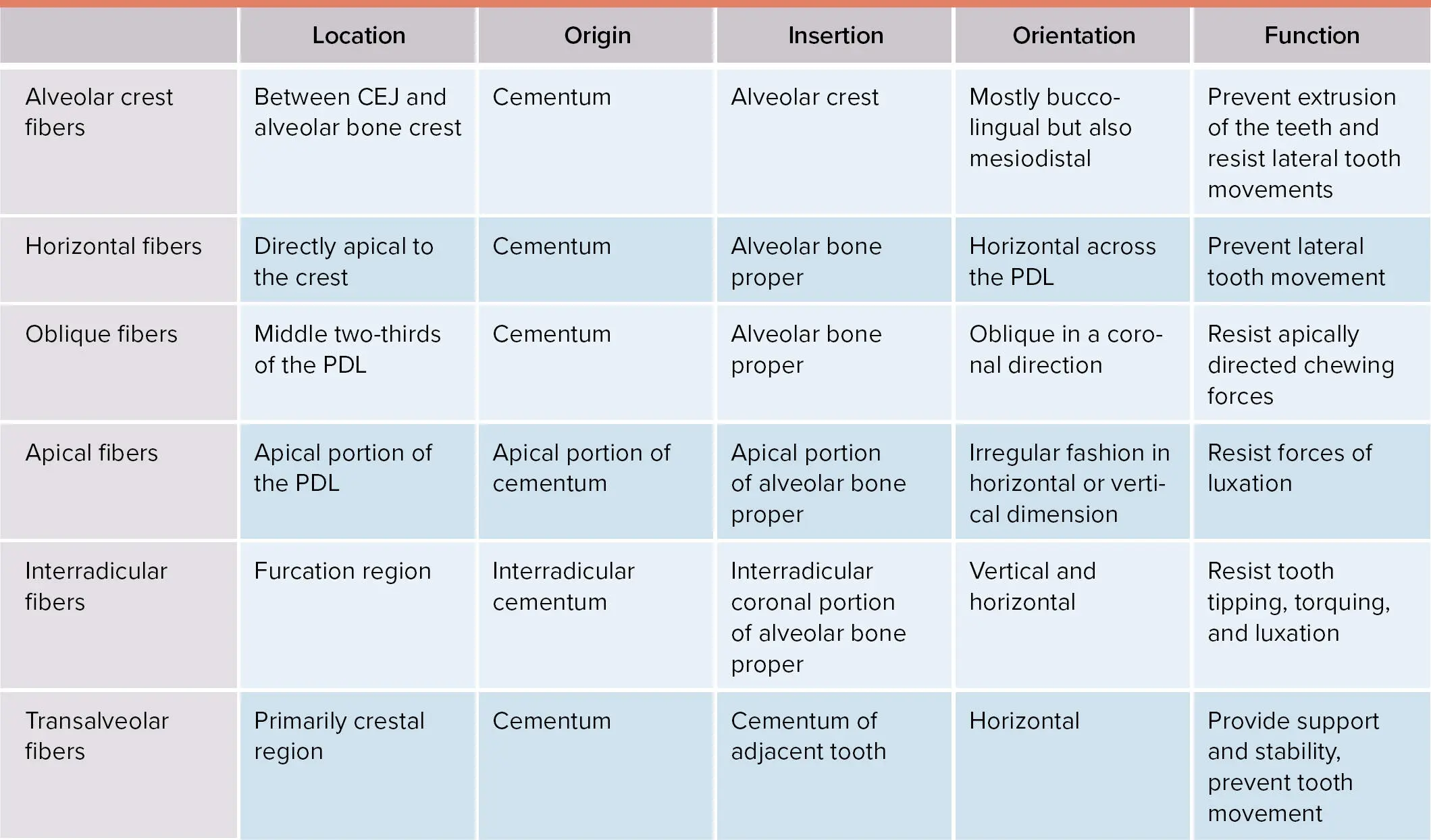
CEJ, cementoenamel junction.
The PDL is formed by different cell types. The fibroblasts are the most abundant as they are responsible for the metabolism of the extracellular components. Within this heterogeneous population of fibroblasts within the PDL, osteoblast-like fibroblasts are also present, and these are rich in alkaline phosphatase. 6,7In addition, the PDL contains stem cells, epithelial cell rests of Malassez, cells from the blood vessels, and cells associated with the immune and nervous systems.
