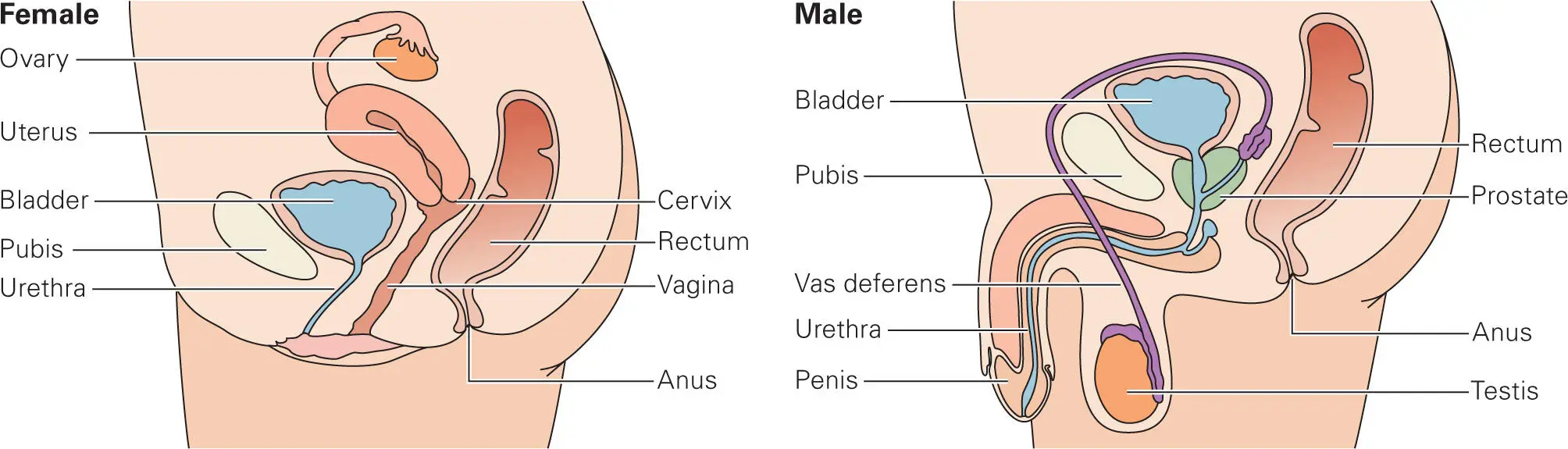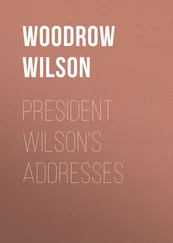
Figure 2-8. Comparison of the female and male urogenital tracts. Anatomical differences between the female and male urogenital tracts result in different environments and physical barriers that lead to different bacteria colonizing different sites. Physical barriers include a sphincter at the opening of the urethra that prevents ascent of microbes to the bladder and kidney. The urethra is shorter in females than males. Flushing of the bladder and urethra with urine removes adherent bacteria. Secretion of mucin blocks microbes from gaining access to the epithelial surface. A cervical mucus plug protects the uterus and fallopian tubes in females. Lactobacillus species, major resident bacteria in healthy females, protect the vaginal cavity from other bacteria that might enter from the anal area, which is relatively close to the vaginal opening. Sexually active partners exchange their resident microbiota with each other.
Altered conditions, such as pH changes or obstructions, can facilitate certain pathogens (e.g., E. coli, Proteus mirabilis, Staphylococcus saprophyticus, and Klebsiella species) to colonize the urethra and cause urinary tract infections (UTIs), especially in women. Almost 95% of UTIs are attributed to bacteria that normally reside at the opening of the urethra and travel up to the bladder and occasionally as far as the kidney. Women are more likely to get UTIs because in females the urethra is much shorter and closer to the anus. Some anatomical obstructions of the ureter or the urethra, such as prostate enlargement, kidney transplant, or bladder or kidney dysfunction, as well as indwelling catheter use, can impair bacterial clearance by urine and promote bacterial growth and infection.
In the vagina, a cervical plug protects the uterus and fallopian tubes from invasion by bacteria. The vagina is lined by a stratified epithelium, which produces a variety of protective defense mechanisms, including lysozyme, lactoferrin, small antimicrobial cationic peptides, and proteins (such as secreted IgA and IgG antibodies, secretory leukocyte protease inhibitors, and various cytokines and chemokines). The resident microbiota plays an important protective function against pathogens in the female genital tract. The application of molecular sequencing technologies over the past decade has contributed greatly to our understanding of urogenital microbiome composition and dynamics. In sexually active partners, the microbiota exchange freely and influence each other. There are also age-specific changes to the microbiomes and immune functions that occur, especially in response to hormones in women. Resident vaginal bacteria are thought to help prevent acquisition of sexually transmitted infections, such as HIV.
