Successful Training in Gastrointestinal Endoscopy
Здесь есть возможность читать онлайн «Successful Training in Gastrointestinal Endoscopy» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Successful Training in Gastrointestinal Endoscopy
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:3 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 60
- 1
- 2
- 3
- 4
- 5
Successful Training in Gastrointestinal Endoscopy: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Successful Training in Gastrointestinal Endoscopy»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Teaches trainee gastroenterologists the endoscopic skills needed to meet the medical training requirements to practice gastroenterology and helps clinical specialists refresh their skills to pass their recertification Successful Training in Gastrointestinal Endoscopy, Second Edition
Successful Training in Gastrointestinal Endoscopy, Second Edition
Successful Training in Gastrointestinal Endoscopy — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Successful Training in Gastrointestinal Endoscopy», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
One such evaluation process is called the Direct Observation of Procedural Skill (DOPS) form. This form focuses on six broad motor skill parameters and was developed by researchers as a means of assessing these skills following an intensive hands‐on training course [27, 48]. Another standardized skill evaluation form has been developed at the Mayo Clinic (Rochester, MN) in conjunction with the ASGE, which grades a spectrum of both cognitive and motor skills of trainees during colonoscopy. These component skills of colonoscopy were identified by a panel of expert endoscopists and educators and are based on the general training and competency recommendations outlined by professional societies [49]. From this, a blueprint for the evaluation tool was created, and based on this blueprint and refinement by the ASGE training committee, the Assessment of Competency in Endoscopy (ACE) was developed ( Table 6.4). Some version of this survey has been in use for over a decade at Mayo and is completed on every colonoscopy from the first day of a fellow's training until graduation. The supervising staff enters these data directly into the institution's endoscopy database during the procedure so that the performance data are connected to other procedural data such as cecal intubation time and withdrawal times as well as special therapies applied, polyp detection, and complications. This assessment tool was recently made available as part of the ProVation Endoscopy reporting software package used by a vast number of endoscopy centers. Linking this evaluation to the procedural database has allowed the avoidance of having staff duplicate much of the data already generated automatically as part of the procedure. Admittedly, the goal of completing a fellow skills assessment with every procedure is labor‐intensive and daunting but can certainly be accomplished. Alternatively, the use of assessment forms such as the DOPS or ACE could be performed on a periodic basis, giving instructors a “snap‐shot” in time of how a trainee compares to the expected learning curve.
Table 6.3 Competency metrics for continuous assessment
| Cognitive skills |
| Appropriate use of initial sedation |
| Continuous monitoring and management of patient comfort and depth of sedation |
| Identification of landmarks/awareness of scope location |
| Accuracy and sophistication of pathology recognition |
| Selection of appropriate tools and settings for therapy |
| Motor skills |
| Safe scope advancement |
| Loop reduction techniques |
| Depth of independent scope advancement |
| Cecal intubation time |
| Success/failure at TI intubation |
| Mucosal inspection during withdrawal |
| Application of tools for therapy |
The data collected from such an ongoing evaluation system allow reporting of a fellow's performance at any given point in their training as well as the comparison of the individual's scores to the average learning curve of his/her peers at the same points in training ( Figure 6.35). In the examples shown, progress reports can graphically depict the learning curves of any of the various competency parameters. In this example, the progress of three different first year fellows—A, B, and C (above, at, and below average, respectively)—is shown. This allows program directors to spot early those trainees who are falling off the learning curve and provide intervention earlier in training. Additionally, these metrics and average learning curves are valuable data for establishing criteria to define what performance equates to “competence” in a reliable, reproducible, and generizable manner. The concept of “competence” at present is rather limited in scope. A method that can formally define and assess competence such as ACE Tool or DOPS can be powerful tools. Each teaching institution should be encouraged to adopt some form of continuous assessment process whether using a comprehensive form such as the one described here or an ongoing skills assessment in a more limited form. Eventually, professional organizations and regulating organizations will require some type of direct measures of competence for all training portfolios as the parameters of cognitive and motor competence are increasingly better defined [50, 51].
