1 ...7 8 9 11 12 13 ...28 In 2016–2018, the MMR among women living in the most deprived areas was 15.3 compared with 5.7 for women living in the most affluent areas, a close to threefold difference. Attention should also be focused on women who book late or are poor attenders for antenatal care. In 2016–2018, 22% of women who died booked late, 61% did not receive the recommended level of antenatal care and 27% did not receive the minimum level of antenatal care as defined by National Institute for Health and Care Excellence (NICE) guidance.
In the 2016–2018 report black women have more than fourfold higher MMRs than white women, a disparity which has been evident for many years and has been worsening more recently. The increase is less among other ethnic groups ( Table 2.2), but is also significantly higher in women from Asian and mixed ethnic backgrounds. Women recently arrived from overseas often have communication difficulties and are at particular risk.
Table 2.2 Estimated maternal mortality rates by ethnic group, England 2016–2018
| Ethnic group (England only) |
Total maternities |
Deaths ( n ) |
Rate/100 000 (95%CI) |
Relative risk (95%CI) |
| White (inc. not known) |
1 486 428 |
117 |
7.87 (6.51–9.43) |
1 (Ref.) |
| Asian |
191 145 |
28 |
14.65 (9.73–21.17) |
1.86 (1.19–2.83) |
| Black |
81 704 |
28 |
34.27 (22.77–49.53) |
4.35 (2.77–6.62) |
| Chinese/others |
75 270 |
6 |
7.97 (2.93–17.35) |
1.01 (0.36–2.27) |
| Mixed |
31 823 |
8 |
25.14 (10.85–49.53) |
3.19 (1.35–6.50) |
2.5 Direct deaths
Hypertensive disease
The number of deaths from pre‐eclampsia is a fraction of what it was in 1952–1954 ( Table 2.3) and most recently has fallen dramatically from 19 in 2006–2008 to 10 deaths in 2009–2011, nine deaths in 2010–2012 and then six deaths in 2014–2016. This reduction is largely due to the introduction of guidelines on fluid management and none of the recent deaths have been due to pulmonary or cerebral oedema. However, there is a continuing problem with failure to control systolic hypertension, and preventing intracranial haemorrhage remains a challenge. Among the recent recommendations the following points are emphasised:
Epigastric pain in the second half of pregnancy should be considered to be the result of pre‐eclampsia until proved otherwise
Keep blood pressure (BP) below 150/100, and very high systolic BP is a medical emergency with urgent treatment needed
Neuroimaging should be performed if a woman with hypertension or pre‐eclampsia has focal neurology, severe or atypical headache or incomplete recovery from a seizure
Stabilising the mother including controlling her BP is vital prior to intubation
New‐onset hypertension or proteinuria needs prompt referral with clear communication between health professionals
Table 2.3 The changes in direct deaths reported to the CEMDs, 1952–2018
| Cause |
1952–1954 (England+Wales) |
2006–2008 (UK) |
2009–2011 (UK and Ireland) |
2010–2012 |
2014–2016 |
2016–2018 |
| Hypertensive disease |
246 |
19 |
10 |
9 |
6 |
4 |
| Obstetric injury |
197 |
0 |
7 |
7 |
1 |
4 |
| Haemorrhage |
188 |
8 |
14 |
11 |
17 |
10 |
| Early pregnancy/abortion |
153 |
0 |
– |
7 |
3 |
7 |
| Thromboembolism |
138 |
18 |
30 |
26 |
32 |
33 |
| Anaesthesia |
49 |
7 |
3 |
4 |
1 |
1 |
| Genital tract sepsis |
42 |
26 |
15 |
12 |
11 * |
12 * |
*Now reported as pregnancy‐related sepsis, so now includes urinary tract infections.
Some of these recommendations are directed at non‐obstetricians, and, unfortunately, maternity staff do not always recognise the need for effective control of BP.