Lactobacillus species are the major resident vaginal bacteria found in healthy humans. Lactobacillus bacteria ferment glycogen, which is abundantly produced in the vaginal tract. These bacteria produce hydrogen peroxide and lactic acid, which helps maintain a weakly acidic (pH 4–5) environment that serves to inhibit the growth of other microbes, thereby preventing infection by yeast (vulvovaginal candidiasis or vaginitis) and bacteria (bacterial vaginosis). Humans are unique among primates in having a vaginal microbiome dominated by Lactobacillus species, though it is not known why. How the vaginal mucosa tolerates chronic colonization with Lactobacillus species, while still protecting against colonization by other microbes, is an area of active research.
Special Defenses of the Respiratory Tract
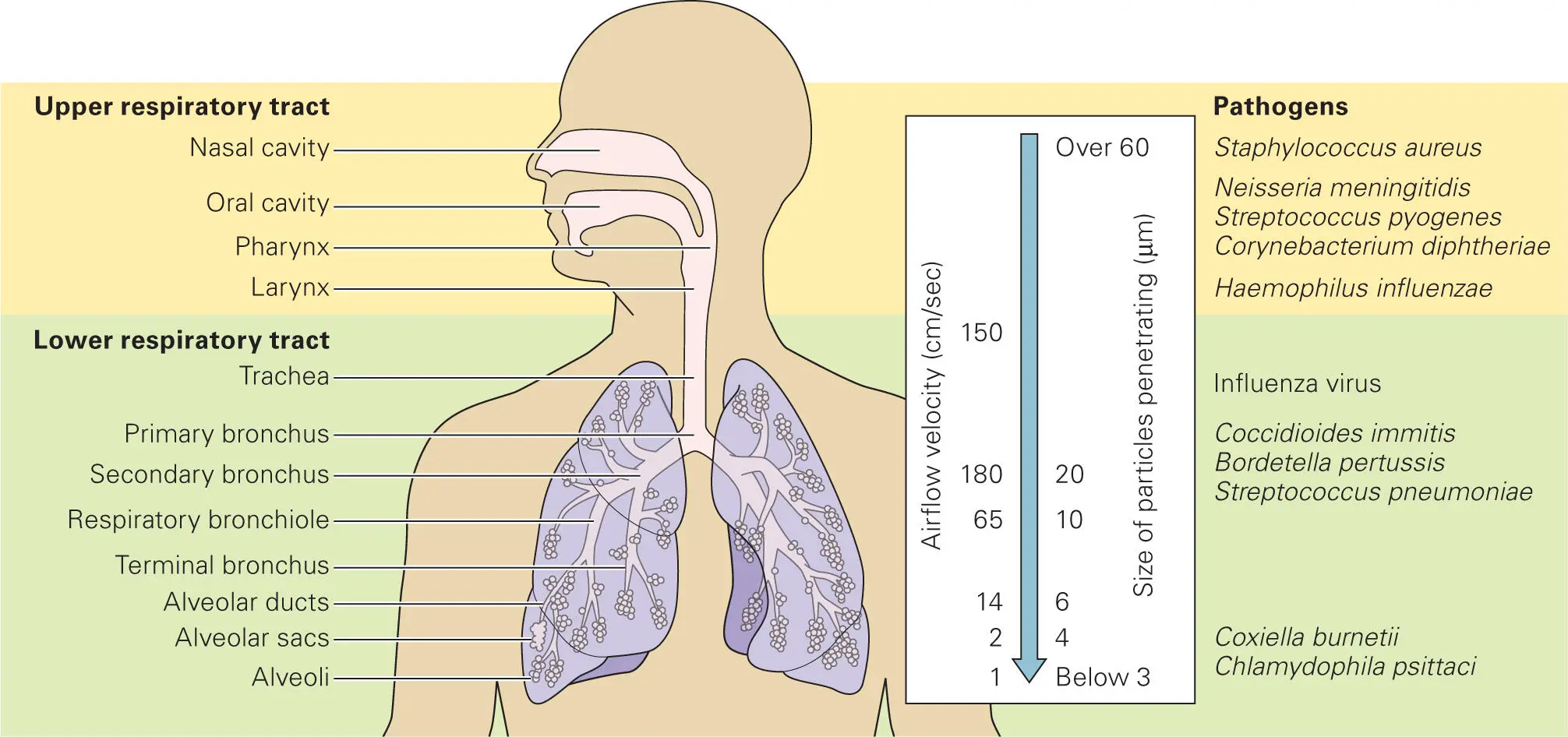
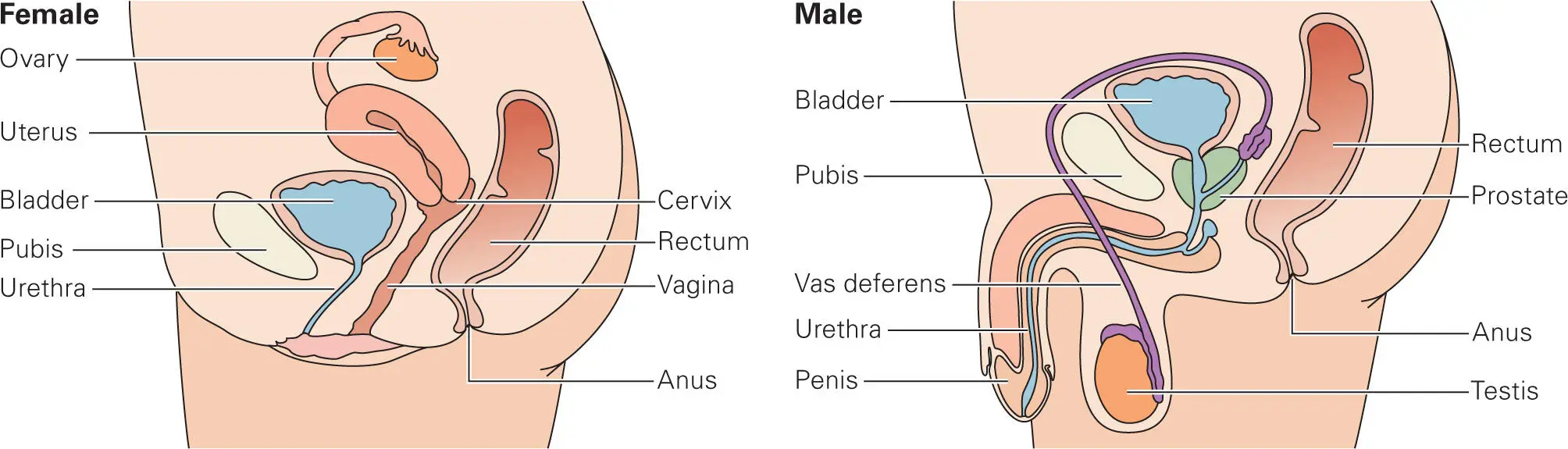
The respiratory system is comprised of a ciliated epithelial cell layer that is interspersed with goblet cells that secrete mucin. In the respiratory tract (as well as in the fallopian tubes of the vaginal tract), there are specialized ciliated columnar cells, whose elongated protrusions (cilia) continuously wave in the same direction. The waving action of the cilia propels mucus blobs out of the area. Airway epithelial cells also secrete collectins (collagen-containing C-type lectins), including surfactants A and D that bind to bacterial lipopolysaccharide (LPS), defensins and other antimicrobial peptides, and proteases. Hospitals often encounter problems associated with comatose patients, in which the absence of a normal cough reflex and reduced mucociliary clearance result in an increased susceptibility to respiratory infections. Turbulence of airflow from breathing, coughing, and sneezing serves to expel microbes out of the lungs, sometimes at velocities reaching over 150 cm/sec. In hospitals, problems can occur with respirators, which introduce air with tiny water droplets potentially contaminated with pathogens directly into the lung, thereby bypassing the upper respiratory airflow and mucociliary defenses.
