Ridley's The Vulva
Здесь есть возможность читать онлайн «Ridley's The Vulva» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Ridley's The Vulva
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:3 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 60
- 1
- 2
- 3
- 4
- 5
Ridley's The Vulva: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Ridley's The Vulva»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Ridley’s The Vulva
Ridley’s The Vulva
Ridley's The Vulva — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Ridley's The Vulva», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
The urogenital diaphragm
The urogenital diaphragm (also known as perineal membrane or triangular ligament) is a tough fibrous membrane attached to the pubic rami ( Figure 2.12). It has three midline breaks, one at the apex of the triangle just below the pubic symphysis where the clitoral vessels and nerves pass from the deep to the superficial perineal pouch, and two more posteriorly for the entrances of the urethra and vagina.
Deep perineal pouch
The deep perineal pouch is limited above by the pelvic floor and pubovesical ligaments and below by the urogenital diaphragm. It is continuous with the ischiorectal fossae posteriorly. The urethra and vagina pass through the deep perineal pouch in the midline. Vessels and nerves run alongside the urethra and vagina, and their clitoral branches ascend through the apical opening in the urogenital diaphragm. The deep pouch also contains voluntary muscle fibres, some of which surround the urethra and vagina while others run transversely into the perineal body behind the vagina.
Superficial perineal pouch
This lies below the urogenital triangle and contains the structural elements of the female external genitalia, which, with their skin covering, exhibit the external appearance characteristic of the vulva. The clitoral bulbs lie in the superficial perineal pouch adjacent to the lateral wall of the vagina and are attached to the inferior surface of the urogenital diaphragm by the overlying bulbospongiosus muscle. Just behind the clitoral bulbs, also lying on the urogenital diaphragm, are Bartholin’s glands. The superficial transverse perineal muscles lie transversely across the base of the urogenital triangle at the posterior margin of the superficial perineal pouch ( Figure 2.13).
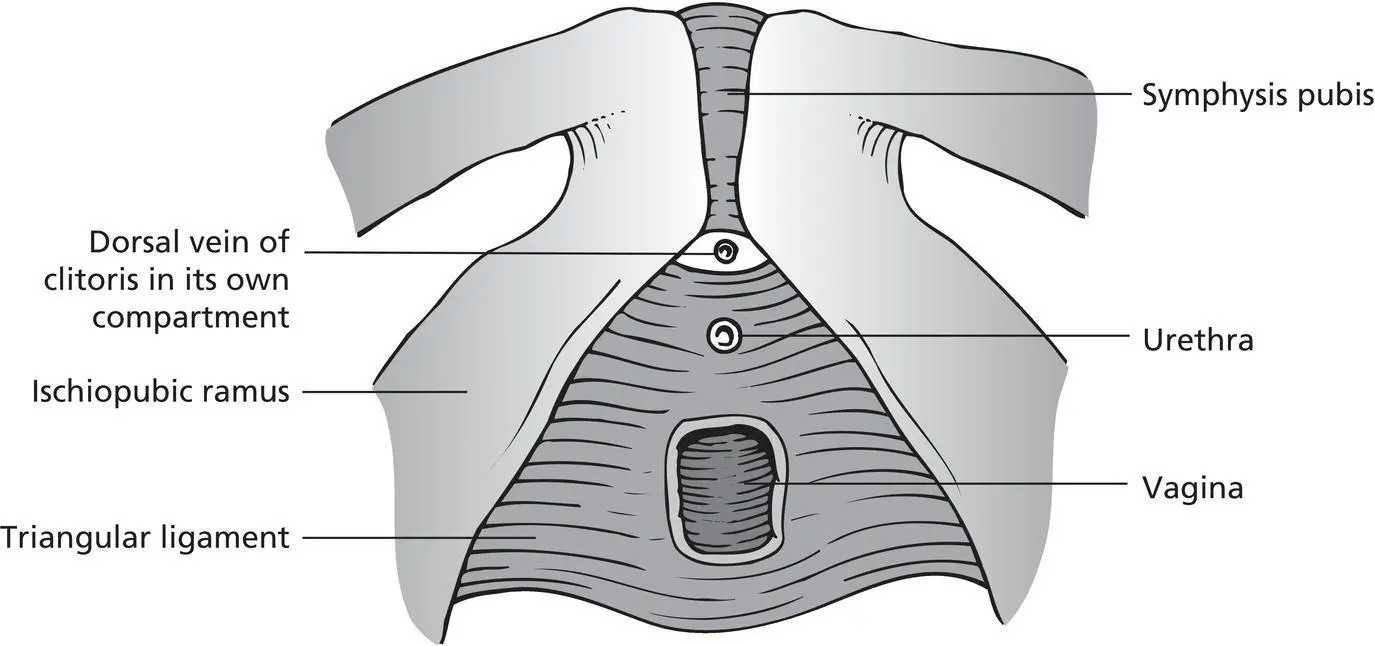
Figure 2.12 The urogenital diaphragm.
