Nutrition becomes the controlling factor in the development of chronic degenerative diseases.
A detailed description of the Asian dietary model and a sample menu plan can be found in Appendix B.10.
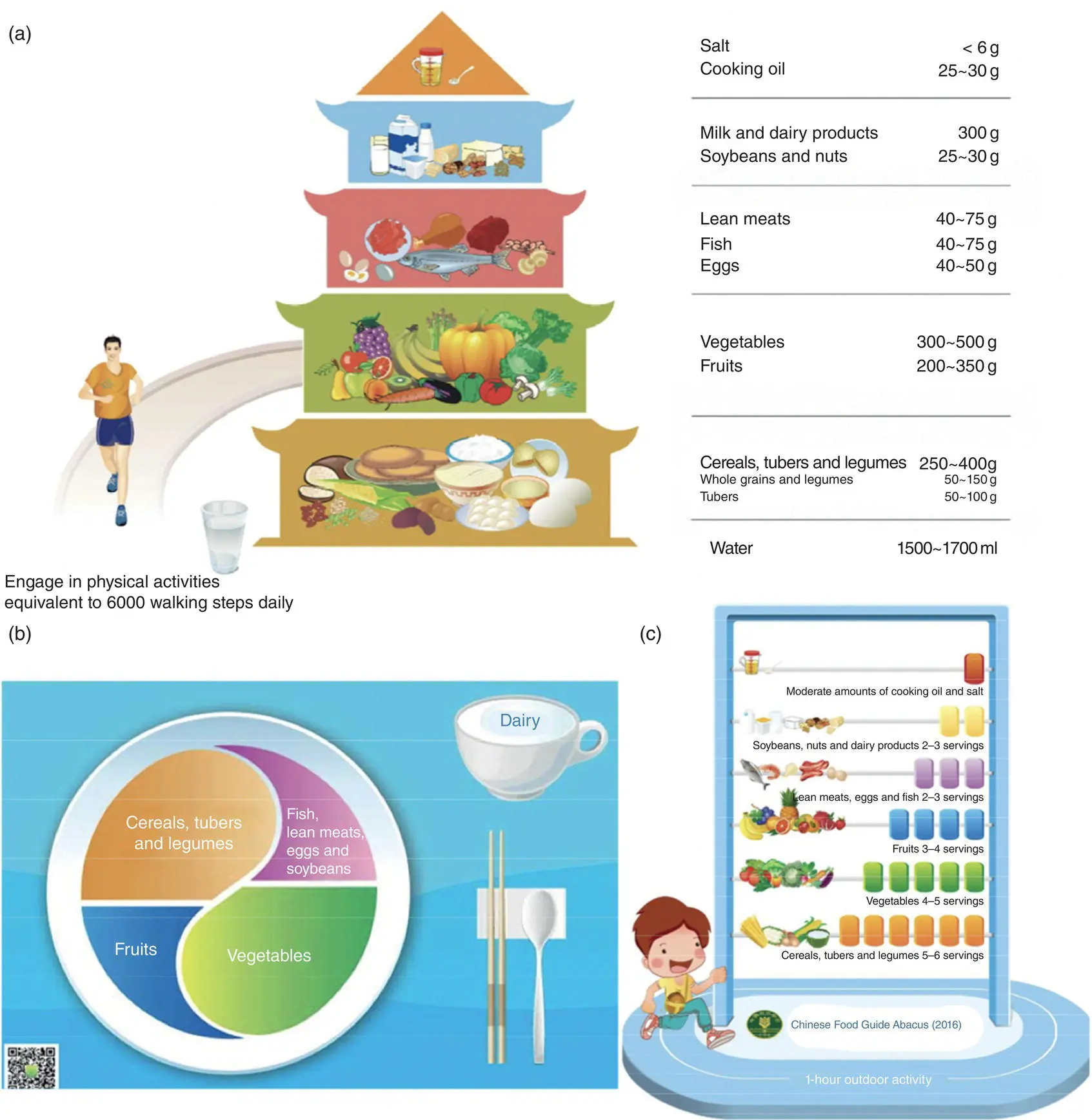
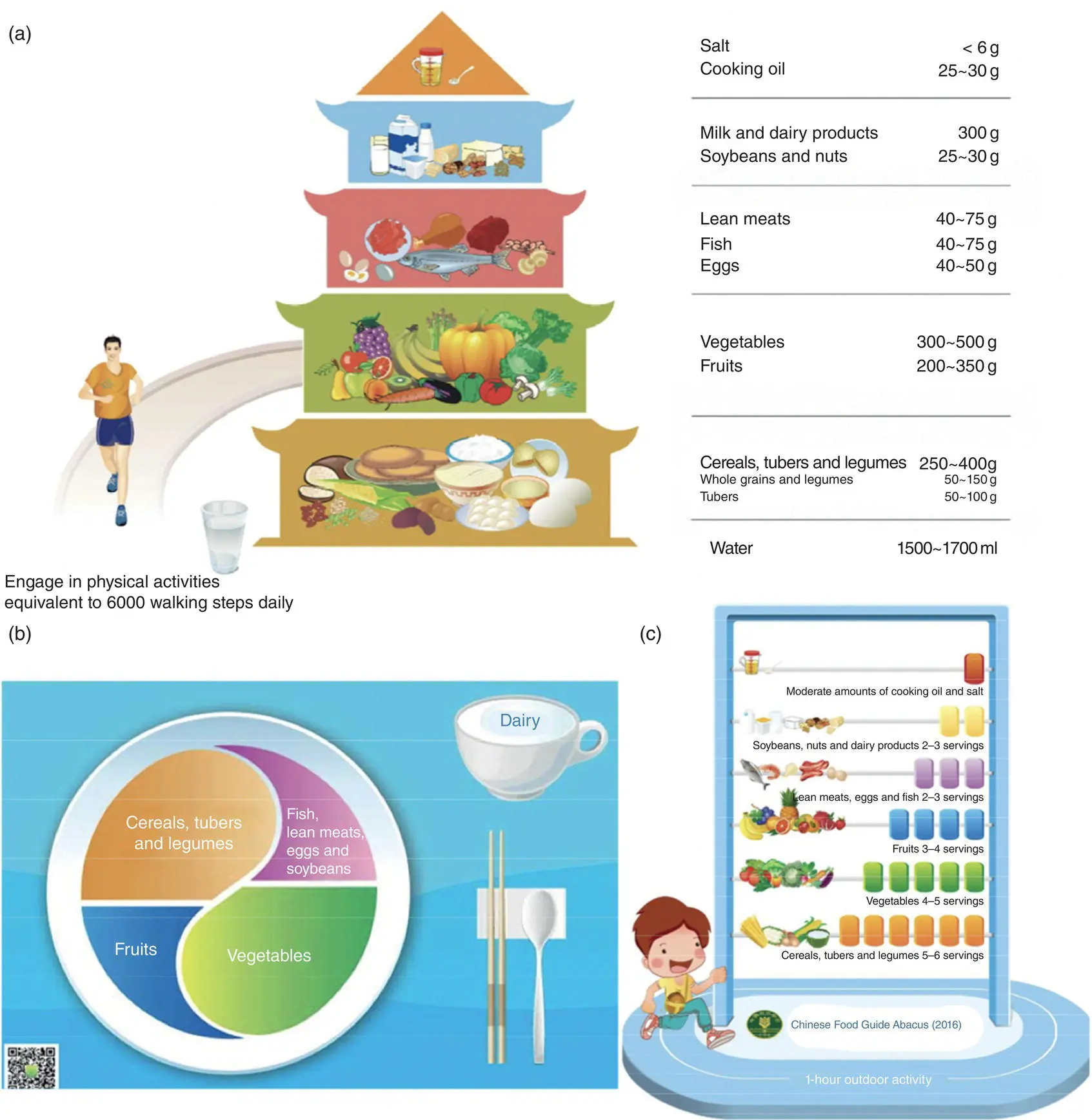
FIGURE 6.5 Illustrations for the Chinese dietary guidelines launched in 2016: (a) Chinese Food Guide (CFG) G‐Pagoda is the main graphical illustration; (b) CFG‐Plate; and (c) CFG‐Abacus function as supplementary illustrations for CFG‐Pagoda.
