20 20 Martin, R.M., Donovan, J.L., Turner, E.L. et al. (2018). Effect of a low‐intensity PSA‐based screening intervention on prostate cancer mortality. The CAP randomized clinical trial. Journal of the American Medical Association 319 (9): 883–895.
21 21 Schröder, F.H., Hugosson, J., Roobol, M.J. et al. (2014). Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow‐up. Lancet 384 (9959): 2027–2035.
22 22 Andriole, G.L., Crawford, E.D., Grubb, R.L. et al. (2009). Mortality results from a randomized prostate‐cancer screening trial. New England Journal of Medicine 360 (13): 1310–1319.
23 23 Sturgeon, K.M., Hackley, R., Fornash, A. et al. (2018). Strategic recruitment of an ethnically diverse cohort of overweight survivors of breast cancer with lymphedema. Cancer 124 (1): 95–104.
1 1 https://www.nimhd.nih.gov/about/overview/history/
2 2https://www.whitehouse.gov/wp‐content/uploads/2017/11/Revisions‐to‐the‐Standards‐for‐the‐Classification‐of‐Federal‐Data‐on‐Race‐and‐Ethnicity‐October30‐1997.pdf
3 3https://www.healthypeople.gov/2020/about/foundation‐health‐measures/Disparities
4 4https://www.nimhd.nih.gov/about/overview/research‐framework.html
5 5 https://grants.nih.gov/grants/funding/women_min/guidelines.htm
2 Getting Under the SkinPathways and Processes that Link Social and Biological Determinants of Disease
Chandra L. Jackson1, Rada K. Dagher2, Jung S. Byun3, Tilda Farhat4, and Kevin L. Gardner5
1 Epidemiology Branch, Social and Environmental Determinants of Health Equity, National Institute of Environmental Health Sciences, National Institutes of Health, Cary, NC, USA
2 National Institutes of Health, National Institute on Minority Health and Health Disparities, Division of Scientific Programs, Bethesda, MD, USA
3 National Institutes of Health, National Institute on Minority Health and Health Disparities, Division of Intramural Research, Bethesda, MD, USA
4 National Institutes of Health, National Institute on Minority Health and Health Disparities, Office of Science Policy, Planning, Evaluation, and Reporting, Bethesda, MD, USA
5 Department of Pathology and Cell Biology, Columbia University Medical Center, New York, NY, USA
A fundamental aspect of health disparities research is to understand the differential influences through which “where” and “how” we live affects our daily lives, and to provide everyone with an opportunity to reach and maintain their greatest health potential. “Where and how” we live encompasses, for instance, how we feed, how we sleep, and how we feel. It is also characterized by the differing ways in which we each respond to the vicissitudes of life. These influences on health are complex, multifactorial, interact with each other, accrue throughout the life course, and differentially affect various populations.
The domains that have the greatest influence on health and health disparities include the healthcare system, the sociocultural environment, the physical environment, and behavioral and biological determinants. Of note, modifiable environmental exposures and social factors, combined with a certain level of susceptibility may trigger epigenetic changes, thus producing biological processes contributing to health disparities. These domains are inextricably linked and may combine to produce synergistic effects on health, but their impacts are not distributed uniformly throughout the population. Several diseases and conditions can occur with increased frequency and severity (producing worse outcomes) in certain population groups. Understanding how these domains interact and combine to determine health outcomes (along the dimensions of race, ethnicity, socioeconomic status, and lifestyle) requires a transdisciplinary approach [1]. A transdisciplinary perspective cuts across different areas of expertise while filling in gaps of knowledge and understanding. Through cooperative and integrated efforts, subject matter experts must work together across disciplines and with communities to understand the causes/determinants and environmental or social pathways, as well as biological mechanisms of health disparities in order to implement interventions to eliminate or reduce disparities. A precision perspective in this effort requires the recognition of heterogeneity in the environmental, social, and behavioral influences. It also requires an understanding of how population‐specific differences in the magnitude of environmental, social, and behavioral influences may be fundamental causes of disparities in disease incidence, progression, and outcomes. Effective interventions—whether social, behavioral, or therapeutic—to eliminate or mitigate health disparities may depend on how thoroughly we understand the biological underpinnings of the contributions of the environment and society (including their influences on behavior) to disease. Developing such interventions will require the combined efforts of interdisciplinary teams, including, for instance, social, behavioral, environmental, and translational scientists. Moreover, understanding the biology of disease and how it may be exacerbated by environmental or behavioral influences will also provide new insights that will assist in identifying population‐specific differences in disease susceptibility across the life course, as well as effective interventions at the biological, behavioral, societal, and environmental levels.