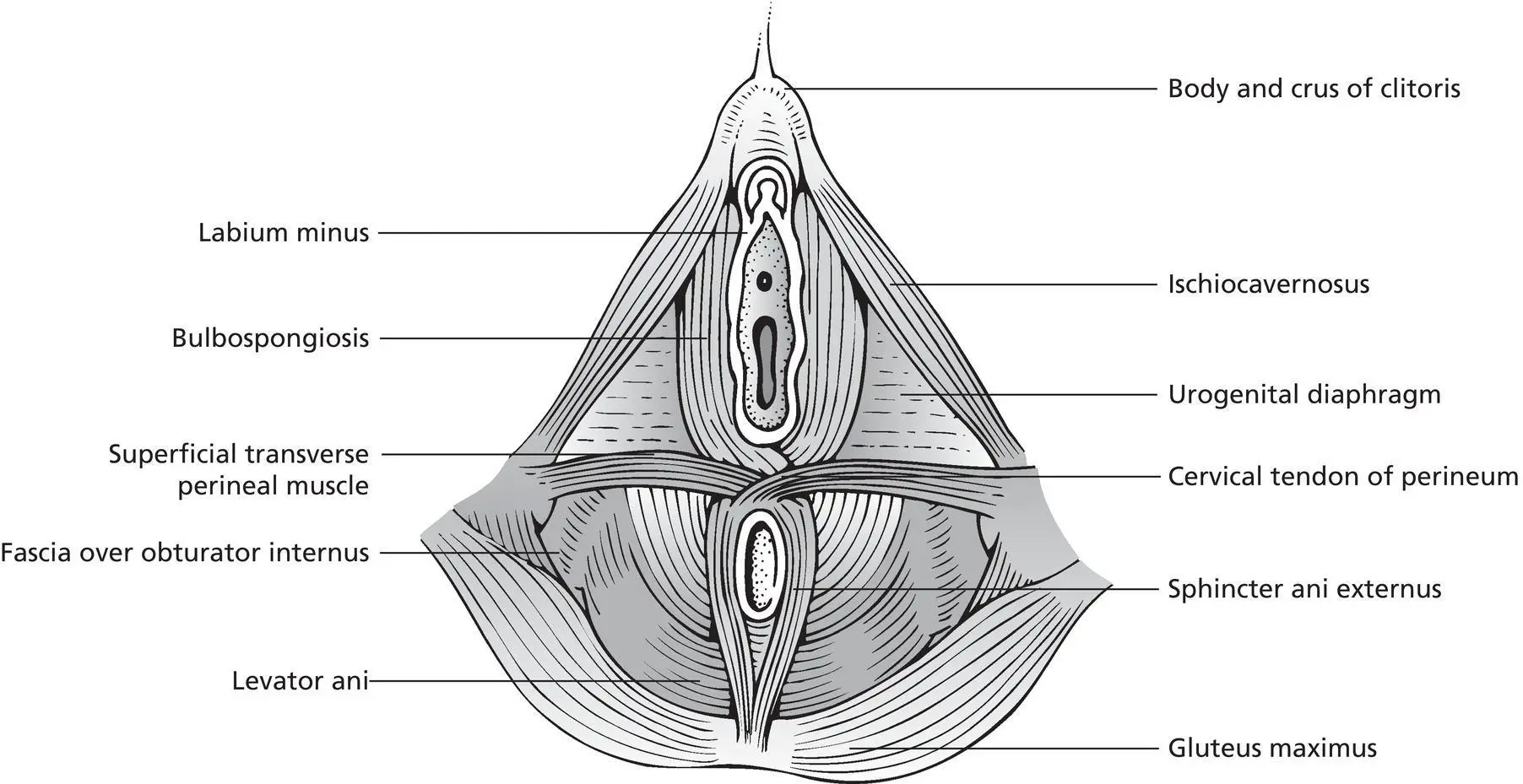
Figure 2.13 The superficial structures of the perineum.