Source:Reprinted from Yang et al. (2018b).
The traditional Asian diet is followed in most Asian countries, and although it varies in many aspects between countries, it holds many similarities regarding the consumption of traditional Asian foods.
The Asian diet is primarily characterized by high consumption of rice, foods of plant origin (e.g., soy products), fish and seafood, as well as fruits and vegetables.
The Japanese and the Chinese dietary guidelines represent two well‐documented examples of healthy Asian diets.
The incidence of several chronic diseases, such as CVD and cancer, has been shown to be lower in most Asian societies compared to most Western countries.
The recent shift from the traditional Asian diet to a more Western‐like diet is characterized by an increase in meat consumption and a decrease in rice consumption.
Self‐Assessment Questions
1 What are the main characteristics of the Asian diet?
2 State two well‐documented examples of healthy Asian diets.
3 What kinds of foods are included at the base of the “Chinese Food Guide Pagoda”?
1 Abaidia, A.E., Daab, W., and Bouzid, M.A. (2020). Effects of Ramadan fasting on physical performance: a systematic review with meta‐analysis. Sports Med. 50 (5): 1009–1026.
2 Akhlaghi, M. (2020). Dietary Approaches to Stop Hypertension (DASH): potential mechanisms of action against risk factors of the metabolic syndrome. Nutr. Res. Rev. 33 (1): 1–18.
3 Ali Mohsenpour, M., Fallah‐Moshkani, R., Ghiasvand, R. et al. (2019). Adherence to Dietary Approaches to Stop Hypertension (DASH)‐style diet and the risk of cancer: a systematic review and meta‐analysis of cohort studies. J. Am. Coll. Nutr. 38 (6): 513–525.
4 Baroni, L., Goggi, S., and Battino, M. (2018). VegPlate: a Mediterranean‐based food guide for Italian adult, pregnant, and lactating vegetarians. J. Acad. Nutr. Diet. 118 (12): 2235–2243.
5 Chen, J., Campbell, T.C., Li, J., and Peto, R. (1990). Diet, Lifestyle and Mortality in China. A Study of the Characteristics of 65 Chinese Counties. A joint publication of: Oxford University Press, Cornell University Press, and the People’s Medical Publishing House.
6 Coronary heart disease in seven countries. XVII. The diet. (1970). Circulation 41 (4 Suppl): I162–I183.
7 Derbyshire, E.J. (2016). Flexitarian diets and health: a review of the evidence‐based literature. Front. Nutr. 3: 55.
8 Eliasi, J.R. and Dwyer, J.T. (2002). Kosher and halal: religious observances affecting dietary intakes. J. Am. Diet. Assoc. 102 (7): 911–913.
9 Eveleigh, E.R., Coneyworth, L.J., Avery, A., and Welham, S.J.M. (2020). Vegans, vegetarians, and omnivores: how does dietary choice influence iodine intake? A systematic review. Nutrients 12 (6): 1606.
10 FAO. (2010). Food‐based dietary guidelines for Japanese. www.fao.org/nutrition/education/food‐dietary‐guidelines/regions/countries/Japan/en.
11 Fernando, H.A., Zibellini, J., Harris, R.A. et al. (2019). Effect of Ramadan fasting on weight and body composition in healthy non‐athlete adults: a systematic review and meta‐analysis. Nutrients 11 (2): 478.
12 Gonzalez‐Garcia, S., Esteve‐Llorens, X., Moreira, M.T., and Feijoo, G. (2018). Carbon footprint and nutritional quality of different human dietary choices. Sci. Total Environ. 644: 77–94.
