1 ...7 8 9 11 12 13 ...50 Left ventricular hypertrophy in the absence of secondary causes
Mismatch between ECG finding of low voltage and echocardiogram finding of left ventricular hypertrophy
Granular sparking appearance of left ventricular wall
Apical sparing
Diastolic dysfunction
Biatrial dilatation and reduced left ventricular cavity dimensions
ECG hallmarks are low voltages. Further investigations include:
sFLC ratio and serum/urine immunofixation (to investigate for AL).
Cardiac imaging (non‐invasive diagnosis)Longitudinal strain imaging using 2D speckle tracking for ‘apical sparing’ patternCardiac MRI for diffuse and subendocardial ‘late gadolinium enhancement’ pattern that does not respect coronary distributions (93% sensitive, 70% specific)99mTcPYP scintigraphy for grade 2 or 3 myocardial radiotracer uptake (100% specificity and positive predictive value, in absence of monoclonal gammopathy)
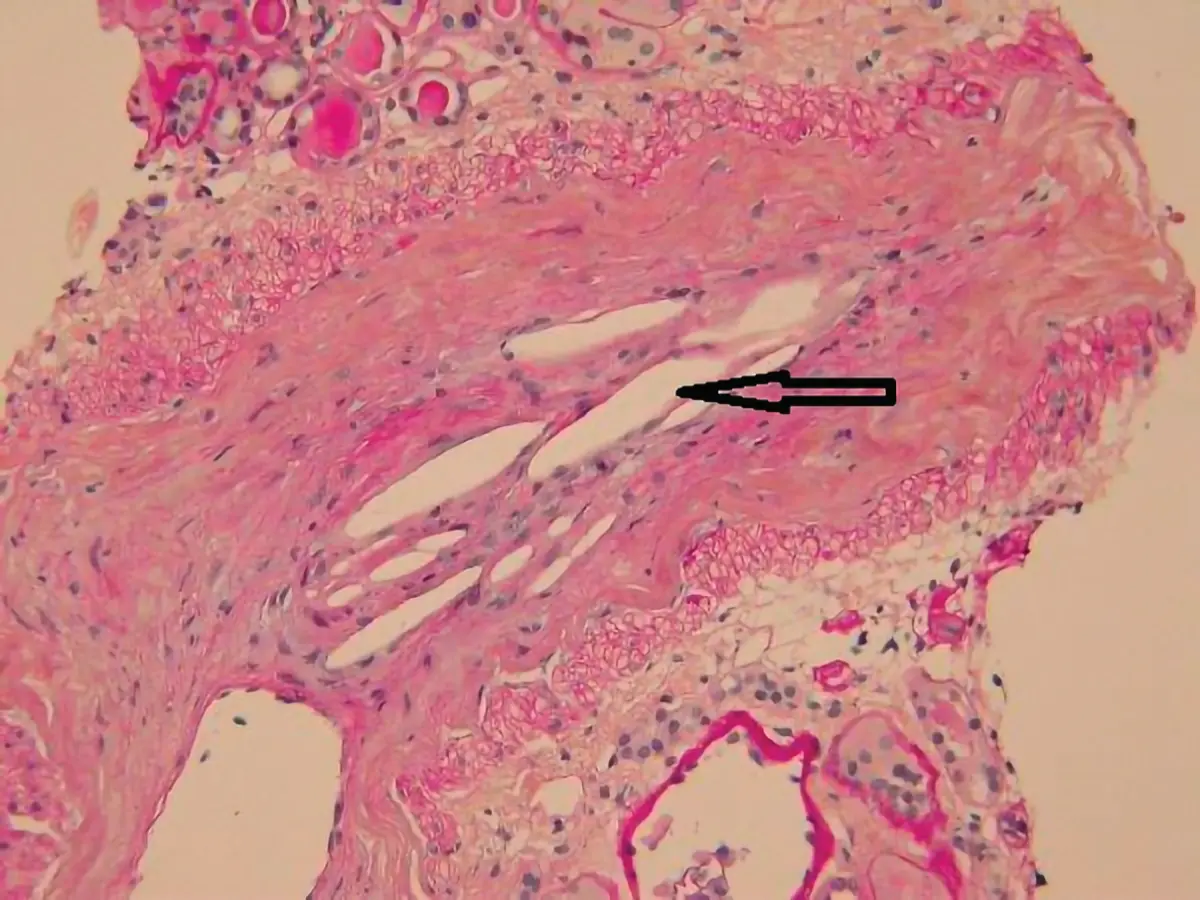
Endomyocardial biopsy (diagnostic gold standard, 100% sensitive for CA).