Anal triangle
The anal triangle is the triangular area bounded by the ischial tuberosities and the coccyx. The anal canal lies within this area. The ischiorectal fossae lie laterally to the anal canal ( Figure 2.14). These are pyramid‐shaped areas bounded by ischium and obturator internus laterally, levator ani medially, and the perianal skin inferiorly. The fossae contain fat and connective tissue, and the nerves to the anus, perineum, and external genitalia traverse this space. The anal canal is the terminal 2.5–3.5 cm of the large intestine and passes through the levator ani. It has an internal involuntary sphincter derived from the smooth muscle of the rectum around its upper two‐thirds and an external voluntary sphincter muscle around the lower two‐thirds. This sphincter muscle blends with the puborectalis muscle.
The pelvic floor
The pelvic floor (pelvic diaphragm) is composed of sheets of muscles arranged around the midline urethra, vagina, and anal canal. The main functions of the pelvic floor are to support the pelvic organs and to help to maintain continence when intra‐abdominal pressure is raised during episodes of coughing, sneezing, and muscular effort. This pelvic floor is made up of the ischiococcygeus, iliococcygeus, and pubococcygeus muscles, which have a bilateral linear origin from the white line overlying the obturator fascia on the side wall of the pelvis. This extends from the ischial spine posteriorly to the pubic bone anteriorly. The muscles reach their midline insertion into the sacrum, coccyx, anococcygeal raphe, and perineal body, and therefore form a gutter‐shaped pelvic floor, which slopes downwards and forwards ( Figure 2.15).
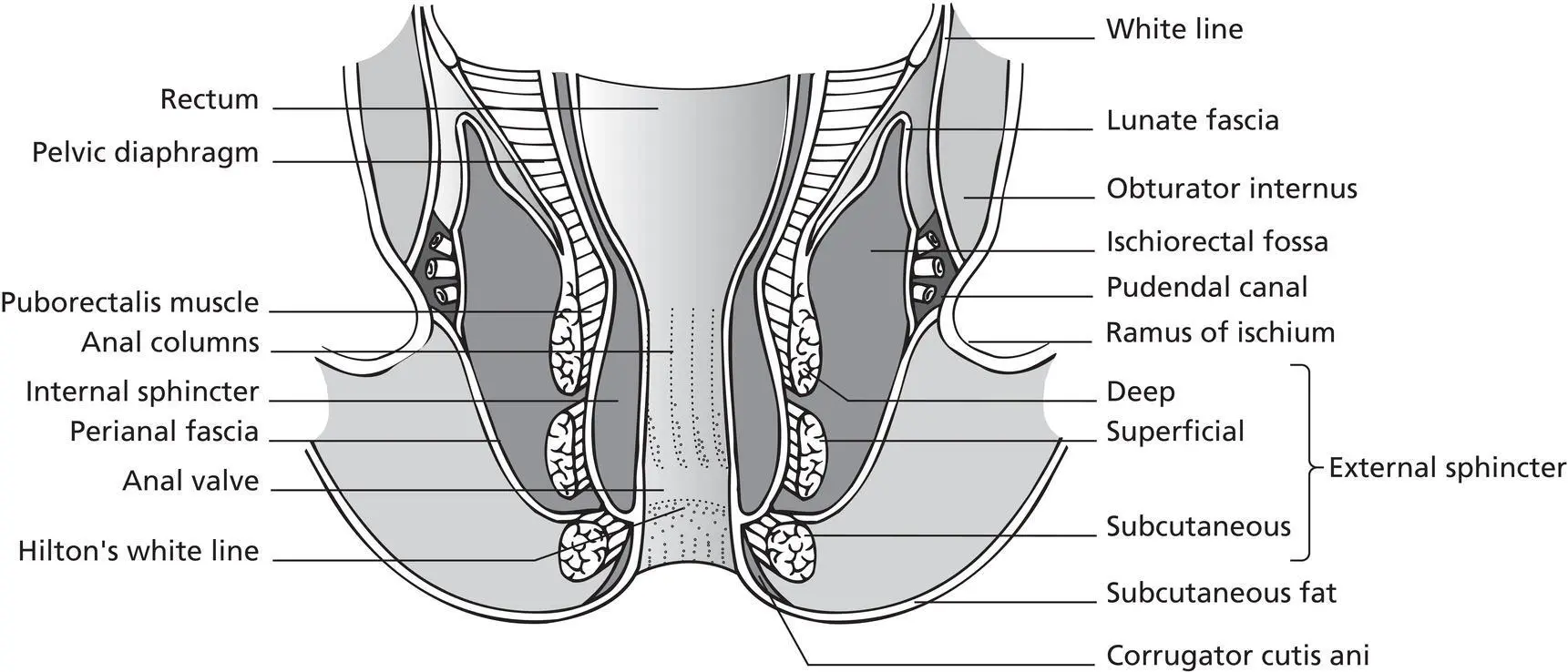
Figure 2.14 A coronal section through the anal canal and ischiorectal fossa.