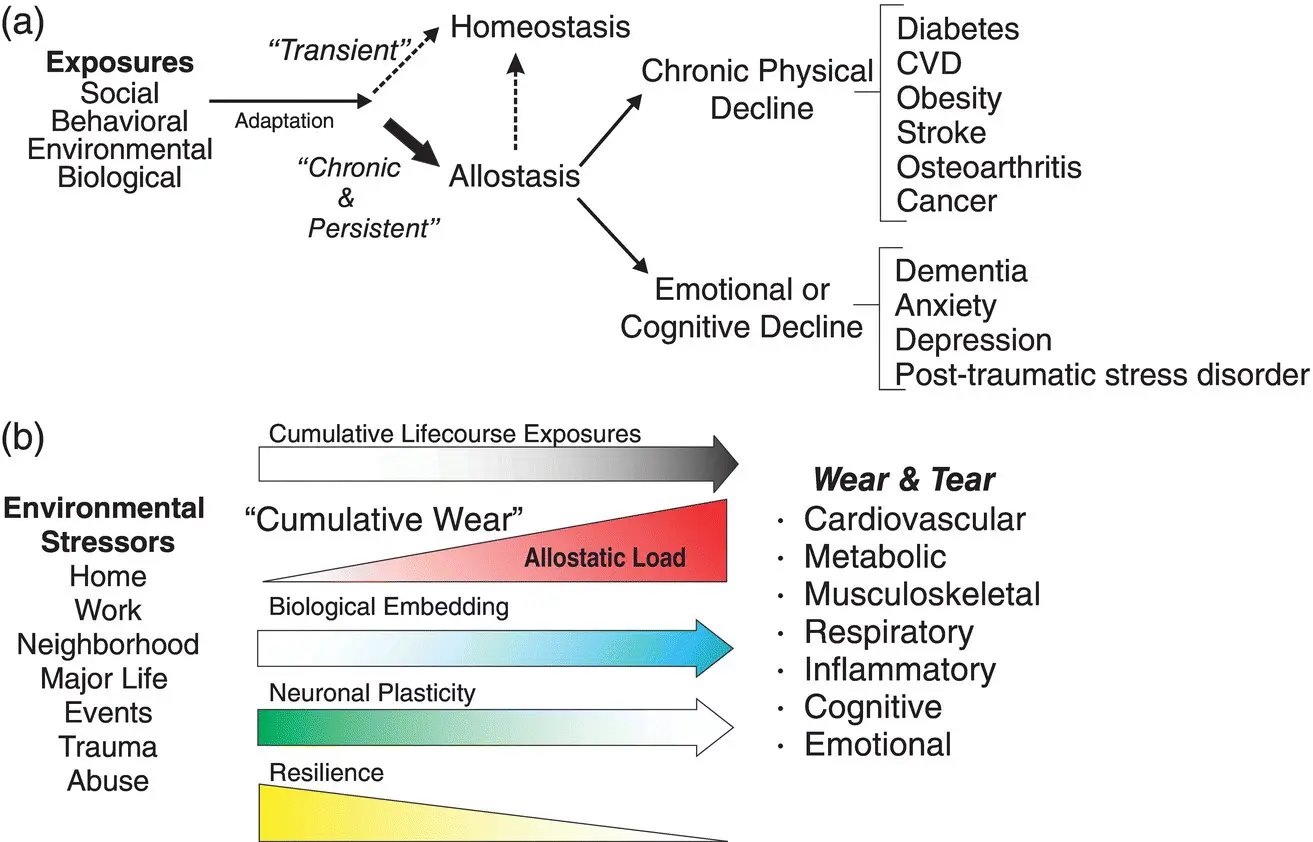
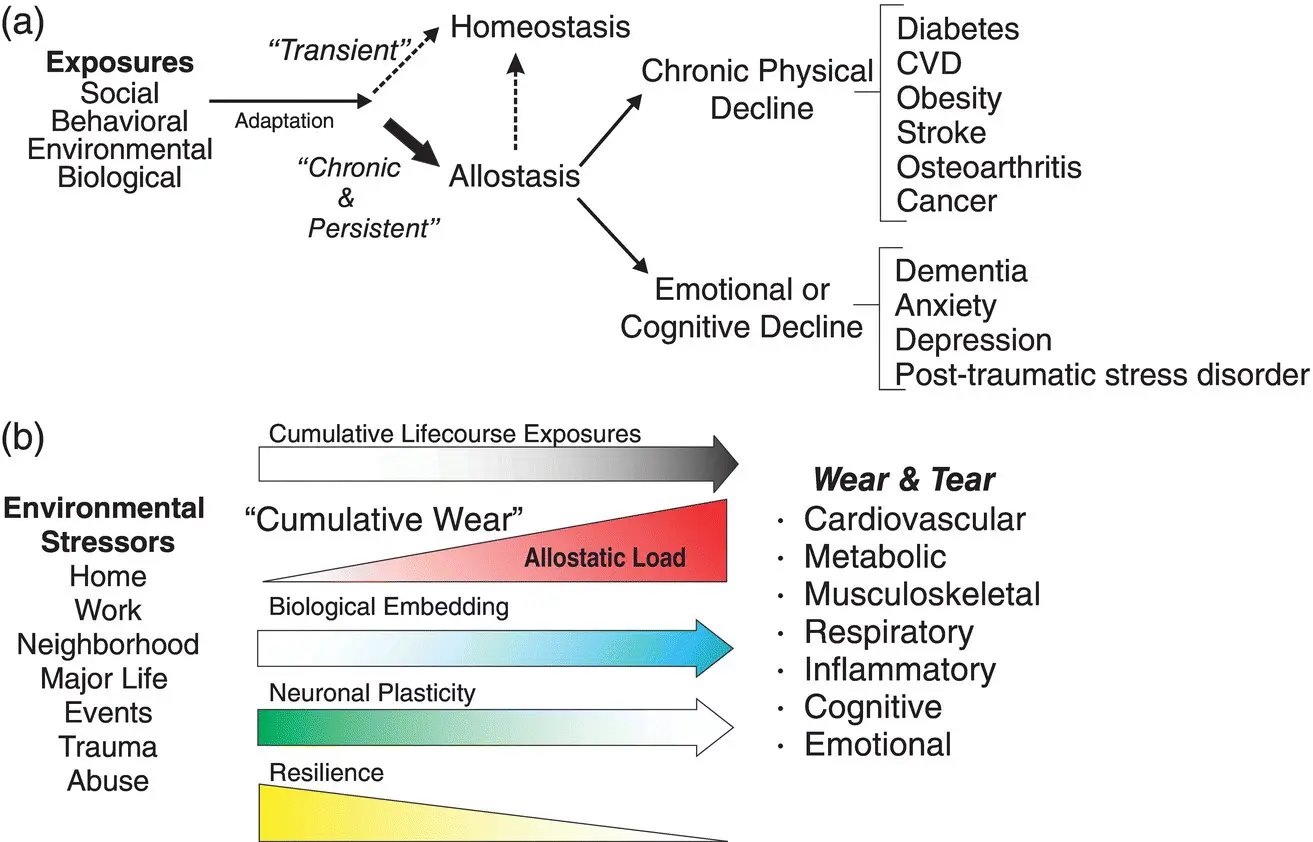
In this chapter, we discuss the pathways that influence how environmental, social, behavioral, and biological determinants independently and synergistically influence health disparities. We will begin by discussing the concept of allostatic load and how it provides a framework and perspective through which we can understand how environmental, social, behavioral, and biological determinants combine to influence health outcomes and potentially contribute to health disparities. By focusing on studies of social, racial, and ethnic differences in sleep, nutrition, and depression, we will provide examples from the literature that illustrate how such mechanisms converge to influence disparities in health outcomes.
2.2 Allostasis and Allostatic Load
One of the most significant universal biological imperatives is the maintenance of homeostasis. From the Greek homeo , meaning “similar” and stasis , meaning “stand” or “state,” homeostasis refers to the body's ability to maintain internal stability. Humans and mammals have evolved numerous physiological systems to maintain homeostasis (e.g., body temperature, serum electrolytes, blood pressure, and pH). Similarly, from the Greek allo, meaning “other” or “variable,” allostasis refers to change or adaptation to maintain stability and preserve homeostasis, particularly in response to environmental challenges ( Figure 2.1a). Allostasis, as initially coined by Sterling and Eyer [2] and popularized by McEwen [3], defines the central role of the brain in stress responses through the neuroendocrine and autonomic nervous system. This system is referred to as the hypothalamic‐pituitary‐adrenal (HPA) axis and, along with elements of the brain governing behavioral and physiological changes in the cardiovascular, metabolic, and autonomic nervous system, is a central component of the global stress response system [4]. Traditionally referred to as the “fight or flight” response, many components of the HPA have adapted to environmental threats or change to promote survival ( Figure 2.1b) [5].
Читать дальше