Istvan Urban 2021
Introduction Introduction 1 The biology of vertically and horizontally augmented bone Vertical bone growth is very challenging, both biologically and technically. A recent meta-analysis by Urban et al 1 found that, regardless of the technique, about 4.5 mm of vertical bone gain was achieved in the included studies. However, complications occur least frequently when the guided bone regeneration (GBR) technique is used. The results of this study indicate the advantage of using GBR. The technical challenge of GBR is discussed extensively in this book, while the biologic challenge that may play a role in limiting vertical bone gain is discussed in this chapter. Based on the author’s experience, the amount of vertical bone gain is not limited by biology, but more by the clinician’s abilities. The biologic background of vertical bone gain was investigated by the author in preclinical settings.
Chapter 1 The biology of vertically and horizontally augmented bone
Chapter 2 Scientific evidence of vertical bone augmentation utilizing a titanium-reinforced polytetrafluoroethylene mesh 2 Scientific evidence of vertical bone augmentation utilizing a titanium-reinforced polytetrafluoroethylene mesh Introduction This chapter examines how a dense polytetrafluoroethylene (d-PTFE) mesh was investigated in the author’s clinical practice. The primary study objectives were: 1. To evaluate the amount of bone height gain in millimeters and as a percentage of the baseline deficiency as a result of vertical bone augmentation (VBA) using a titanium-reinforced PTFE mesh (RPM) with mixed autogenous and anorganic bovine bone mineral (ABBM) particulate grafts. 2. To examine the influence of defect location, baseline deficiency extent, and membrane exposure on augmentation height. 3. To report the incidence of surgical and postsurgical complications associated with this treatment.
The extreme vertical defect of the posterior mandible
Chapter 3 Reconstruction of the extreme posterior mandibular defect: surgical principles and anatomical considerations
Chapter 4 Reconstruction of an advanced posterior mandibular defect with scarred tissue
Chapter 5 Reconstruction of an advanced posterior mandibular defect with narrow basal bone
Chapter 6 Reconstruction of an advanced posterior mandibular defect with incomplete periodontal bone levels: the ‘pawn sacrifice’
Chapter 7 Reconstruction of an advanced posterior mandibular defect with the Lasagna technique using low-dose bone morphogenetic protein-
Anterior mandibular vertical augmentation
Chapter 8 Reconstruction of the advanced anterior mandibular defect: surgical principles and anatomical considerations
Chapter 9 Reconstruction of the advanced anterior mandibular defect: considerations for soft tissue reconstruction and preservation of the regenerated bone
Chapter 10 Reconstruction of the advanced anterior mandibular defect: importance of horizontal bone gain
Posterior maxilla
Chapter 11 Long-term results of implants placed in augmented sinuses with minimal and moderate remaining alveolar bone
Chapter 12 Difficulties and complications relating to sinus grafting: hemorrhage and sinus septa
Chapter 13 Difficulties in sinus augmentation and posterior maxillary reconstructions: missing labial sinus wall and ridge deficiencies
Chapter 14 Sinus graft infection and postoperative sinusitis
Chapter 15 The reconstruction of an extreme vertical defect in the posterior maxilla
Anterior maxillary vertical augmentation
Chapter 16 Introduction and clinical treatment guidelines
Chapter 17 Complex reconstruction of an anterior maxillary vertical defect
Anterior maxillary defect
Chapter 18 Extreme defect augmentation in the anterior maxilla
Soft tissue reconstruction in conjunction with bone grafting
Chapter 19 Reconstruction of a natural soft tissue architecture after bone regeneration
Chapter 20 The labial strip gingival graft
Chapter 21 The double strip graft
Chapter 22 Large open-healing connective tissue graft
Reconstruction of the interimplant papilla
Chapter 23 The double connective tissue graft
Chapter 24 The Ice-cube connective tissue graft
Chapter 25 The Iceberg connective tissue graft
Interproximal bone and soft tissue regeneration
Chapter 26 Vertical periodontal regeneration in combination with ridge augmentation
Ultimate esthetics
Chapter 27 Reconstructionof the bone and soft tissue in conjunction with preserving the mucogingival junction
Chapter 28 Complications
Introduction
1
The biology of vertically and horizontally augmented bone
Vertical bone growth is very challenging, both biologically and technically. A recent meta-analysis by Urban et al 1found that, regardless of the technique, about 4.5 mm of vertical bone gain was achieved in the included studies. However, complications occur least frequently when the guided bone regeneration (GBR) technique is used. The results of this study indicate the advantage of using GBR. The technical challenge of GBR is discussed extensively in this book, while the biologic challenge that may play a role in limiting vertical bone gain is discussed in this chapter. Based on the author’s experience, the amount of vertical bone gain is not limited by biology, but more by the clinician’s abilities.
The biologic background of vertical bone gain was investigated by the author in preclinical settings.
The histology of polytetrafluoroethylene (PTFE) membranes in an in vivo setting
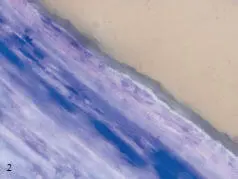
The mucogingival tissue is primarily characterized by a moderate vascularized fibrotic reaction that surrounds the PTFE membrane. The membrane is usually internally and externally surrounded by connective tissue that is rich in fibers and poor in cells, with the fibers oriented parallel to the membrane. Membrane pores, if present, show the presence of a highly vascularized matrix of connective tissue and a dense network of collagen fibers that penetrates across the pores to fix on the internal side of the membrane or, in some cases, to the newly formed bone.
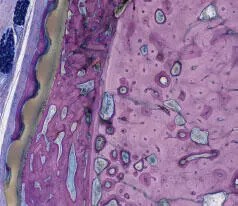
The inner layer, which is composed of expanded PTFE (e-PTFE), is always placed against the bone of the lingual and buccal sides. A slight number of macrophages admixed with a few lymphocytes, polymorphonuclear cells, giant cells/osteoclasts, and plasma cells were observed around the membrane. Deep at the lingual side of the ridge, the membrane was often in direct contact with the bone tissue, even showing slight signs of osteointegration ( Figs 1-1
to 1-4
).

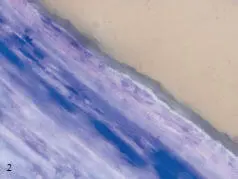
Figs 1-1 and 1-2 Parallel-oriented fibers around the membranes.
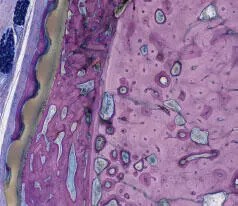
Fig 1-3 The membrane shows signs of osseointegration on both sides. Note the excellent biocompatibility of the polytetrafluoroethylene (PTFE) membrane.
Читать дальше