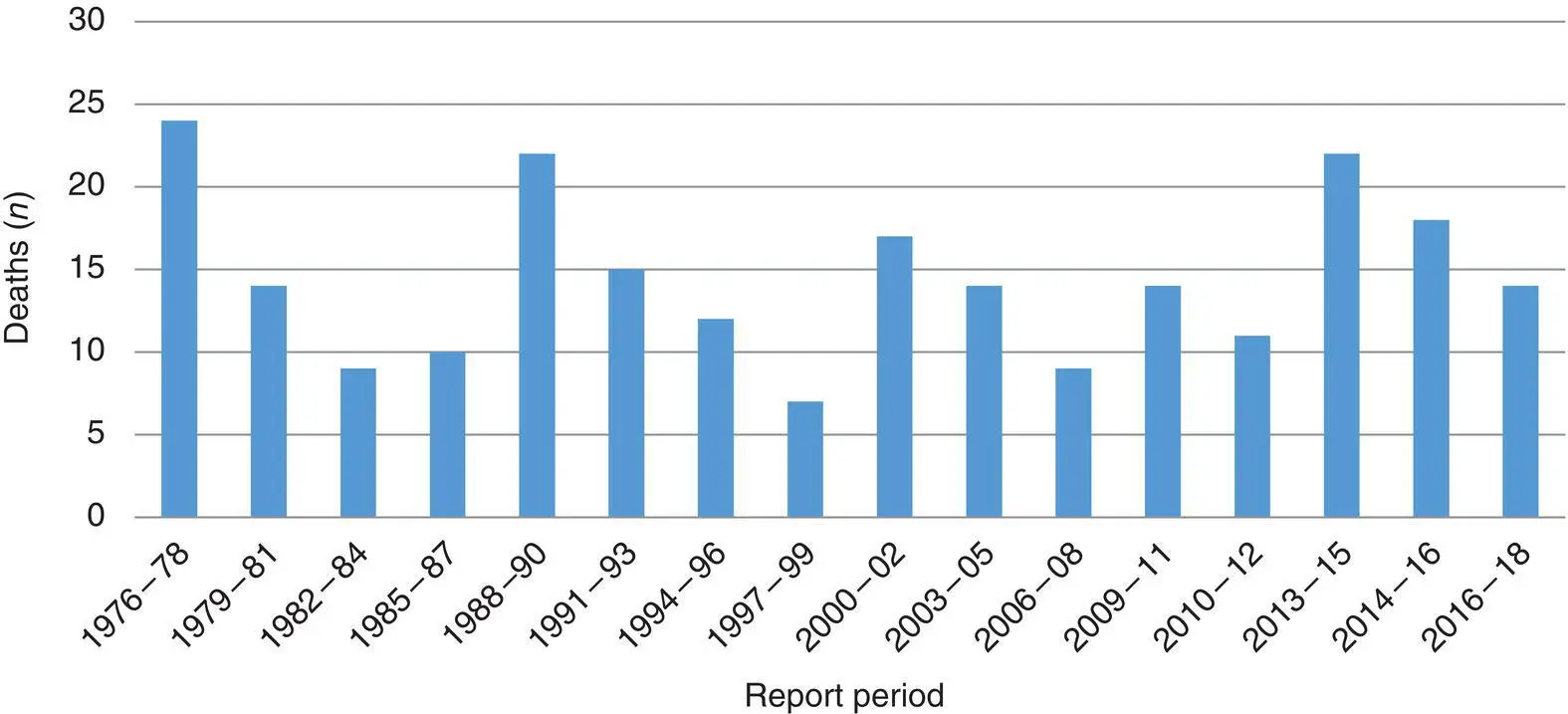
Over the past 40 years, deaths from haemorrhage have fluctuated ( Figure 2.1), which may represent relaxation and tightening of standards. For example, the peak in 1988–1990 included cases where doctors had ignored the recommendation that CS for placenta praevia should be carried out by a consultant.
