Ridley's The Vulva
Здесь есть возможность читать онлайн «Ridley's The Vulva» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Ridley's The Vulva
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:3 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 60
- 1
- 2
- 3
- 4
- 5
Ridley's The Vulva: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Ridley's The Vulva»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Ridley’s The Vulva
Ridley’s The Vulva
Ridley's The Vulva — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Ridley's The Vulva», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
The parasympathetic system does not participate in mediation of common sensations such as temperature and pain. The sensory components of the parasympathetic innervation of the perineum mediate the sensation of distension from the anal canal and vagina, while its motor component is responsible for the vascular engorgement of vaginal erectile tissue.
The cutaneous innervation of the perineum conveys all modalities of common sensation such as touch, pain, itch, and temperature, as well as complex sensations such as wetness. In addition, these cutaneous nerves carry postganglionic sympathetic nerves that provide motor innervation to sweat glands, pilomotor units, and blood vessels. These sacral spinal nerves also supply motor innervation to the muscles of the perineum. The anterior part of the perineum is supplied by two nerves that emerge from the superficial inguinal ring just above the body of the pubic bone. These are the ilioinguinal nerve (L1) and the genital branch (L2) of the genitofemoral nerve (L1 and L2). The lateral aspect of the perineum, more posteriorly, is supplied by the perineal branch (S1) of the posterior cutaneous nerve of the thigh (S1–S3). The remainder of the cutaneous innervation of the perineum is supplied by the pudendal nerve (S2–S4) and the perineal branch of the fourth sacral nerve , which also supplies the skin of the anal margin.
Pudendal nerve
The pudendal nerve enters the ischiorectal fossa, close to the tip of the ischial spine on the medial side of the pudendal artery. Running anteriorly on the lateral wall of the ischiorectal fossa, it gives rise to the inferior haemorrhoidal nerve, which arches over the roof of the fossa to reach the midline, where it supplies the terminal part of the anal canal and the perianal skin. The pudendal nerve then divides into the perineal branch , which supplies the rest of the perineal skin, and the dorsal nerve of the clitoris , which supplies the anterior labia minora and the glans of the clitoris.
The inferior haemorrhoidal branch of the pudendal nerve supplies the deep and subcutaneous parts of the external anal sphincter. The perineal branch supplies the muscles of the urogenital triangle as well as the anterior part of the levator ani muscle and the urethral sphincter. The remainder of the levator ani muscle and the superficial part of the external anal sphincter are supplied by the perineal branch of the fourth sacral nerve . Damage to the pudendal nerves may cause loss of muscle tone in the pelvic floor and can be associated with problems of incontinence.
Microscopic anatomy
The cutaneous nerves contain axons with the cell bodies lying in the dorsal root ganglia. The main nerve trunks enter the subcutaneous fat and divide into smaller bundles that form a horizontal network with fibres ascending alongside blood vessels to form a plexus of interlacing nerves in the superficial dermis. A few reach the basement membrane but do not extend far into the epidermis. The hair follicle has a complex nerve network, being an important cutaneous receptor.
Normal microscopic anatomy and histological features
Epithelia of the vulva
The vulva is covered in epithelia that gradually change from normal keratinised skin on the outer aspects to a non‐keratinised mucosa in the vestibule and vagina.
Keratinised, stratified squamous epithelium is made up of four layers histologically:
1 A basal layer, the lower border of which rests on the basal lamina
2 A spinous or prickle‐cell layer, which forms the bulk of the epidermis
3 A granular layer
4 A horny layer or stratum corneum.
The epithelial thickness reduces and the keratin layer increases going from medial to lateral on the vulva [29]. This has been confirmed in a recent study of 118 biopsies of normal vulval skin [ 30]. In addition, it was found that the stratum corneum was always of a basket weave pattern on the mons pubis, and this pattern was more common in hair‐bearing skin but did not occur on the perineum, where compact or intermediate patterns were seen.
Differentiation is the process that occurs as the keratinocytes move upwards through the spinous layers to form the tough, protective, flexible outer surface of the skin. The keratinocytes flatten and lose their nuclei as they progress upwards, ending up as flattened structureless squamous cells at the surface. Parakeratosis (the retaining of nuclei) can be seen at the mucocutaneous junction in some patients and is considered a normal finding [ 30].
Mons pubis
The mons pubis is covered with hair‐bearing skin. The pilosebaceous unit comprises the hair follicle, the hair, the sebaceous gland, and the arrectores pilorum muscle, and some are associated with an apocrine gland. Eccrine glands are also present.
Labia majora
The outer surface of the labia majora and the perianal area are covered with hair‐bearing skin ( Figure 2.16), but the inner aspects are hairless. The labia majora have a full complement of adnexal structures, but there is no hair in the pilosebaceous unit on the inner aspect. Small numbers of lymphocytes are often seen, and anogenital mammary‐like glands (AGMLG) are found most commonly in the interlabial sulci.
