FIG 2-3A vibration anesthesia device (Blaine Labs) achieves its effect through stimulation-induced analgesia and muscle relaxation.
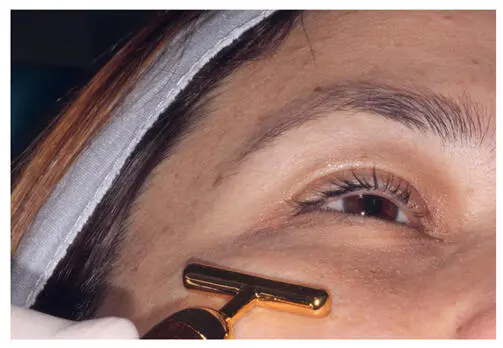
FIG 2-4Vibration anesthesia device applied concurrently with anesthesia injection.
Topical anesthesia
Topical anesthetics offer the same nerve-blocking qualities as injectables and can increase patient comfort when used separately or in conjunction with injectable anesthetics. 7 Lidocaine, alone or in combination with another anesthetic, is the most widely used topical anesthetic. 8 Today, many commercially prepared dermal fillers add lidocaine to the product, allowing patients with high resistance to pain the option to receive topical anesthetics alone in lieu of injectable anesthetics.
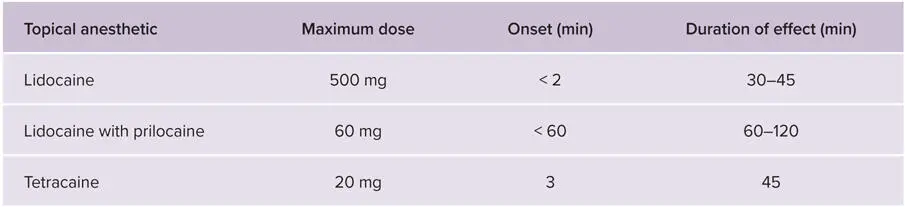
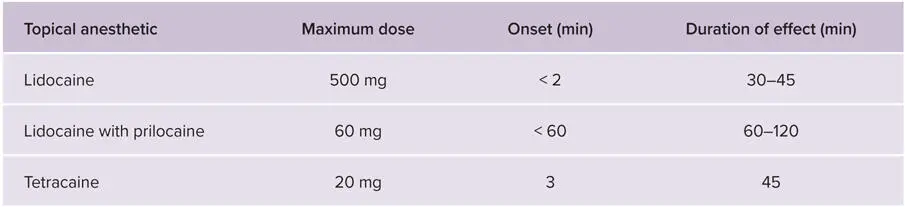
The effectiveness of a topical anesthetic depends on the depth of skin penetration, the location of the skin surface, the length of exposure time, and the concentration of the ingredients ( Table 2-1). 8 Table 2-2lists several properties of different topical anesthetic types. 9 The topical anesthetic favored by the authors is a compounded formula of 10% benzocaine, 20% lidocaine, 10% tetracaine (commonly referred to as BLT and widely used in cosmetic procedures 1 ), and 10% dimethyl sulfoxide (DMSO) in a Lipoderm (Professional Compounding Centers of America) base. DMSO is added to the standard formula not only for its anti-inflammatory effects, but also because of its capacity to rapidly and easily penetrate the skin. This formula can be ordered from any compounding pharmacy. 2 Most topical anesthetics take effect within 15 minutes of administration of a 0.5-mg dose.
TABLE 2-1Formulas for commonly used topical anesthetics
| Name |
Ingredients |
| LMX4 (Eloquest) |
Lidocaine 4% |
| EMLA |
Lidocaine 2.5%, prilocaine 2.5% |
| BLT plus (compounded formula) |
Benzocaine 10%, lidocaine 10%, tetracaine 10%, dimethylsulfoxide 10% in Lipoderm (Professional Compounding Centers of America) base |
TABLE 2-2Properties of topical anesthetics 9
Few complications are associated with the use of topical anesthesia ( Table 2-3). 8 For facial dermal filler procedures, topical anesthetic is applied on a relatively small surface area, and therefore the risk of toxicity is minor. The risk of this complication increases when these agents are used on larger surface areas, such as in certain laser treatments. 8 When using a compounded formula, it is extremely important to know whether the compounding pharmacy is formulating the anesthetic with phenylephrine because this can affect dosing (as can tetracaine, the ingredient most commonly associated with toxic dosing). The addition of phenylephrine, a vasoconstrictor, reduces the risk of systemic toxicity. 7,10,11
TABLE 2-3Complications associated with topical anesthesia
| Adverse event |
Signs and symptoms |
| Allergic reaction |
Pruritis and papules locally, and the remote possibility of urticaria, angioedema, and anaphylaxis |
| Lidocaine toxicity of the central nervous system |
Dizziness, tongue numbness, tinnitus, diplopia, nystagmus, slurred speech, seizures, respiratory distress |
| Lidocaine toxicity of the cardiovascular system |
Arrhythmias, hypotension, cardiac arrest |
| Tetracaine toxicity of the central nervous system |
Restlessness, agitation, seizure activity |
| Methemoglobinemia caused by lidocaine, tetracaine, or prilocaine |
Cyanosis, acidosis |
In the authors’ practices, most patients receiving dermal filler treatments begin with a microdermal needling procedure for dermal rejuvenation of the entire face. As described in chapter 6, a topical anesthetic is applied before microdermal needling. For patients who have a high pain tolerance, dermal filler treatments can proceed without the need for injectable anesthetics for all of the areas covered in this text with the exception of the lips, which are highly sensitive and generally require a lip ring block prior to dermal filler treatment (see chapter 10). 2 Depending on their size and depth, scars and frown lines can be treated using only a topical anesthetic in most patients.