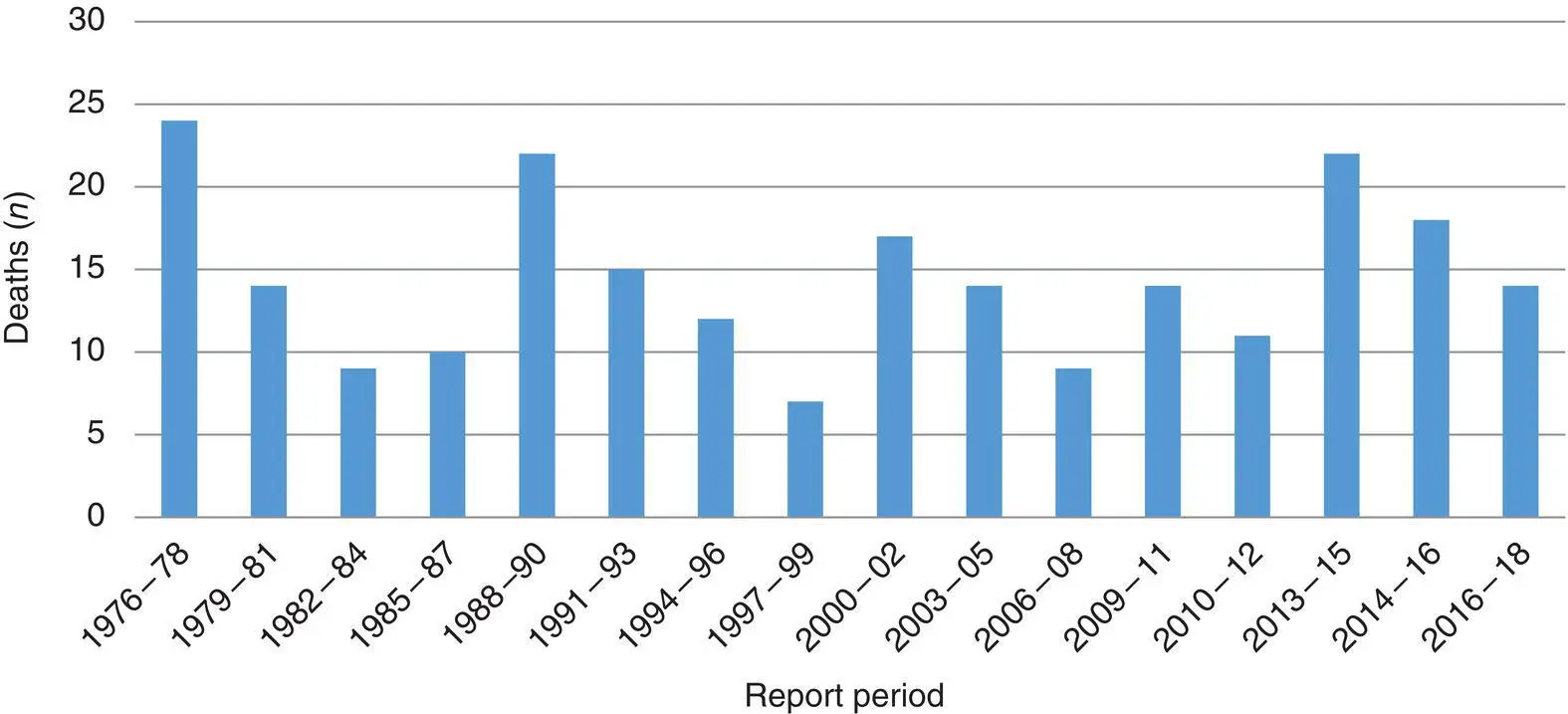
Figure 2.1 Deaths from haemorrhage reported to the CEMDs, 1976–2018
It is important, however, to see these numbers in context. Haemorrhage is by far the most common life‐threatening complication of childbirth: surveys of severe morbidity show that haemorrhage of >2.5 litres occurs once in about 300 births. Therefore over a 3‐year period with more than 2 million births in the UK, several thousand cases are treated successfully.
In 2016–2018, the total of 14 deaths due to haemorrhage included two cases of uterine atony, three of morbidly adherent placenta, three of abruption, two of uterine inversion and four of genital tract trauma. In 79% of cases there was room for improvements in care, and the main messages focused on:Ensuring a senior clinician takes a ‘helicopter view’ of the management of a woman with major obstetric haemorrhage to coordinate all aspects of care
Early recognition (especially when haemorrhage is concealed) including awareness of the signs of uterine inversion
Ensuring that the response to obstetric haemorrhage is tailored to the proportionate blood loss as a percentage of circulating blood volume based on a woman’s body weight
Early correction of coagulopathy
Progressing to hysterectomy when bleeding is uncontrolled, particularly from a morbidly adherent placenta or uterine rupture
Every triennium, one or more deaths occur in women who refuse blood transfusion and guidelines have been issued about the management of such patients. Placenta praevia associated with a uterine scar is particularly dangerous and all women with a previous CS should have a scan for placental localisation in the second trimester and, if low lying, again at 32 weeks.