Definitive diagnosis of amyloidosis requires biopsy ( Table 1.3).
Table 1.3 Sensitivity of different organ biopsy in diagnosis of amyloidosis.
| Organ |
Sensitivity |
| Abdominal fat pad |
70% |
| Bone marrow |
50% to 60% |
| Clinically involved organ |
99% to 100% |
| Rectum |
70% to 85% |

Donnelly J, Hanna M. Cardiac amyloidosis: An update on diagnosis and treatment. Cleveland Clinic Journal of Medicine. 2017;84(12 suppl 3):12–26.
https://www.ccjm.org/content/84/12_suppl_3/12.long
10. Answer: A
Cardiac output is defined by the amount of blood ejected by each ventricle in one minute. Cardiac output (litres/min) is the product of the stroke volume (litres/beat) and the heart rate (beats/min). There are four determinants of cardiac output, including heart rate, preload, afterload, and contractility.
Heart rate is affected by chronotropic factors. Sympathetic stimulation by noradrenaline, adrenaline, and medications such as atropine can increase heart rate. Activation of the parasympathetic system and chemicals, such as acetylcholine and adenosine, slows down the heart rate.
Preload is the amount of blood entering the ventricle during diastole, also known as the end‐diastolic volume. It is influenced by blood volume, venous return, and atrial contraction.
Afterload occurs during systole when ventricle contracts and ejects blood out of the aorta and into the pulmonary trunk. Atherosclerosis, peripheral vasoconstriction, and hypertension increase afterload due to increased resistance.
Inotropic factors affect the contractility of the heart. Positive inotropes such as sympathetic stimulation by noradrenaline and dobutamine increases cardiac output. The parasympathetic system, acetylcholine, beta blockers, acidosis, and calcium channel blockers can have negative inotropic effect on the heart and reduce cardiac contractility.
Atropine increases heart rate, causing a higher cardiac output. Adenosine slows down heart rate hence reduces cardiac output. Hypertension increases the force against which the ventricles must pump in order to eject blood, hence reducing cardiac output. Beta blockers have negative inotrope effect and also slow down the heart rate, resulting in decreased cardiac output.
Acidosis reduces left ventricle contractility. However, this is compensated for by an increased heart rate and a reduced systemic vascular resistance, resulting in an increased cardiac output.

Vincent J. Understanding cardiac output. Critical Care. 2008;12(4):174.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2575587/
11. Answer D
Episodic loss of consciousness is most commonly caused by cardiac syncope, reflex syncope, orthostatic syncope, and less commonly seizure. Clinical features present on history, examination and basic investigation findings can be useful in determining the likelihood of various causes, although no individual feature is diagnostic for a particular cause.
Patient features that increase the likelihood of cardiac syncope are increasing patient age, history of atrial fibrillation or flutter, history of cardiac failure, and history of severe structural heart disease. Some precipitating factors can decrease the likelihood of cardiac syncope, such as syncope in a warm place, during a medical procedure, or after using the toilet. Dyspnoea or chest pain prior to syncope are associated with higher likelihood of cardiac syncope, whereas cold sensitivity, headache, mood change, and abdominal discomfort decrease the likelihood of cardiac syncope. Witnessed cyanosis is associated with higher likelihood of cardiac syncope, whereas inability to remember details prior to the episode and mood changes after the episode are associated with lower likelihood of cardiac syncope. A combination of normal ECG and no history of cardiac disease is associated with a lower likelihood of cardiac syncope. Contrary to popular teaching, the presence or absence of injury does not predict for or against cardiac syncope.
Two clinical scores, Evaluation of Guidelines in SYncope Study (EGSYS) and vasovagal score), assign scores on the basis of a combination of clinical factors and have some predictive value over and above individual patient characteristics. EGSYS uses six patient variables and a score less than three has a likelihood ratio of cardiac syncope of 0.12–0.17. The vasovagal score has only been prospectively evaluated in one study but a cut‐off score of less than –2 has likelihood ratio of over 8 for cardiac syncope and equal to or more than –2 has a likelihood ratio of 0.10, making this score a potentially good discriminator, if results can be duplicated.
Biomarkers are not yet utilised in widespread practice for the evaluation of syncope, but there is some evidence that high‐sensitivity troponin and N‐terminal pro‐B‐type natriuretic peptide may become useful in ruling out cardiac syncope.
Several clinical features have high specificity, but low sensitivity for the diagnosis of seizure. These include head turning during the event, unusual posturing during the event, urinary incontinence, tongue trauma, and the patient having no recall of witnessed unusual behaviours.
