In case of heavy nicotine consumption (more than 10 cigarettes per day), the extensive use of xenogenic bone substitute materials in combination with membrane techniques should be avoided, as wound healing complications are more likely to occur due to reduced vascularization and therefore loss of the augmented areas. 6
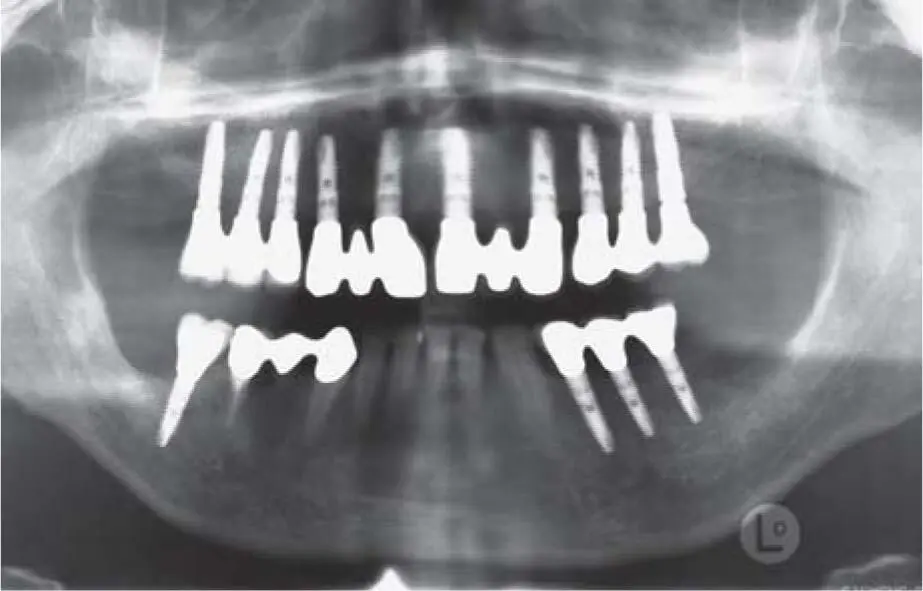
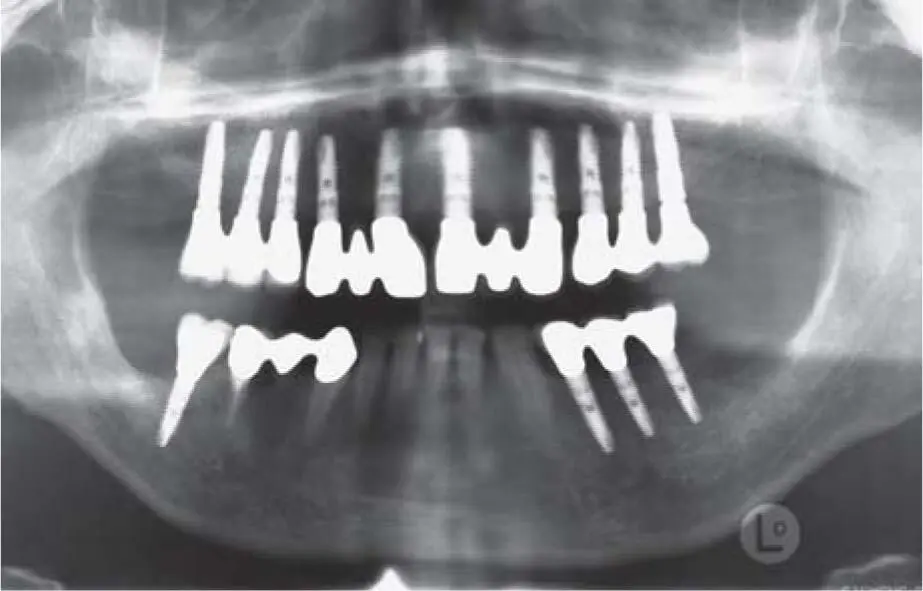
Fig 2-3bSituation after an implant prosthetic restoration with three-unit FPDs after extensive reconstruction of the alveolar crest by autogenous grafting procedure.
Nicotine use is not a contraindication for bone augmentation, but patients should be aware of the overall increased risk of complications. 3For the surgical procedure, the focus should be on minimally invasive methods such as the tunnel technique or the vestibular incision technique (see Chapter 8on risks and complications).