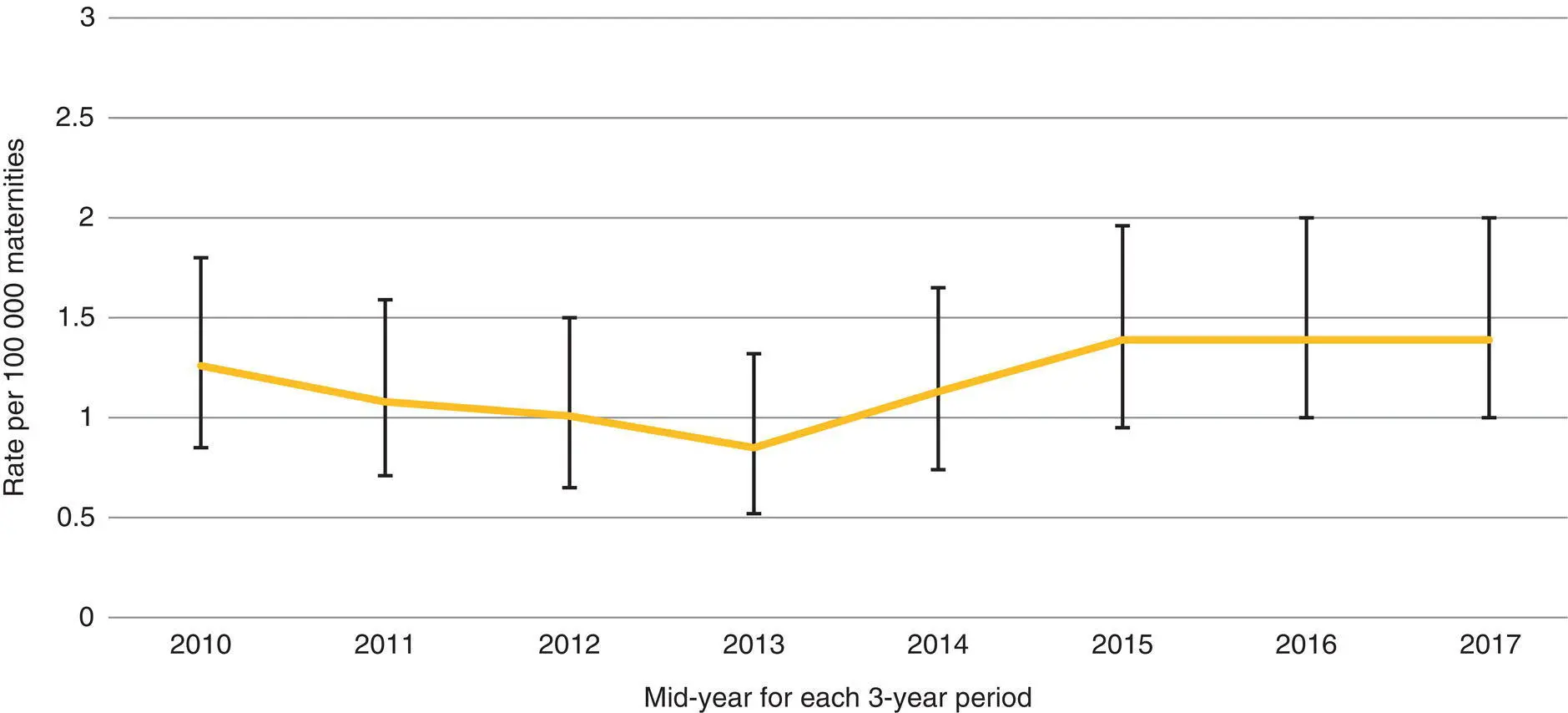
Thromboembolism has been the leading direct cause of maternal death in the UK since 1985, but while the number of deaths fell dramatically from 41 to 18 between 2003–2005 and 2006–2008, this improvement has not been sustained. In the 1990s, a previous fall occurred after the RCOG published recommendations on thromboprophylaxis at CS. Deaths during pregnancy and after vaginal delivery, however, continued to rise and these were targeted by a further RCOG guideline in 2004. These categories fell sharply in 2006–2008, the first full triennium after the new guideline was published. However deaths from thromboembolism have risen again and in 2016–2018 there were 33 ( Figure 2.2).