The extracellular matrix of the PDL consists of collagenous and noncollagenous proteins. Collagen type I is the most abundant, and it is also the primary constituent of the Sharpey fibers, together with collagen II, V, VI, XII, and XIV. 8Other noncollagenous proteins present in the PDL are tenascin, fibronectin, vitronectin, elastin, and glycoproteins. In addition, hyaluronate, heparan sulfate, chondroitin sulfate, and dermatan sulfate are the glycosaminoglycans identified in the PDL. Dermatan sulfate is the principal glycosaminoglycan, while versican and decorin are the main proteoglycans. 8,9
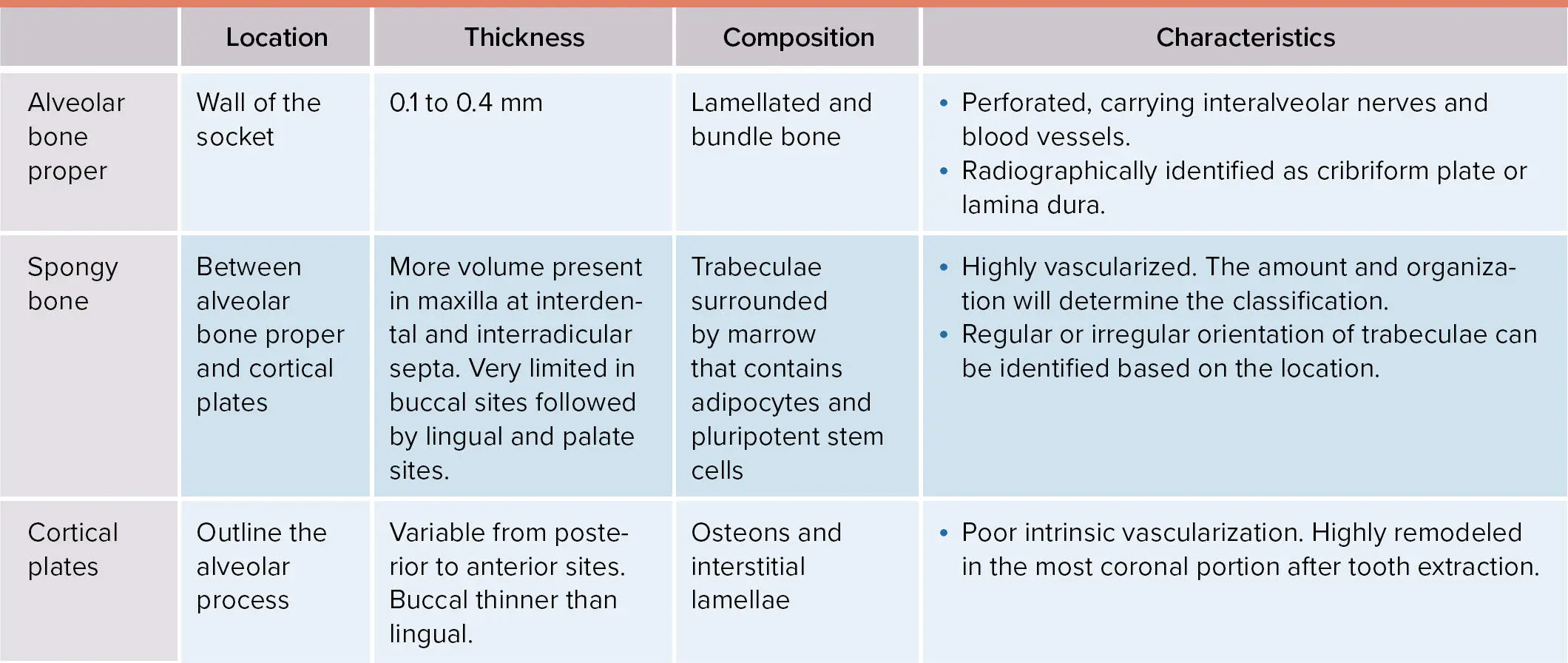
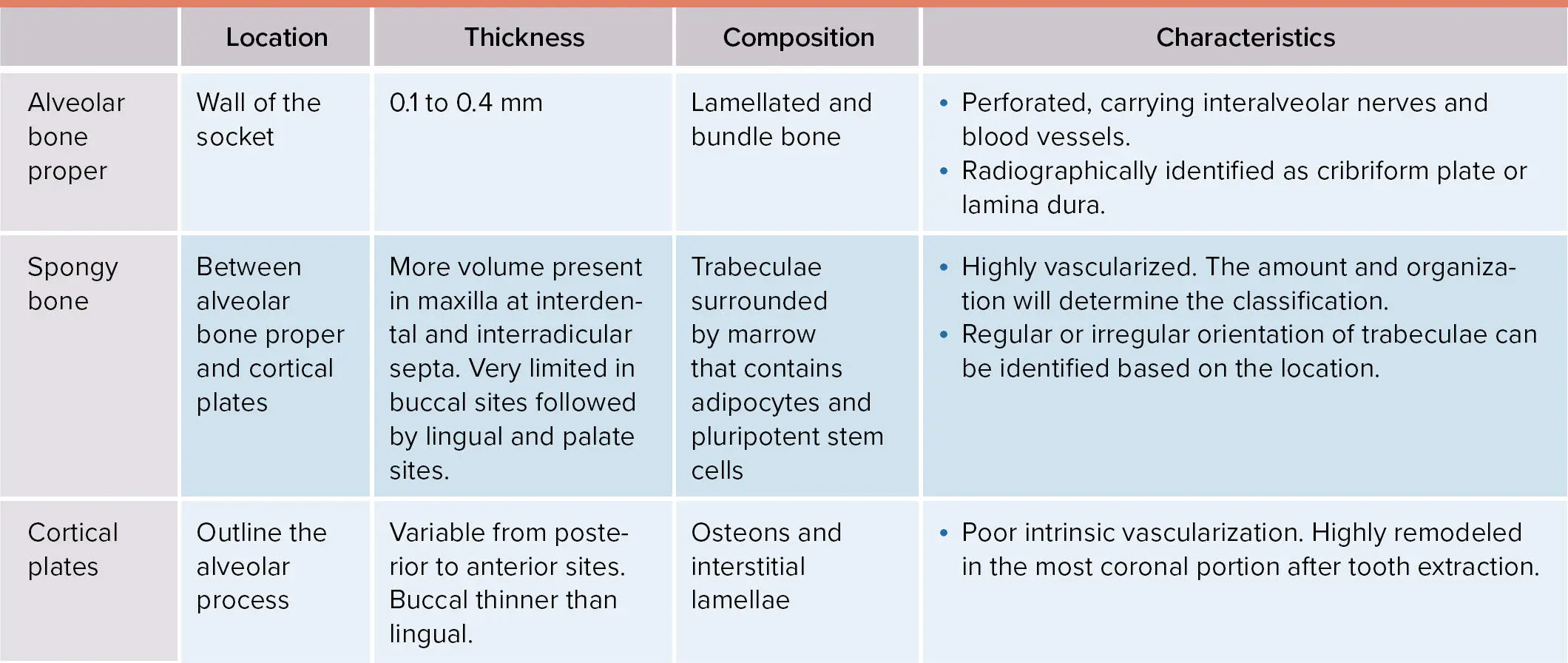
One of the two mineralized tissues that comprises the attachment apparatus is the alveolar bone. Just like any other type of bone in the human body, it is composed of a mineralized matrix and a nonmineralized connective tissue. Within the mineralized tissues, calcium is the most prevalent mineral in the form of hydroxyapatite. The alveolar bone, also known as alveolar process, consists of spongy bone, cortical plates, and the alveolar bone proper( Table 1-2). The crest of the alveolar bone refers to the most coronal portion of it, and its distance from the cementoenamel junction (CEJ) in a healthy periodontium is within the range of 1 to 3 mm.
TABLE 1-2 Features of alveolar bone
The alveolar bone is created following an intramembranous ossification with ectomesenchymal cells from the dental follicle intervening in the developmental process. The presence of teeth is essential for the development of the alveolar bone. As such, in absence of a PDL, the alveolar bone proper will not develop. 5