2.3.2 General medical findings
Among general medical conditions, diseases with a direct impact on bone metabolism are still the greatest risk group for implant therapy, especially in combination with bone grafting. Most patients in western society do not exercise enough and many of them suffer from degeneration of the skeletal system, especially due to hormonal changes and advanced age. Today, osteoporosis is considered to be one of the most severe diseases, with the risk of life-threatening vertebral body factors 35( Fig 2-4a). Hints that the blood levels of cholecalciferol (vitamin D) is low are soft bone structures in preoperative radiographs or increased bone resorption. 19In such cases, medication is administered, which is specified in three different stages. 36The least risky and most beneficial for implant placement consists of calcium and vitamin D supplements. Newer drug approaches follow the application of strontium preparations, which have a positive effect on bone metabolism, as bone resorption is inhibited, and the formation of new bone is promoted. In such instances, however, negative phenomena can occur in the area of the oral mucosa, which can then lead to peri-implant mucosal changes if the medication continues ( Fig 2-4b).

Fig 2-4aDensitometry in case of osteoporosis with below-average bone density values in the area of the spine.
2.3.2.1 Antiresorptive therapy
To inhibit osteoclast activity, antiresorptive therapy using bisphosphonate or RANKL inhibitors is available. 83The range of increased performance bisphosphonate drugs has increased in the past few decades. In addition, the human RANKL antibody Denosumab (Prolia) was approved in 2010 for the treatment of postmenopausal osteoporosis. As a subcutaneously administered drug, it extends the possibility of individualized osteoporosis medication, also interfering in bone metabolism. 87
To reduce the risk of occurrence of osseous disseminations, e.g. in patients with breast and prostate carcinomas and with multiple myeloma, a high dose of bisphosphonates is given. For these tumors, a high rate of new disease (antiresorptive drug-related osteonecrosis of the jaw – ARONJ) is continually observed every year. 31Usually, intravenously administered bisphosphonate therapy, which is used curatively as well as palliatively, means a reduction in the consequences of the oncological disease for these patients, since further metastasis growth in the bone is reduced. 31Since metastasis needs the help of the osteoclasts to remove bone, allowing for their growth, the strong inhibition of the osteoclasts will stop bone resorption: metastasis cannot grow inside the bone any longer.

Fig 2-4bAphthoid mucosal lesion on the planum buccale and on the fixed mucosa on the alveolar ridge in osteoporosis-induced strontium therapy (Protelos).
Due to the change in bone metabolism, a careful dental examination is recommended to perform invasive dentoalveolar surgery prior to medication in order to avoid osteonecrosis in the oral cavity.
Osteoporosis is a disease that shows an increasing prevalence with increasing life expectancy, especially in females. If left untreated, it leads to a significant impairment of the quality of life of those affected. In Germany, a prevalence of 6.3 million people with osteoporosis is assumed, with an incidence of 885,000 new cases per year. 35Bisphosphonate therapy for osteoporosis is administered through a weekly oral intake or a quarterly or yearly intravenous injection that lead to a stabilization of the skeletal system. A short-term intake of bisphosphonates shows no increased risk of osteonecrosis. After an intake of the medication for longer than 3 years, a higher prevalence of osteonecrosis as well as other general medical side effects are evidenced. 80Classic open wound healing is absolutely contraindicated, especially after tooth extraction, due to extremely high risk of infection. In addition, after other dentoalveolar surgery, reduced bone regeneration is observed, and the risk for sequestration of the infected bone can occur 31( Fig 2-5aand b).

Fig 2-5aBisphosphate-induced osteonecrosis in plasmacytoma with colonization of multi-resistant hemolyzing streptococci.
