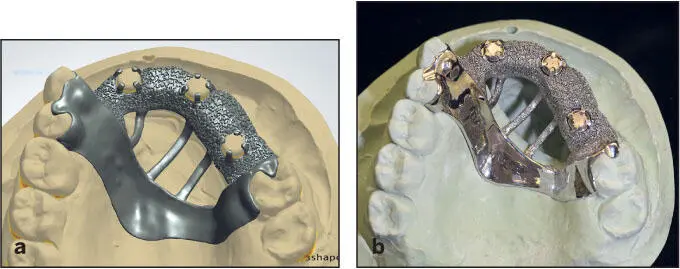
The manufacturing units work in conjunction with the CAD software. The generated STL files form the software used to control the manufacturing units. Currently, the most standardized method for producing implant-related restorations is via milling through a computer numeric controlled (CNC) machine. More recently, additive manufacturing has become an option; however, it requires further refinements to produce implant prostheses of acceptable quality (see earlier section entitled “New manufacturing techniques”). 106However, additive manufacturing is extremely beneficial for the production of casts, removable partial denture frameworks ( Fig 5-21), and surgical guides from digital data.
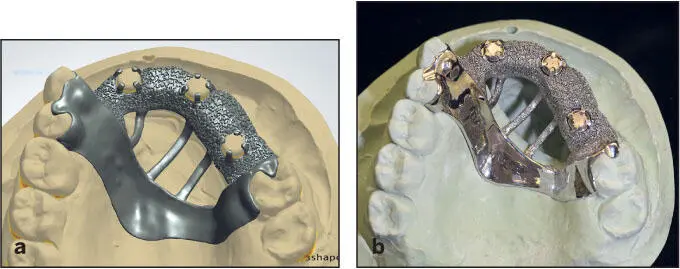
Fig 5-21 (a) Designed framework. (b) Printed pattern confirmed to fit the master cast.
Milling-facilitated production of components of more contemporary materials
Milled titanium and base metal alloys (such as cobalt- chromium), abutments, and frameworks can be reliably produced with a fit level closer to prefabricated implant components. 1As a result, several implant companies and milling centers provide customized component options. While titanium has been a material of interest due to its biocompatibility and similarity to the implant material, it cannot be predictably veneered with ceramic. As a result, base metal alloys were proposed as an alternative to overcome the ceramic bonding limitations. In addition, after the introduction and advancement of toughened zirconia, implant components can be produced from zirconia, which is