Table 6.4 Assessment of Competence in Endoscopy (ACE) tool. This survey is completed by staff during each colonoscopy and grades a fellow's various cognitive and motor skills. This form is meant to augment the data already collected by the procedural database (such as medications administered, cecal intubation, and withdrawal times). Such a form allows for continuous assessment of a fellow's individual skills as they progress toward competence. (Copyrighted and used with permission of Mayo Foundation for Medical Education and Research.)
Modified from the Mayo Colonoscopy Skills Assessment Tool (© Mayo Foundation for Medical Education and Research) as reported in Sedlack RE. The Mayo Colonoscopy Skills Assessment Tool: a validation of a unique instrument to assess colonoscopy skills in trainees. Gastrointest Endosc 2010;72:1125–33. Used with permission.
| ASGE Assessment of Competency in Endoscopy (ACE). Colonoscopy Skills Assessment ToolFellow: Staff: Date of procedure: Time of Intubation: Time of Maximal Insertion Extent: Time of Extubation: |
| Fellow’s knowledge of the indication and pertinent medical issues (INR, Vitals, Allergies, PMH, etc.): □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Poor knowledge of patient’s issue, or started sedating without knowing the indication) □ 2. Intermediate (Missed an Important element, i.e. Allergies, GI Surgical History, or INR in pt on Coumadin) □ 3. Advanced (Missed minor elements) □ 4. Superior (Appropriate knowledge and integration of patient information) Management of patient discomfort during this procedure (Sedation titration, Insufflation management, Loop reduction): □ N/A Fellow observed □ 1. Novice (Does not quickly recognize patient discomfort or requires repeated staff prompting to act) □ 2. Intermediate (Recognizes pain but does not address cause [loop or sedation problems] in a timely manner) □ 3. Advanced (Adequate recognition and corrective measures) □ 4. Superior (Competent continuous assessment and management, i.e. intermittently reassess level of sedation and comfort) Effective and efficient use of air, water, and suction: □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Repeated prompting due to too much/little air, inadequate washing, or repeated suctioning of mucosa) □ 2. Intermediate (Occasional prompting due to too much/little air, inadequate washing or repeated suctioning of mucosa) □ 3. Advanced (Adequate use of air, water and suctioning, but room to improve on efficiency) □ 4. Superior (Efficient and effective management of washing, suctioning, and air) Lumen identification: □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Generally only able to recognize lumen if in direct view) □ 2. Intermediate (Can grossly interpret large folds to help locate which direction the lumen is located) □ 3. Advanced (Can use more subtle clues [Light/shadows, arcs of fine circular muscles in wall] but struggles at times) □ 4. Superior (Quickly and reliably recognizes where lumen should be based on even subtle clues) Scope steering technique during advancement: □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Primarily “Two‐hand knob steering”, unable to perform two steering maneuvers simultaneously) □ 2. Intermediate (Frequent 2‐hand knob steering, limited use of simultaneous steering maneuvers [i.e. torque, knob, advance]) □ 3. Advanced (Primarily uses torque steering, can perform simultaneous steering techniques) □ 4. Superior (Effortlessly combines simultaneous steering techniques [torque, knob, advance] to navigate even many difficult turns) Fine tip control: □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Primarily gross tip control only, frequently in red out) □ 2. Intermediate (Limited fine tip control, “frequently over‐steers turns, struggles with biopsy forceps/snare targeting”) □ 3. Advanced (loses fine control when keeping lumen or targeting tools at difficult turns when torque or knobs are needed) □ 4. Superior (Excellent fine tip control or tool targeting even in difficult situation.) Loop reduction techniques (pull‐back, external pressure, patient position change): □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Unable to reduce/avoid loops without hands‐on assistance) □ 2. Intermediate (Needs considerable coaching on when or how to perform loop‐reduction maneuvers) □ 3. Advanced (Able to reduce/avoid loops with limited coaching) □ 4. Superior (Without coaching, uses appropriate ext. pressure/position changes/loop‐reduction techniques) What is the farthest landmark the fellow reached without any hands‐on assistance? □ N/A. Fellow observed only or Procedure terminated before completion . □ 1.Rectum, □ 2. Sigmoid, □ 3. Splenic flexure, □ 4. hepatic flexure, □ 5. Cecum No TI attempt (Reached cecum with no attempt at TI intubation) □ 6. Cecum Failed TI attempt (Reached cecum but Failed attempt at TI intubation) □ 7. Terminal Ileum (Successful intubation of TI) □ 8. Other‐Post surgical anatomy encountered, fellow reached maximal intubation Adequately visualized mucosa during withdrawal □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Red out much of the time, does not visualize significant portions of the mucosa or requires assistance) □ 2. Intermediate (Able to visualize much of the mucosa but requires direction to re‐inspect missed areas) □ 3. Advanced (Able to adequately visualize most of the mucosa without coaching) □ 4. Superior (Good visualization around difficult corners and folds and good use of suction/cleaning techniques) Pathology identification/interpretation: □ N/A, Study was normal (Go to question 11) □ 1. Novice (Poor recognition of abnormalities. Misses or cannot ID significant pathology) □ 2. Intermediate (Recognize abnormal findings but cannot interpret. “erythema”) □ 3. Advanced (Recognizes abnormalities and correctly interprets. “colitis”) □ 4. Superior (Competent identification and assessment. “Mild chronic appearing colitis in a pattern suggestive of UC”) 10a. Independent polyp detection by fellow □ N/A. No polyps present □ 1. None (Staff identified all polyps) □ 2. Some (Fellow independently identified at least one polyp but not all polyps present) □ 3. All (Fellow independently ID’ed all polyps encountered) 10b. Accurate location of lesion/pathology: □ 1. Novice (Unable to use landmarks to ID location in the colon, “I don’t know”) □ 2. Intermediate (Understands landmarks but either does not recognize or incorporate into decision‐making process) □ 3. Advanced (Good understanding and recognition of landmarks but generalizes pathology location “Descending colon”) □ 4. Superior (Very specific about location, e.g.