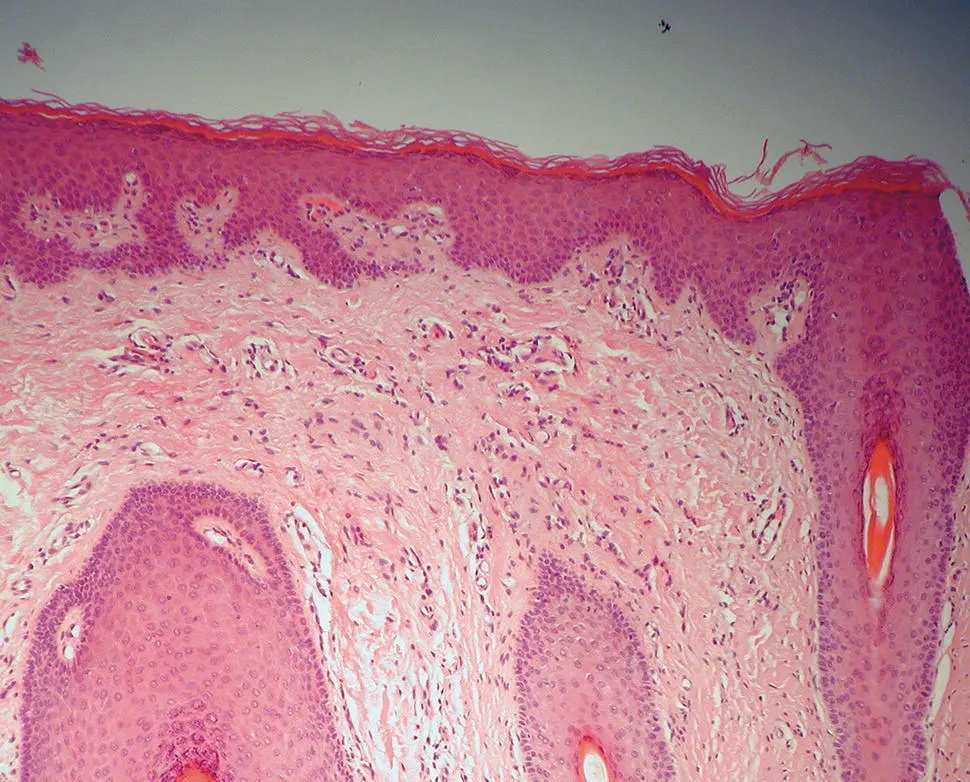
Figure 2.16 Histology of normal labium majus.
AGMLGs
It was originally thought that mammary tissue seen in the vulva was an embryological remnant of the mammary ridge. The AGMLGs were first described by van der Putte [ 31], and it is now clear that they are a distinct entity and are a normal component of anogenital skin [ 32]. They are found predominantly in the interlabial sulci of the vulva and have distinctive morphological, histological, and immunohistochemical features that are similar to the breast [ 33].
The morphology of the glands ranges from a simple wide duct with a few small diverticula to a complicated, convoluted tubular system that have features similar to those seen in the breast but without the lobules ( Figure 2.17). Most glands, however, consist of a coiled duct with diverticular extensions at irregular intervals along their length. The glands all have a straight excretory duct that opens directly onto the skin surface. The anogenital glands extend to 3.9 mm into the dermis, which is deeper than eccrine or apocrine glands [ 34]. They are lined by simple columnar epithelium resting on a layer of myoepithelium. The columnar epithelium extends into the straight excretory duct until a short distance from the surface and then gives way to non‐keratinised, stratified squamous epithelium without a myoepithelial layer. The lining epithelium may show columnar cell change in these AGMLGs [ 34].
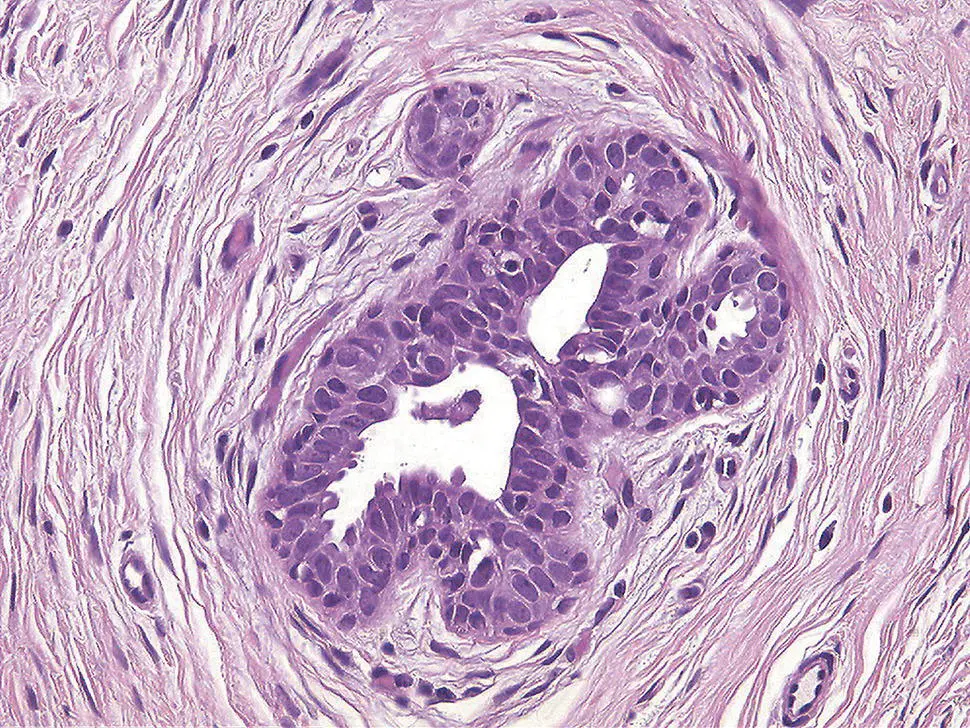
Figure 2.17 Lobulated anogenital mammary‐like gland with compact columnar epithelium
(courtesy of Dr James Scurry).
Labia minora
The inner and outer aspects of the labia minora are covered with non‐hair‐bearing skin, but sebaceous glands are still found, which open directly onto the skin. Eccrine glands are rarely seen. The dermis of the labia minora is composed mainly of elastic fibres and blood vessels with a rich innervation. The arrangement of blood vessels within the labia minora forms erectile tissue similar to that in the penile corpus spongiosus, their embryological counterpart in the male.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Ridley's The Vulva»
Представляем Вашему вниманию похожие книги на «Ridley's The Vulva» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Ridley's The Vulva» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.