13 Haghighatdoost, F., Bellissimo, N., Totosy, de Zepetnek, J.O., and Rouhani, M.H. (2017). Association of vegetarian diet with inflammatory biomarkers: a systematic review and meta‐analysis of observational studies. Public Health Nutr. 20 (15): 2713–2721.
14 Haider, L.M., Schwingshackl, L., Hoffmann, G., and Ekmekcioglu, C. (2018). The effect of vegetarian diets on iron status in adults: a systematic review and meta‐analysis. Crit. Rev. Food Sci. Nutr. 58 (8): 1359–1374.
15 Iguacel, I., Huybrechts, I., Moreno, L.A., and Michels, N. (2021). Vegetarianism and veganism compared with mental health and cognitive outcomes: a systematic review and meta‐analysis. Nutr. Rev. 79 (4): 361–381.
16 Kanerva, N., Kaartinen, N.E., Schwab, U., Lahti‐Koski, M., and Männistö, S. (2014). The Baltic Sea Diet Score: a tool for assessing healthy eating in Nordic countries. Public Health Nutr. 17 (8): 1697–1705. doi: 10.1017/S1368980013002395.
17 Koufakis, T., Karras, S.N., Zebekakis, P., and Kotsa, K. (2018). Orthodox religious fasting as a medical nutrition therapy for dyslipidemia: where do we stand and how far can we go? Eur. J. Clin. Nutr. 72 (4): 474–479.
18 Landberg, R. and Hanhineva, K. (2019). Biomarkers of a healthy Nordic diet: from dietary exposure biomarkers to microbiota signatures in the metabolome. Nutrients 12 (1): 27.
19 Lankinen, M., Uusitupa, M., and Schwab, U. (2019). Nordic diet and inflammation – a review of observational and intervention studies. Nutrients 11 (6): 1369.
20 Lee, I.M., Shiroma, E.J., Lobelo, F. et al. (2012). Effect of physical inactivity on major non‐communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 380 (9838): 219–229.
21 Li, Y., Hruby, A., Bernstein, A.M. et al. (2015). Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J. Am. Coll. Cardiol. 66 (14): 1538–1548.
22 Mach, F., Baigent, C., Catapano, A.L. et al. (2020). 2019 ESC/EAS guidelines for the management of dyslipidemias: lipid modification to reduce cardiovascular risk. Eur. Heart J. 41 (1): 111–188.
23 Makarem, N., Bandera, E.V., Lin, Y. et al. (2018). Consumption of sugars, sugary foods, and sugary beverages in relation to adiposity‐related cancer risk in the Framingham offspring cohort (1991–2013). Cancer Prev. Res. (Phila). 11 (6): 347–358.
24 Martin, C.A., Gowda, U., Smith, B.J., and Renzaho, A.M.N. (2018). Systematic review of the effect of lifestyle interventions on the components of the metabolic syndrome in South Asian migrants. J. Immigr. Minor. Health. 20 (1): 231–244.
25 Melina, V., Craig, W., and Levin, S. (2016). Position of the Academy of Nutrition and Dietetics: vegetarian diets. J. Acad. Nutr. Diet. 116 (12): 1970–1980.
26 Meltzer, H.M., Brantsaeter, A.L., Trolle, E. et al. (2019). Environmental sustainability perspectives of the Nordic diet. Nutrients 11 (9): 2248.
27 Mihrshahi, S., Ding, D., Gale, J. et al. (2017). Vegetarian diet and all‐cause mortality: evidence from a large population‐based Australian cohort – the 45 and up study. Prev. Med. 97: 1–7.
28 NCEP‐ATPIII. (2001). Executive summary of the third report (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285 (19): 2486–2497.
29 Nishimura, T., Murakami, K., Livingstone, M.B. et al. (2015). Adherence to the food‐based Japanese dietary guidelines in relation to metabolic risk factors in young Japanese women. Br. J. Nutr. 114 (4): 645–653.
Читать дальше