Topical anesthetic procedures begin with the application of alcohol to remove skin oils and to boost the penetration of the anesthetic. The anesthetic can then be rubbed directly on the skin either with gloved hands or a cotton applicator (Fig 2-5). Alcohol is used again to remove the anesthetic once the nerve-blocking effect has been achieved.

FIG 2-5A topical anesthetic cream will generally take effect within about 5 minutes and last at least 30 minutes, depending on the formulation.
Injectable Anesthesia
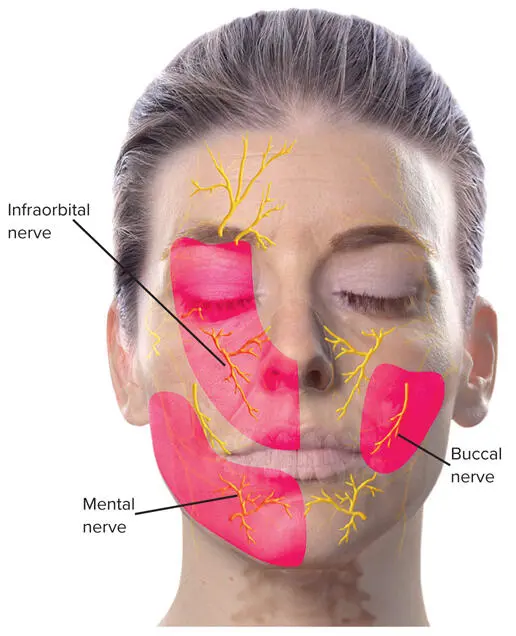
Administering anesthesia injections is obviously within the scope of every dentist’s daily practice. However, because the target of the anesthesia is the facial nervous system rather than the oral cavity, the dentist should thoroughly review the anatomy of the face, with special emphasis on the innervation location of each injection site in the facial nervous system network (Fig 2-6).
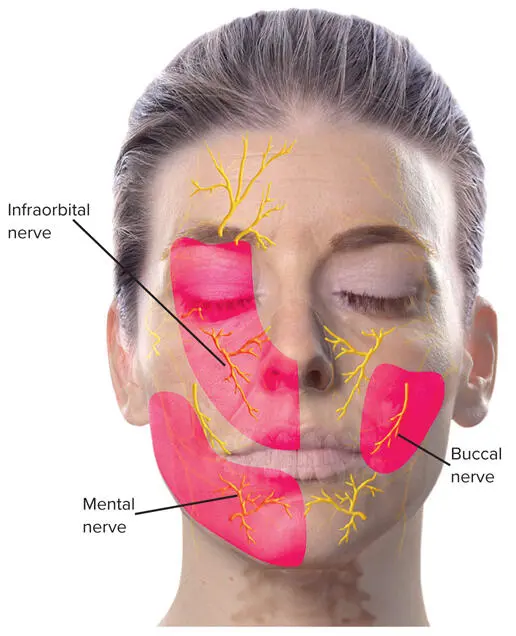
FIG 2-6Sensory nerves of the face. As most dentists know, the distal portion of the inferior branch of the infraorbital nerve services the upper lip; however, the superior branches of the nerve service the medial cheek, lateral nose, and lower eyelid. Similarly, the mental nerve services the lower lip, but the distal portion of the buccal nerve services the corners of the lips. The infraorbital and mental nerves stretch vertically from the mandible to the supraorbital notch located along the upper border of the orbit. These nerves are detectable roughly 2.5 cm lateral to the midline of the face. The infraorbital foramen can be reached about 1 cm inferior to the infraorbital bony margin, whereas the mental foramen can be detected 1 cm above the mandibular margin.
Complications from injections range from patient anxiety and fainting to bruises, infections, and allergic reactions. Toxicity from the anesthetic is almost nonexistent because of the low doses given, but accidental injections to nerve or blood vessels could lead to nervous system or cardiovascular system toxicity, with possible serious results (eg, respiratory distress, cardiac arrest; Box 2-1). 1
BOX 2-1Complications associated with injectable anesthesia
Bruising
Infection
Nerve injury
Allergic reactions
Lidocaine toxicity of the central nervous system
Lidocaine toxicity of the cardiovascular system
Epinephrine adverse response
Local infiltration and ring blocks are the two most common methods of administering injectable lidocaine in small doses (0.5 to 6.0 mL). Local infiltration of a solution of 0.1-mL buffered lidocaine with epinephrine is used for most of the procedures covered in this text (Figs 2-7 and 2-8). It usually requires a series of 3 to 6 subcutaneous injection sites, which should raise the skin slightly but not dimple it. The maximum dose that should be given to an adult according to body weight is 4.5 mg/kg for lidocaine without epinephrine and 7 mg/kg for lidocaine with epinephrine. 9 Patients who are especially anxious or who have a low pain threshold for needle injections can be preemptively treated with any of the noninvasive anesthetic techniques described earlier. Alternatively, the clinician can apply a topical anesthetic about 15 minutes prior to treatment.
Читать дальше