Ischiococcygeus muscle
This arises from the ischial spine and is inserted into the fifth sacral vertebra and the coccyx.
Iliococcygeus muscle
The iliococcygeus arises from the ischial spine and posterior half of the fibrous linear origin and, overlying the pelvic surface of the ischiococcygeus, is inserted into the coccyx and anococcygeal raphe. This raphe is the interdigitation of muscle fibres from the right and left sides, and extends from the tip of the coccyx to the anorectal junction.
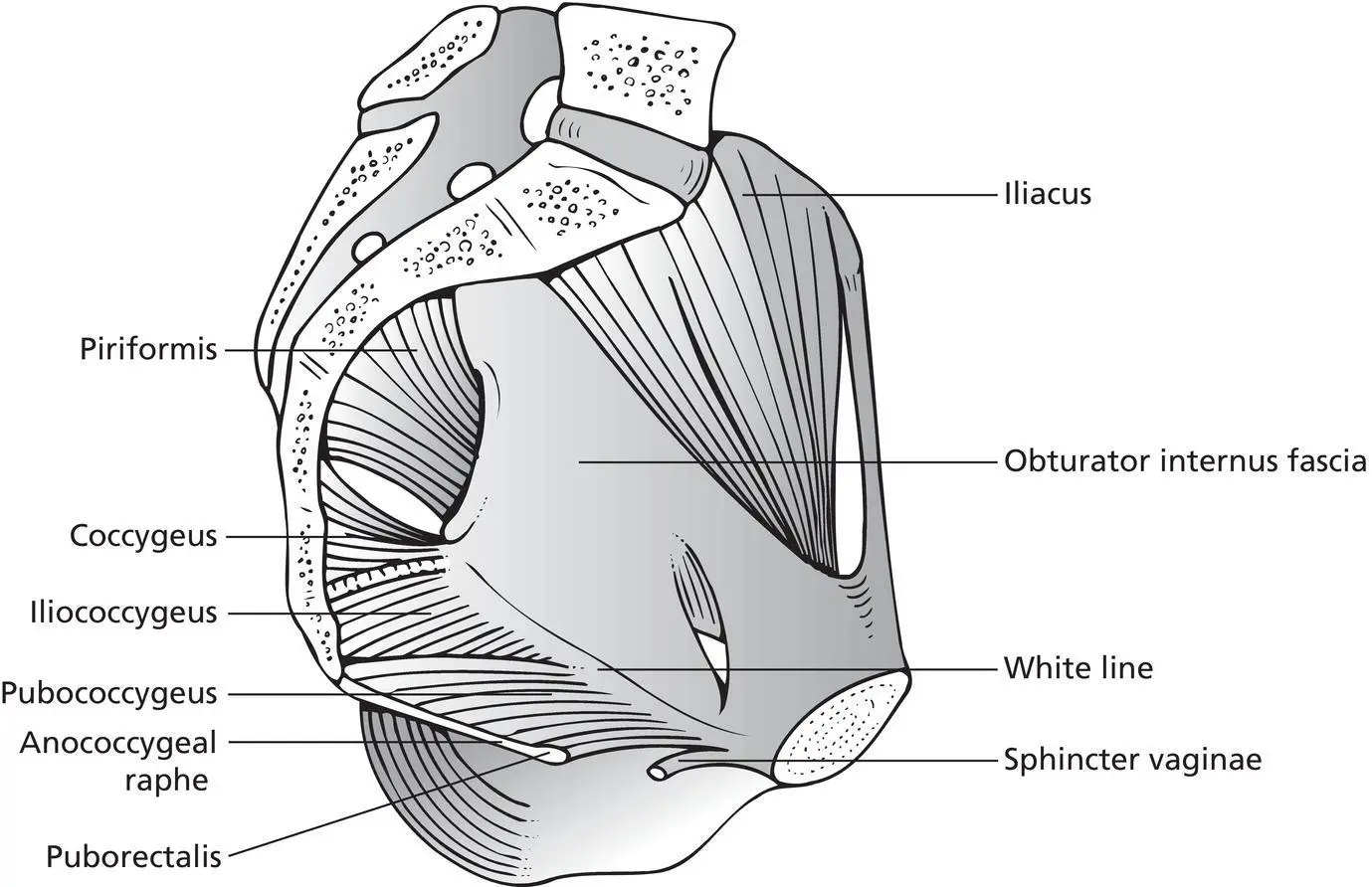
Figure 2.15 The muscles of the pelvic walls and pelvic floor.