The upper and lower respiratory tracts have different environments, and different commensal and pathogenic microbes are associated with the different areas ( Figure 2-9). A healthy lower respiratory tract lacks significant microbiota, while a few bacteria normally colonize the upper respiratory tract, most notably Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and nontoxigenic Corynebacterium diphtheriae, all of which are potential pathogens and are known to cause upper and lower respiratory infections when the immune system is impaired. In lung diseases such as asthma, cystic fibrosis, and chronic obstructive pulmonary disease, other pathogens also colonize the lungs, including Pseudomonas aeruginosa, Burkholderia cepacia, and Mycoplasma pneumoniae. In humans, colonization of the lower respiratory tract with Bordetella pertussis always leads to disease symptoms of whooping cough.
Figure 2-9. The upper and lower respiratory tract. The respiratory system is comprised of a ciliated epithelial cell layer that secretes mucus. Turbulence of airflow and mucociliary action help keep the lungs clear of particles and microbes. The upper respiratory tract includes the nose, nasal cavity, mouth, throat (pharynx), and voice box (larynx). The upper respiratory tract is often colonized by Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and nontoxigenic Corynebacterium diphtheriae. These bacteria can be opportunistic pathogens under certain conditions or when they colonize the lower respiratory tract. The lower respiratory tract includes the trachea, bronchi, and lungs (alveoli). The lungs are normally clear of bacteria, but can be invaded by opportunistic or outright pathogens during infection or under certain conditions. Data from Madigan MT, Martinko JM, Stahl D, Clark DP. 2015. Brock Biology of Microorganisms, 13th ed. Pearson, Upper Saddle River, NJ.
Immune Defenses of the Skin and Mucosa
Although this chapter focuses on the protective physical and biochemical barriers provided by intact skin and mucosa, it is important to note that these barriers are backed up by specialized portions of the immune system, which will be described in more detail in subsequent chapters. For example, bacteria that manage to get past the epidermis through cuts or burns encounter a specialized cell type called Langerhans cells. Langerhans cells belong to a class of cells called dendritic cells (DCs) that process the invading bacteria and activate the immune cells of the skin-associated lymphoid tissue (SALT). We will discuss the role of phagocytes (e.g., macrophages and dendritic cells) in chapter 3when we cover “The Innate Immune System: Always on Guard.”
Читать дальше