21 19 Recording the maxillo-mandibular relationship The denture bases Natural tooth contacts in partially dentate patients The registration material A passive process The process Checking the registration
22 20 Prescribing the upper wax contour Using the previous denture as a guide Lip support Incisal level and the alar–tragal plane Buccal corridors Other useful markers Tongue space and assessing speech
23 21 Prescribing the lower wax contour The tongue Lip support Incisal level and plane Buccal relationship Vertical dimensions, tongue space and speech
24 22 Tooth selection and arrangement Biological markers Tooth shapes Tooth sizes Tooth shade and characterisation Other considerations
25 23 Occlusal dimensions and occlusal schemes Conform or reorganise? Occlusal schemes Complete denture occlusal schemes Facebows
26 24 Respecting the neutral zone Diagnosis Managing the neutral zone The formal neutral zone impression Effects of respecting the neutral zone
27 25 Assessing trial prostheses What should be checked at try-in? Managing occlusal discrepancies
28 26 Fitting and reviewing finished prostheses Returning on casts Checking the fitting surface Checking occlusal contacts Reviewing the prostheses
29 27 Copying features from existing prostheses Tooth arrangements Fitting surface Full denture contour Modifying prostheses prior to copying How to create modified copy dentures
30 28 Classifying partial prostheses and material choices Kennedy Classification Applegate Classification Potential difficulties with each class Material choice
31 29 Designing partial prostheses Preliminary registration Other necessary information A system of design
32 30 Saddles, rests and clasps Saddles Rests Direct retention – clasps Indirect retention
33 31 Connectors and bracing Bracing Major and minor connectors
34 32 Surveying and preparing guide planes Should I survey for acrylic dentures? Path of natural displacement Path of insertion Guide planes Modifying the dentition
35 33 Designing frameworks – case examples Example 1 – Upper Kennedy Class I, modification I Example 2 – Lower Kennedy Class III, modification I Example 3 – Upper Kennedy Class III, modification I Example 4 – Upper Kennedy Class III, modification I Example 5 – Upper Kennedy Class III, modification I Example 6 – Lower Kennedy Class II
36 34 Precision attachments – the fixed–removable interface Classifying precision attachments Semi-precision rests
37 35 Dealing with frameworks and substructures Try-in of the framework Alloy teeth Accounting for additions Protecting small anterior saddles Altering clasps
38 36 The altered cast technique and the RPI system The altered cast technique The RPI system
39 37 Swing-lock prostheses What is a swing-lock prosthesis? Indications Contraindications Assessing the periodontal condition The latch assembly Retentive elements Connector design
40 38 Gingival veneers Contraindications Veneering materials Indirect technique Retention Silicone vs acrylic Shade taking
41 39 Immediate and training prostheses Complete immediate dentures Partial immediate dentures Training prostheses
42 40 Occlusal splints Splint types Occlusal coverage Records for construction
43 41 Implant-supported mandibular overdentures Planning Construction Maintenance