Pubococcygeus muscle
The pubococcygeus arises from the anterior half of the linear origin and from the posterior surface of the body of the pubis. The fibres arising from the fibrous linear origin sweep backwards on the pelvic surface of the iliococcygeus to be inserted into the anococcygeal raphe. Those fibres arising from the pubic bone form a muscle sling around the anorectal junction, producing a forward angulation of this junction. This part of the pubococcygeus is referred to as the puborectalis, and it lies beneath the anococcygeal raphe and intermingles with the deep part of the external anal sphincter. The most medial fibres arising from the pubis form a muscle sling around the vagina (sphincter vaginae) which unite with the perineal body behind the vagina. The midline gap between the medial edges of the sphincter vaginae is occupied by the pubovesical ligaments and the deep dorsal vein of the clitoris.
The inguinofemoral region
The femoral triangle is a gutter‐shaped depression below the groin. The base is formed by the inguinal ligament, and its apex is situated medially and inferiorly. The inguinal ligament is the lower free margin of the external oblique muscle of the anterior abdominal wall and extends from the anterior superior spine of the iliac bone laterally to the tubercle on the body of the pubic bone medially. Midway between these two points, the external iliac artery becomes the femoral artery and enters the femoral triangle deep to the inguinal ligament and the deep fascia of the thigh (fascia lata). A short downward extension of the abdominal fascia (femoral sheath) is created when the external iliac vessels enter the triangle, and this sheath encloses the femoral artery laterally, the femoral vein centrally, and the femoral canal medially. The long saphenous vein passes through the saphenous opening in the fascia lata to enter the femoral vein at the medial end of the inguinal ligament.
Table 2.2 Blood supply, innervation, and lymphatic drainage of the vulva.
| Arterial supply | Venous drainage | Innervation | Lymphatic drainage | |
|---|---|---|---|---|
| Mons pubis | Superficial external pudendal artery which is a branch of the femoral artery. | Pudendal veins to the long saphenous vein | Branches of the perineal nerve | To superficial inguinal nodes and then to deep femoral nodes and pelvic nodes |
| Labia majora | Labial branches of the internal pudendal artery | Tributaries to the superficial external pudendal vein which then drain to the great saphenous vein | Labial branches of the perineal nerve | Superficial inguinal nodes and the inferior aspect to the rectal lymphatic plexus |
| Labia minora | Labial branches of the internal pudendal artery | Tributaries to the superficial external pudendal vein which then drain to the great saphenous vein | Labial branches of the perineal nerve | Superficial inguinal nodes |
| Clitoris | Superficial and deep terminal branches of the internal pudendal artery | Deep dorsal vein to vesicle plexus, deep external pudendal veins to femoral vein and internal pudendal veins to internal iliac vein | Dorsal nerve of the clitoris, a branch of the pudendal nerve | To deep inguinal and internal iliac nodes |
| Vestibule | Branches of the internal pudendal artery | Tributaries to the external pudendal vein | Perineal branch of the pudendal nerve | To superficial inguinal nodes |
| External urethral meatus and urethra | Vesical and vaginal arteries which are branches of the anterior internal iliac artery | Via plexus around the urethra to vesicle plexus around the bladder neck and into the pudendal veins | Pudendal nerve | Urethral lymphatics drain into the internal and external iliac nodes |
| Vagina | The vaginal artery may arise from the internal iliac artery or one of its branches, most commonly the internal pudendal artery. The uterine artery supplies a descending branch to the upper vagina, and there is frequently a vaginal branch from the middle rectal artery. The lower vagina is supplied by branches of the internal pudendal artery. These vessels anastomose with each other in or on the vaginal walls. Vessels from the right and left sides anastomose to form unpaired, midline, anterior, and posterior azygos arteries | The veins of the vagina drain to the uterovaginal plexus, which itself communicates with the uterine, vesical, and rectal venous plexuses, all of which drain mainly to the internal iliac veins | Nerve fibres accompany the vessels as they penetrate the walls of the body of the uterus, cervix, and vagina. There is general agreement that almost all of the motor fibres to uterine muscle are sympathetic, while afferent innervation of the body is sympathetic and that of the cervix is parasympathetic | The upper two‐thirds is with the cervix to the internal and external iliac nodes. The lower vessel third drains with the rest of the perineum to the superficial inguinal nodes |
| Perineum | Perineal artery | Internal pudendal vein | Pudendal nerve | Superficial inguinal nodes |
| Pelvic floor | Lumbosacral plexus (S2–S4) |
Blood supply of the vulva
Интервал:
Закладка:
Похожие книги на «Ridley's The Vulva»
Представляем Вашему вниманию похожие книги на «Ridley's The Vulva» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Ridley's The Vulva» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.