In this context, a few years ago, the systemic intake of bisphosphonates for the treatment of oncological disease or in osteoporosis was an absolute contraindication. Clinical experience shows that this contraindication needs to be reevaluated. 16,25Bisphosphonate medication interferes with the physiology of bone metabolism, thereby limiting the function of the osteoclasts responsible for the bone resorption and remodeling processes. 89Accordingly, the indication for techniques that require high osteoclastic activity for the remodeling must especially be reevaluated. In this case, techniques that involve the transplantation of autologous spongiosa are preferable to those that transplant purely cortical bone or xenogeneic bone substitute material that requires higher resorption kinetics to achieve a stable implant site. 20
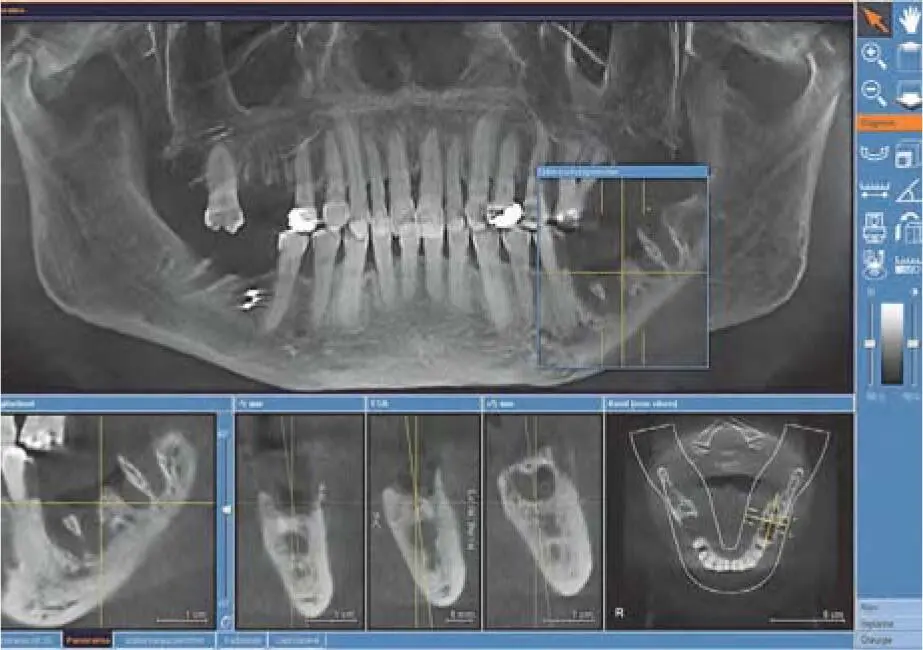
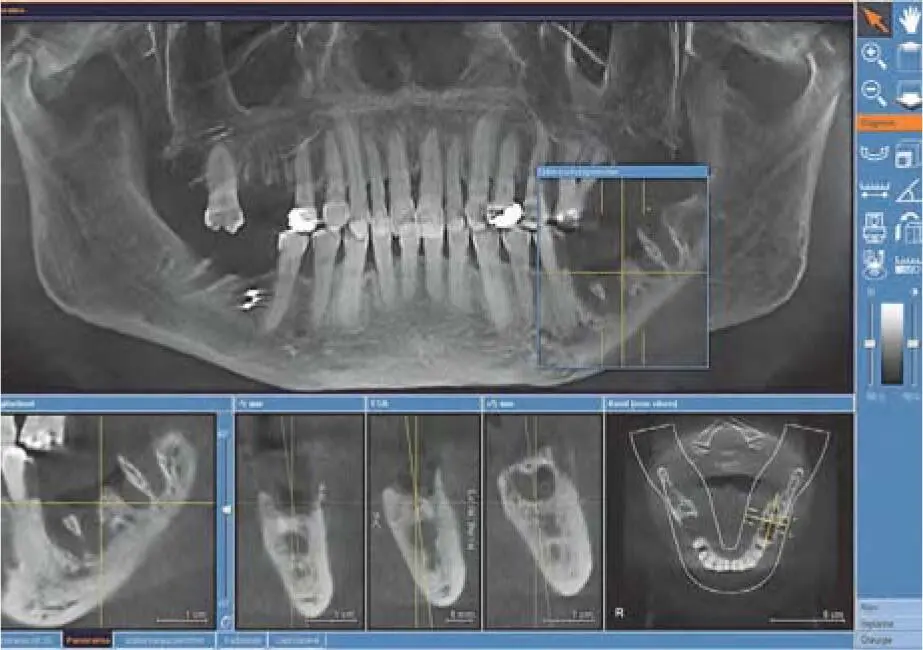
Fig 2-5bCBCT evaluation of the available bone with contraindications for augmentation and implant therapy due to osteonecrosis of the jaw (ONJ).
For oncology therapy with regular infusions ranging from a few months to a few years, implant placement should be avoided. 31Even with long-term oral administration or intravenous administration in the form of so-called ‘depot injections’ of these preparations, the critical limit is set at 3 years. To avoid bisphosphonate-induced bone necrosis in patients receiving treatment for osteoporosis, a very strict indication for augmentation and implant therapy is recommended for these patients. 31,34
Since the success of implant therapy with bisphosphonate therapy is controversial, 42,87the extent of treatment should be determined on an individual basis, depending on the patient’s health and dental history.
2.3.2.2 Specific antibody therapy
Читать дальше