Albassam O, Redelmeier R, Shadowitz S, et al. Did This Patient Have Cardiac Syncope? JAMA. 2019;321(24):2448.
https://jamanetwork.com/journals/jama/article‐abstract/2736568
12. Answer: C
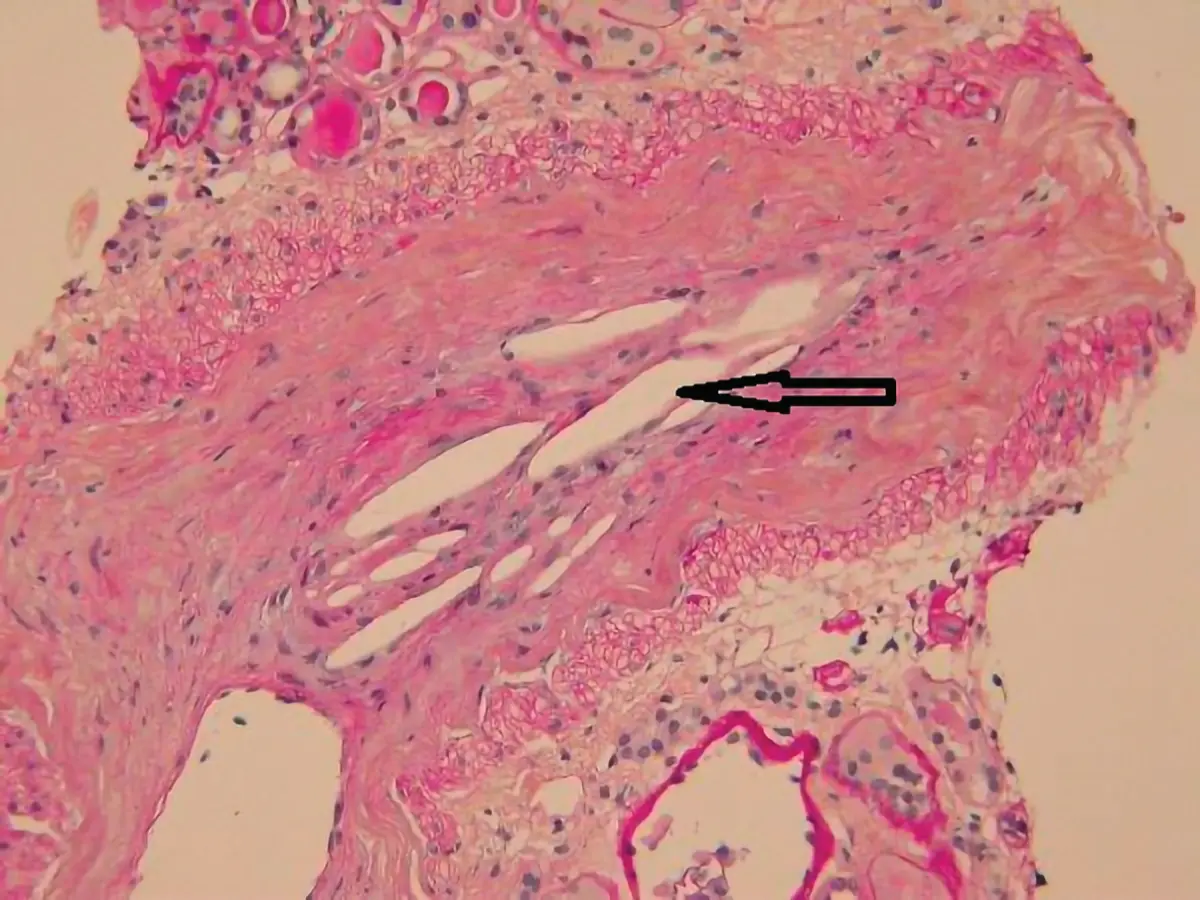
This patient's clinical features, unexplained fever, myalgia, sudden appearance of several small, cool, cyanotic and painful areas of the toe, and AKI are consistent with cholesterol embolisation. Cholesterol embolism is caused by showers of cholesterol crystals from an atherosclerotic plaque that occludes small arteries. Embolisation can occur spontaneously or as an iatrogenic complication from an invasive vascular procedure (angiography or vascular surgery) and after anticoagulant therapy as a result of interference with the protective clot over ulcerative atheromatous plaques and thrombolytic therapy may lyse thrombi, including those covering atherosclerotic plaques.
Читать дальше