44 42 Principles of restoring maxillary defects Primary impressions Major impressions Framework designs Obturator bungs
45 43 Tissue conditioners, liners and re-basing Tissue conditioners Soft liners Degradation Re-basing
46 44 Maintaining adequate oral hygiene The impact of partial prostheses Complicating factors Cleaning partial and complete prostheses Fixed prostheses
47 45 Troubleshooting loose or painful dentures Loss of retention and displacement Pain underneath denture bases Other causes of pain
48 46 Gagging, other difficulties and making a referral Managing the gagging patient Tongue spread and lip activity Speech problems Referral process
49 47 Summary of procedural stages Prescribing the placement of teeth and recording jaw relations Partial denture design Partial denture provision Complete denture provision Modified copy denture provision Implant-supported mandibular overdenture provision
50 Appendices Appendix 1: Complete denture assessment proforma Appendix 2: Restorative assessment proforma Appendix 3: Referral letters Appendix 4: Partial denture design sheet Recommended and supplementary reading
51 Index
52 End User License Agreement
1 Cover
2 Table of Contents
3 Chapter
1 ii
2 iii
3 iv
4 viii
5 2
6 3
7 4
8 5
9 6
10 7
11 8
12 9
13 10
14 11
15 12
16 13
17 14
18 15
19 16
20 17
21 18
22 19
23 20
24 21
25 22
26 23
27 24
28 25
29 26
30 27
31 28
32 29
33 30
34 31
35 32
36 33
37 34
38 35
39 36
40 37
41 38
42 39
43 40
44 41
45 42
46 43
47 44
48 45
49 46
50 47
51 48
52 49
53 50
54 51
55 52
56 53
57 54
58 55
59 56
60 57
61 58
62 59
63 60
64 61
65 62
66 63
67 64
68 65
69 66
70 67
71 68
72 69
73 70
74 71
75 72
76 73
77 74
78 75
79 76
80 77
81 78
82 79
83 80
84 81
85 82
86 83
87 84
88 85
89 86
90 87
91 88
92 89
93 90
94 91
95 92
96 93
97 94
98 95
99 96
100 97
101 98
102 99
103 100
104 101
105 102
106 103
107 104
108 105
109 106
110 107
111 108
112 109
113 110
114 111
115 112
116 113
About the companion website
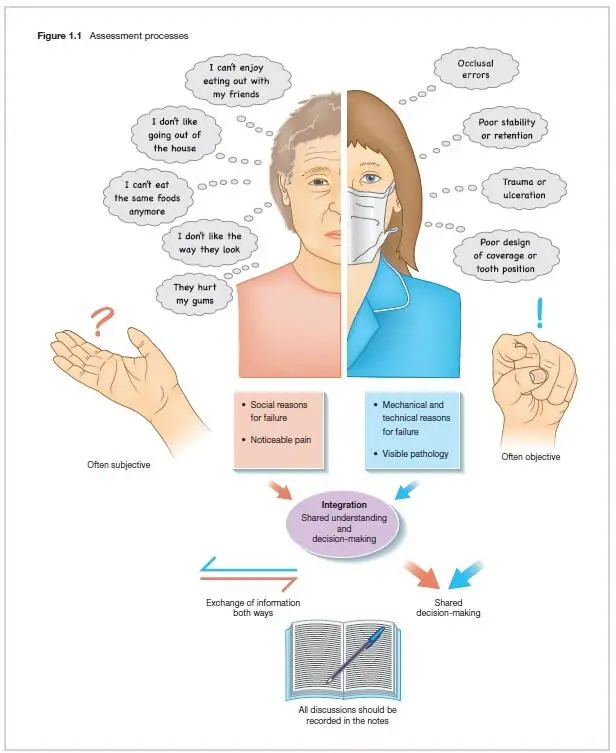
Removable prosthodontics is often described as a ‘black art’ – the Marmite of dentistry; practitioners tend to either love it or hate it. Fortunately, we love it – and with some simple guidance, hopefully you will too. Like most operative interventions, success depends on:
The skill of the dentist
The technical difficulty of the case
The patient's perceptions, ideas and expectations
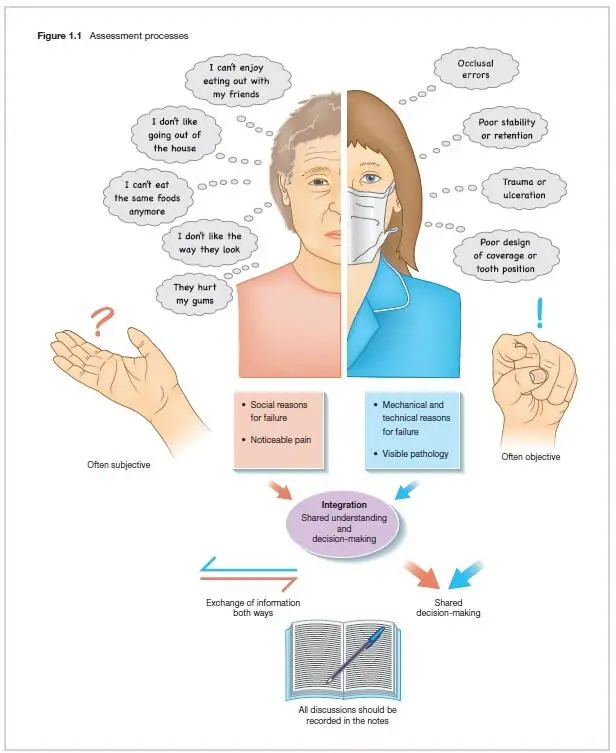
Providing prostheses that are satisfactory to the patient is a challenge – and there are many reasons why patients can be dissatisfied with the finished result. Many relate to social aspects of patients’ lives – how they are able to interact with others, particularly when eating and speaking. Common reasons include:
Unacceptable aesthetics
Inability to chew food properly
Inability to enjoy the same foods as before
Problems with speech
Discomfort or persistent pain
Disagreements over time and cost
Despite the diversity of complaints, there is often a common thread running through them all – lack of information exchange and an inappropriate level of patient expectation. We would therefore argue that the most important skill when making satisfactory removable prostheses is that of communication.
Communication and expectations
Читать дальше