currently the most durable esthetic and metal-free option. To date, milling is the only method to predictably produce zirconia restorations (see chapter 8, section entitled “Monolithic Zirconia Prostheses” and chapter 10, section entitled “Procedures for monolithic zirconia fixed prostheses”).
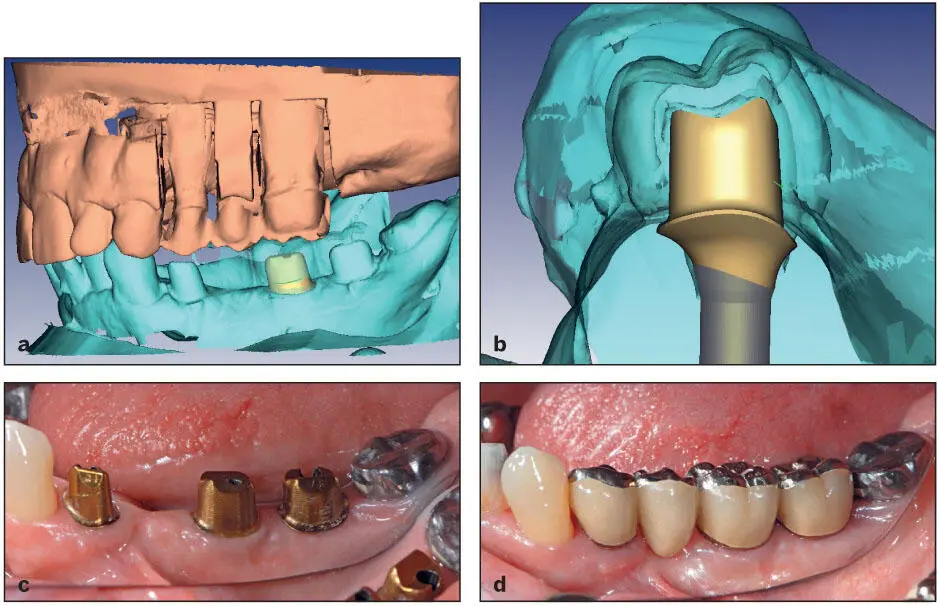
Whenever possible, it is recommended to customize implant components. The use of CAD software allows for abutments to be reliably customized specifically for the prosthetic design and to be manufactured with CAM technology. As opposed to prefabricated components, customizing implant components for individual patients has multiple advantages such as an ideal finish line location, anatomical contouring, and correct material bulk for durability 107( Fig 5-22). Correct finish line location is necessary for cement-retained restorations, because in deep margins it has been found to be difficult or even impossible to eliminate the cement, which will eventually cause biologic complications. Anatomical contouring is advocated to ensure even veneering ceramic layer thickness and acceptable morphology to retain the cemented restoration. In addition, customizing an abutment ensures achieving an ideal gingival contour, emergence profile, resistance form, and retention form.
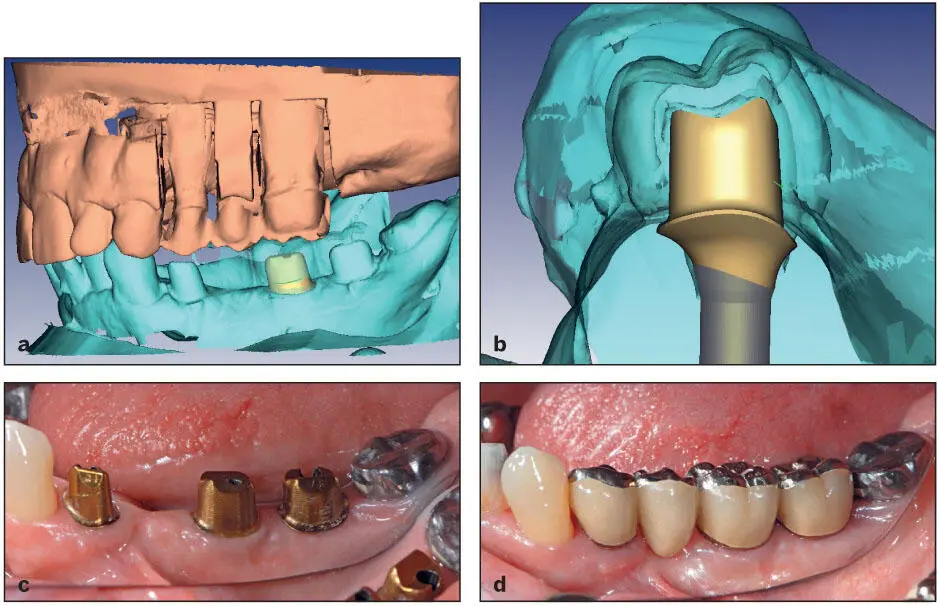
Fig 5-22 (a and b) Image of the planned custom abutment design prior to manufacturing. Designs can be modified or approved. (c) Milled custom abutments tried in to verify fit, contours, and margin placements. (d) Definitive cement-retained metal-ceramic restorations.