“Splenic Flexure region approx. 60 cm from the anal verge with a straight scope”) Interventions performed by fellow: CHECK ALL THAT APPLY □ N/A – Fellow did not perform any interventions (go to question 12) □ Biopsy □ APC Vascular lesion ablation (AVMs) □ Snare polypectomy □ Hemostasis (Hemoclip, electrocautery, etc.) □ Submucosal injection (Lift, Epinephrine, Tattoo) □ Other_____ 11a. What was the fellow’s participation in the therapeutic maneuver(s) (ability to apply tool effectively)? □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Performed with significant hands‐on assistance or coaching) □ 2. Intermediate (Performed with minor hands‐on assistance or significant coaching) □ 3. Advanced (Performed independently with minor coaching) □ 4. Superior (Performed independently without coaching) 11b. What was the fellows knowledge of the therapeutic tool(s)(tool selection, knowledge of set up, cautery setting, how to employ tool)? □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Unsure of the possible tool(s) indicated or settings for pathology encountered) □ 2. Intermediate (Able to identify possible appropriate tool choices but not sure which would be ideal [Snare vs lift & snare]) □ 3. Advanced (Independently selects the correct tool yet needs coaching on settings) □ 4. Superior (Independently identifies correct tool and settings as applicable) Overall Assessment: The fellow’s overall hands‐on skills: □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Learning basic scope advancement; requires significant assistance and coaching) □ 2. Intermediate (Acquired basic motor skills but still requires limited hands‐on assistance and/or significant coaching) □ 3. Advanced (Able to perform independently with limited coaching and/or requires additional time to complete) □ 4. Superior (Competent to perform routine colonoscopy independently) The fellow’s overall cognitive skills (Situational Awareness (SA)/abnormality interpretation/decision‐making skills): □ N/A. Not Assessed (i.e. Fellow observed procedure only) □ 1. Novice (Needs significant prompting, correction or basic instruction by staff) □ 2. Intermediate (Needs intermittent coaching or correction by staff) □ 3. Advanced (Fellow has good SA, and interpretation/decision‐making skills) □ 4. Superior (Competent to make interpretations and treatment decisions independently) |
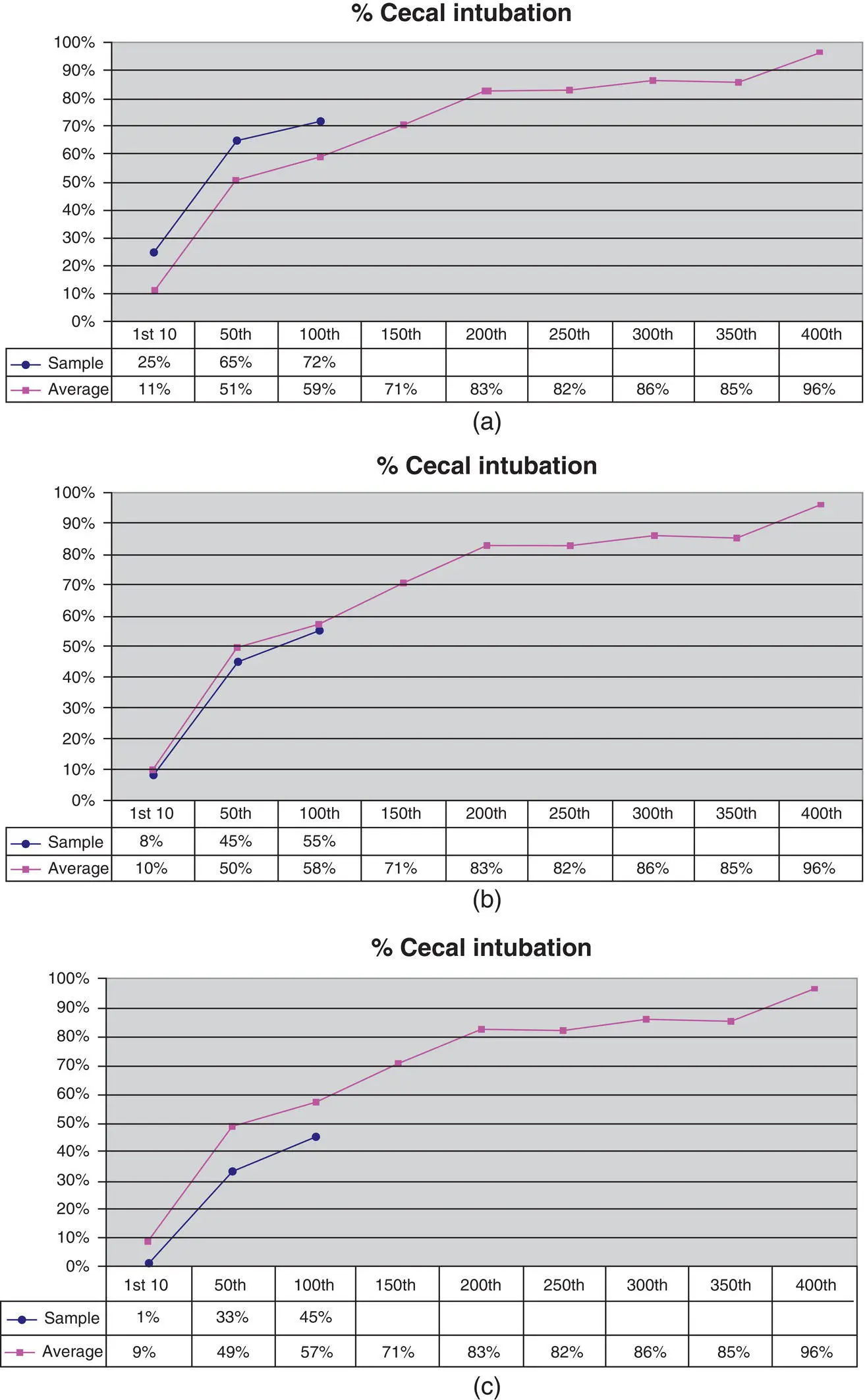
Figure 6.35 Learning curves. Mayo's colonoscopy skills assessment tool (MCSAT) allows ongoing monitoring of various metrics of an individual trainee's performance throughout training. These three images demonstrate how the learning curves of three different fellows (blue lines) might appear for the parameter of cecal intubation rates as compared to the average learning curves of their peers (Magenta). Fellow A is above the learning curve (a), B is following the curve closely (b), and C is repeatedly below the curve and might be identified for early remediation (c).
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Successful Training in Gastrointestinal Endoscopy»
Представляем Вашему вниманию похожие книги на «Successful Training in Gastrointestinal Endoscopy» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Successful Training in Gastrointestinal Endoscopy» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.