The alveolar bone houses the teeth, providing protection and support and allowing proper functioning during mastication, absorbing and distributing the occlusal forces. The primary function of the alveolar bone is to provide a structure where the Sharpey fibers of the PDL anchor to keep the tooth in position and function.
The chemical composition of alveolar bone is 65% hydroxyapatite and 35% organic material such as collagen and noncollagenous proteins (eg, osteocalcin, bone sialoprotein, phosphoprotein, osteonectin, and bone morphogenetic proteins).
Microscopically, two different types of mature bone can be observed based on the organization: (1) the lamellar bone, containing osteons which consist of a blood vessel surrounded by concentric lamellae, and (2) the bundle bonewhere PDL fibers (Sharpey fibers) anchor. In the bundle bone, lamellae can be found parallel to adjacent marrow spaces, and the disposition is parallel to the tooth surface.
Cementum is the second mineralized tissue of the attachment apparatus. It is an avascular mineralized connective tissue that surrounds the dentin at the level of the dental root. Its primary function is to allow for the anchorage of Sharpey fibers that will keep the tooth in the alveolus as well as to adapt and protect during tooth wear and movement. The thickness of cementum increases with age. Also, apical portions of the dental root present with thicker cementum than the coronal counterparts. 5The CEJ is the anatomical area where the crown meets the root. Schroeder and Scherle 10described three types of relationships between cementum and enamel: edge to edge; cementum covering the enamel; or a gap between both structures where dentin is exposed. The most prevalent interrelation is cementum covering the enamel, followed by edge to edge and gap. 11
Читать дальше