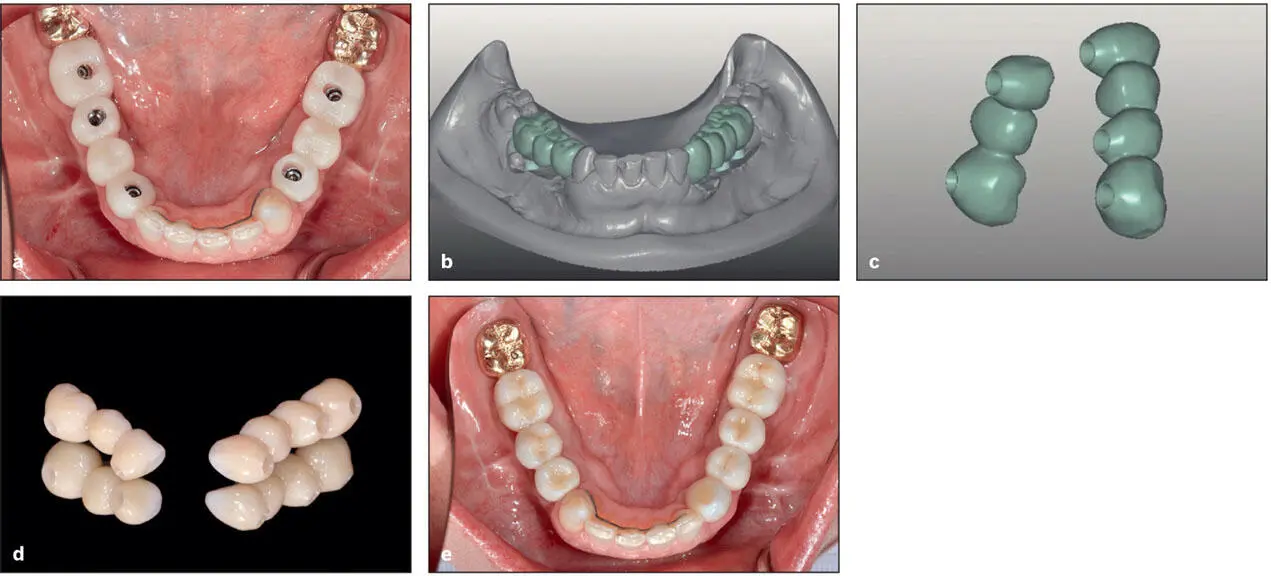
A clear advantage of this feature was found for zirconia- based restorations where the veneering ceramic can be kept to a minimum or eliminated, thereby reducing the likelihood of ceramic chipping ( Fig 5-23). More recently, with the advancement of CAD/CAM technologies, monolithic zirconia has been advocated, where the restoration is made from zirconia with minimal or no ceramic veneering. In addition, the software ensures that a minimal acceptable thickness of the component is provided for milling. Digital fabrication is linked to the design software, ensuring accurate reproduction of the planned components. Therefore, digital customization is more reliable, efficient, and convenient than traditional techniques.
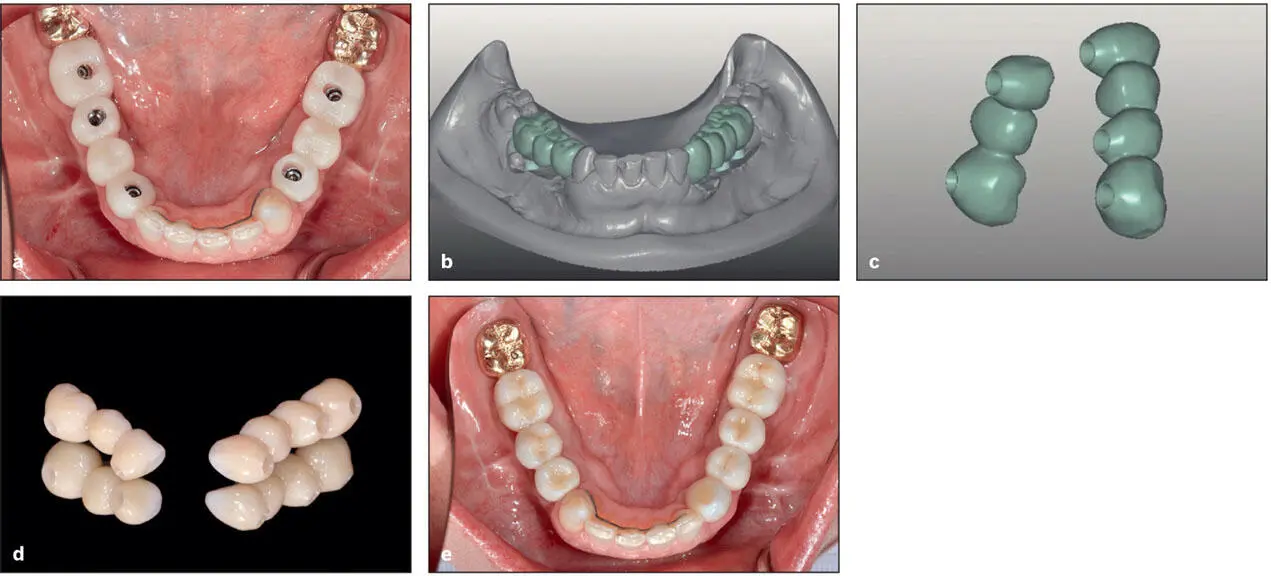
Fig 5-23 (a) Trial (prototype) prostheses. The prostheses were inserted and adjusted as needed to refine the occlusion and hygiene access over a period of several weeks. The prostheses were then removed, placed upon the master cast, and (b) scanned. The tissue surfaces were slightly refined (c) , and the definitive prostheses were fabricated from monolithic zirconia (d and e) .
Because CAD/CAM reduces the level of human intervention and the overall fabrication steps, it has been speculated that CAD/CAM is capable of producing implant components with greater accuracy than conventional techniques. In addition, as the shape of the implant connection and abutments are based on known parameters, reverse engineering modeling and milling the interfaces to high precision is possible. 2, 108This was confirmed by laboratory studies on abutments and frameworks, where the studies consistently found that the fit of CAD/CAM-produced components is superior to conventionally fabricated components. 18This was generally found for titanium and base metal alloys; however, the fit of zirconia components appears promising, although it was more prone to errors in the form of rotational freedom or vertical misfit as well as fractures. 109– 111To overcome this problem, prefabricated titanium metal inserts have been considered.
Evolving workflow