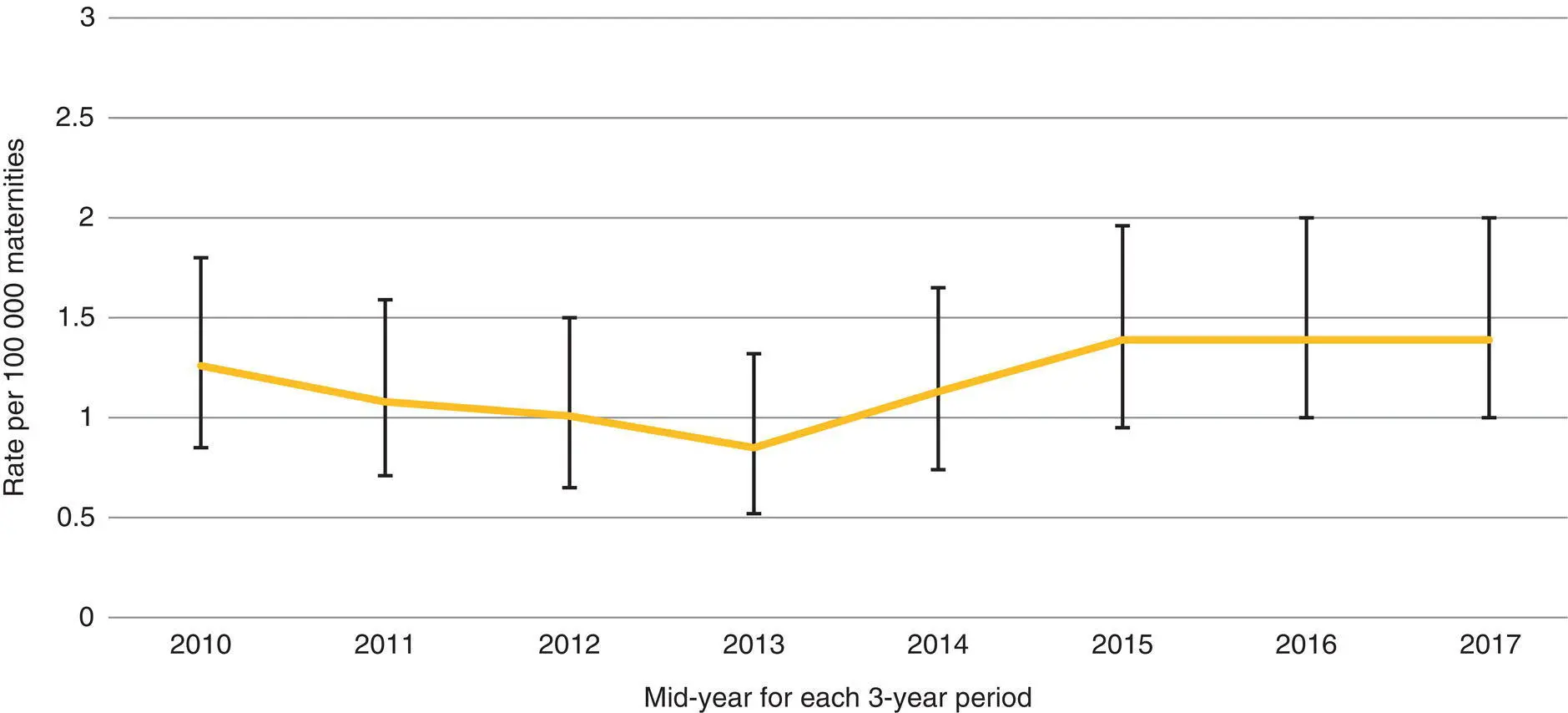
Figure 2.2 Maternal mortality from venous thromboembolism, 3‐year rolling rates in the UK, 2010 to 2017
The most important risk factor for thromboembolism is obesity and the current guidance includes weight‐specific dosage advice on thromboprophylaxis. Risk assessment early in pregnancy is the key to reducing mortality further; this message needs to be heard in gynaecology wards and early pregnancy assessment units as well as in maternity units. However, a clear message from the 2020 report is that there remains confusion about risk assessment scores, which are done inaccurately in many of the cases reviewed.
Читать дальше