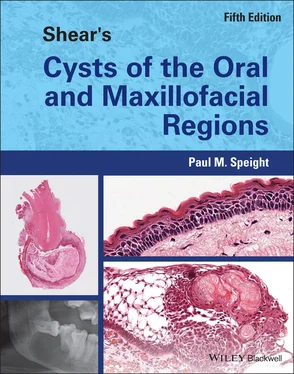
Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions
Здесь есть возможность читать онлайн «Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Shear's Cysts of the Oral and Maxillofacial Regions
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Shear's Cysts of the Oral and Maxillofacial Regions: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Shear's Cysts of the Oral and Maxillofacial Regions»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Shear’s Cysts of the Oral and Maxillofacial Regions
Shear’s Cysts of the Oral and Maxillofacial Regions Fifth Edition
Shear's Cysts of the Oral and Maxillofacial Regions — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Shear's Cysts of the Oral and Maxillofacial Regions», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Colgan et al. (2002 ) suggested that food impaction may have an important part to play. In 13 of their 15 cases the associated tooth was opposed by a maxillary molar and they proposed that the angulation of the affected tooth (usually distal) could promote food impaction into the pericoronal tissues around the crown. As further evidence for this they showed that four cases contained giant cells consistent with a foreign body reaction.
With regard to the mandibular buccal bifurcation cyst, studies have shown that the affected tooth is almost always tilted buccally ( Figure 4.4), giving prominence to the lingual cusps and often associated with increased pocket depth on the buccal aspect (Pompura et al. 1997 ; Philipsen et al. 2004 ). Stoneman and Worth (1983 ) suggested that the mesio‐buccal cusp of the first molar is the first to penetrate the oral mucosa during eruption, and that this would explain the buccal location of the cyst, but this explanation is at odds with the fact that the lingual cusps may erupt first in the buccally displaced tooth. However, it is not known whether this buccal inclination occurs as a result of displacement of the tooth by the cyst, or is present at eruption and may thus predispose to cyst formation. Since the cysts are rare, it is most likely that the associated tooth is buccally displaced at eruption and that this predisposes to inflammation in a buccal pocket and subsequent cyst formation. It is possible that the prominence of the lingual cusps and the buccal inclination may predispose to food impaction on the buccal aspect.
Relationship of the Paradental Cyst to the Dentigerous Cyst
As discussed previously (see ‘Frequency’), there is evidence that some clinicians and pathologists do not recognise the paradental cyst as an entity, but rather regard it as a variant of dentigerous cyst. Ackermann et al. (1987 ) suggested that although the paradental cyst may arise from follicular (reduced enamel) epithelium, the histogenesis is quite different and it should not be regarded as a variant of dentigerous cyst. They believed that the dentigerous cyst should be defined as a cyst enclosing the crown of a completely unerupted tooth.
Despite this, many clinicians and pathologists diagnose collateral lesions associated with partially erupted third molars as ‘inflamed dentigerous cysts’. Fowler and Brannon (1989 ) agreed with Ackermann et al. (1987 ) that a dentigerous cyst is, by definition, associated with an unerupted tooth, but also believed that the paradental cyst is a variant of dentigerous cyst. In this respect, a relationship to the dentigerous cyst may be suggested on the basis of a common origin from epithelium lining the dental follicle, with intraosseous (dentigerous cyst) and extraosseous (paradental cyst) variants associated with totally unerupted and partially erupted teeth, respectively.