Due to the integration of the digital manufacturing with all the features of digital technologies mentioned in this chapter, component and prosthesis fabrication is generally simpler and more reliable than conventional fabrication. For example, digitally produced restorations can easily mimic the digitally planned restoration. Because the CNC machine is controlled by a series of commands from the CAM software, the contour of the restoration can be precisely controlled to generate the planned restoration contour. This will simplify producing esthetic and symmetric restorations. Through the office digital workflow, the clinician is able to produce the implant restoration within the clinic in one restorative visit. This involves scanning the metal insert or prefabricated abutment, designing the prosthesis digitally, and milling the prosthesis via a chairside milling unit. The produced restoration can then be attached to the insert or the abutment. On the other hand, with the aid of a digital impression, an STL image of the implant and the arch can be transferred to the dental technician or milling center for fabrication of the prosthesis. The manufacturing center can produce a dental cast by additive technology on which they can fit the prosthesis for further customization of the contour, shade, proximal contacts, and occlusion. More advanced digital protocols allow for the production of a definitive prosthesis prior to implant placement. Given that implants can be precisely inserted by fully guided surgery, the implants can be immediately restored with a digitally processed prosthesis without significant chairside modifications. However, this protocol requires more validation, because bone and soft tissue healing may influence the appearance of the definitive prosthesis.
Summary
Digital technologies are tools that can enhance clinical outcomes when used properly. However, not all implant surgeries require digital treatment planning, and before digital technology existed, traditional prosthodontic workup methods enabled the prosthodontist or restorative dentist to communicate effectively with the implant surgeon and laboratory technician. Certainly, with digital planning and the associated technologies, the collaboration among the implant team is enhanced. However, more time is spent with planning, and there are increased costs to both the patient and the implant team.
Читать дальше