One possible pathogenic mechanism for the paradental cyst is that it represents a developmental dentigerous cyst that has become laterally (and buccally) displaced by the eruption of the associated tooth, with subsequent inflammation. This seems unlikely, however, since the typical radiology of the paradental cyst (see Figures 4.2 and 4.5a) suggests that the dental follicle remains intact and is not dilated, and such a mechanism would not explain the consistent buccal location. An alternative proposal is that the paradental cyst is simply an inflammatory type of dentigerous cyst that arises as a result of inflammation of the pericoronal tissues surrounding the partially embedded crown of an impacted or erupting tooth. This would be a perfectly acceptable proposal, but for the fact that an inflamed and expanded pericoronal follicle would be indistinguishable from pericoronitis associated with inflammatory osteolysis. Yet paradental cysts show a very distinctive radiology with a buccally orientated radiolucency that is quite distinct from an expanded dental follicle (see ‘Radiological Differential Diagnosis’ and Figures 4.2and 4.5). For these reasons, we believe that inflammatory collateral cysts and dentigerous cysts show distinctive diagnostic features and should be designated as separate entities ( Box 4.2).
Histopathology
Paradental cysts associated with third molars are removed by enucleation of the cyst along with extraction of the associated tooth. Occasionally, the whole specimen is received intact ( Figure 4.6) and will show that the cyst is a sac‐like mass attached at the cementoenamel junction and located on the buccal aspect of the tooth roots. This is in contrast to a dentigerous cyst, which is also attached to the cementoenamel junction, but surrounds the crown of the tooth (see Figures 5.18 and 5.19). Careful examination with a probe will show that the lumen of the cyst is continuous with the periodontal or pericoronal pocket ( Figure 4.6b). This appearance is virtually diagnostic of an inflammatory collateral cyst.
Mandibular buccal bifurcation cysts are usually removed by enucleation or curettage and the tooth is left in situ . In this case the pathologist will often receive fragments of soft tissue that in places may resemble a cyst wall.
Histological examination shows non‐specific features that are indistinguishable from radicular cyst and it will be impossible to make a diagnosis without consideration of the clinical findings and review of the radiology. The cysts are lined by a hyperplastic, non‐keratinised, stratified squamous epithelium, which may be spongiotic and of varying thickness. There is an intense chronic or mixed inflammatory cell infiltrate associated with the hyperplastic epithelium and in the adjacent fibrous capsule ( Figure 4.7). As in radicular cysts, haemosiderin deposits, hyaline bodies, or accumulations of cholesterol crystals may be seen. An opening into the cyst lumen may also be seen and the epithelial lining may be continuous with sulcular or gingival epithelium at the periphery. Occasional cases may show focal accumulations of foreign body–type giant cells, consistent with impaction of food particles (Fowler and Brannon 1989 ; Colgan et al. 2002 ).
Treatment
Inflammatory collateral cysts are simple cysts and there is no evidence to suggest that recurrence is a problem. Paradental cysts associated with third molars are usually enucleated along with the offending tooth. However, if the tooth is not impacted or angulated and appears to be erupting, it may be preserved and should continue to erupt into a normal occlusion.
Mandibular buccal bifurcation cysts are often enucleated without removal of the associated tooth, which then erupts normally. Nevertheless, removal of the cyst may not be necessary, since there is good evidence that it may resolve after more conservative treatment. Marsupialisation of the cyst has been found to be effective and has resulted in compete regression, with normal eruption of the associated tooth and restoration of a normal gingival profile (Lizio et al. 2011 ). Cysts have also been shown to resolve after simple probing and irrigation, or even to heal spontaneously as the tooth erupts (David et al. 1998 ; Gomez et al. 2001 ; Zadik et al. 2011 ). That these cysts are self‐limiting and may resolve spontaneously is supported by the fact that they rarely reach a large size and they do not occur in adults.

Figure 4.7 Paradental cyst adjacent to the root of an impacted mandibular third molar. The cyst is lined by non‐keratinised stratified squamous epithelium of variable thickness and showing areas of proliferation and inflammation in the wall.
Source: Courtesy of Prof G.T. Craig.
Читать дальшеИнтервал:
Закладка:
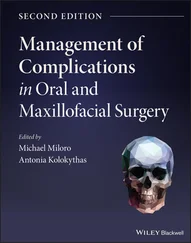
Похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions»
Представляем Вашему вниманию похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Shear's Cysts of the Oral and Maxillofacial Regions» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.