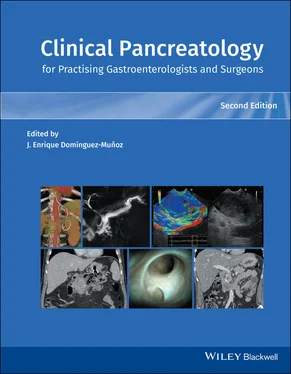
5 Role of CT Scan in Acute Pancreatitis : When is it Indicated and What Information can be Obtained?
Elham Afghani1,2, Mahya Faghih1, and Vikesh K. Singh1,2
1 Division of Gastroenterology
2 Pancreatitis Center, Johns Hopkins Medical Institutions, Baltimore, MD, USA
CT Imaging in Acute Pancreatitis
The routine use of CT imaging is not warranted as most cases of acute pancreatitis (AP) are mild and uncomplicated [1]. The primary role of imaging during the initial presentation of AP is to ascertain the diagnosis and detect pancreatic and/or extrapancreatic complications [1]. Contrast‐enhanced CT (CECT) is the gold standard for diagnosing AP. It has a sensitivity of 92% [2] and a specificity of up to 100% in detecting AP [3,4].
Contrast‐enhanced multidetector row CT (MDCT) is the gold standard for staging severity, assessing complications, and excluding other conditions that may mimic AP [1,5]. It provides high‐quality, multiphase imaging of the pancreas during a short breath‐hold. It can acquire volumetric information and has two‐ and three‐dimensional forms to deliver complex images. It also has dual phases including arterial and portal phases; intravenous contrast is given at a rate of 3 ml/s during the pancreatic and/or portal venous phase. MDCT has thin collimation and slice thickness [6]. If there is a concern for vascular complications, an additional arterial‐phase scan can be added to the protocol following a rapid intravenous bolus injection or contrast [7]. MDCT with perfusion imaging can be used to detect early pancreatic necrosis through ischemic changes [8]. However, perfusion is not widely available and it is not clear if it carries a true advantage over MDCT imaging. Monophasic contrast‐enhanced CT uses lower doses of radiation compared to dual‐phasic MDCT [7]. It is sufficient in most cases of AP, but one of its limitations is its inability to detect vascular complications.
Confirming the Diagnosis of AP
AP is diagnosed when patients present with two of the following: upper abdominal pain, amylase and/or lipase elevation more than three times the upper limit of normal, and/or imaging consistent with AP [1]. However, upper abdominal pain is not specific for AP and the diagnostic value of pancreatic enzyme elevation in AP is not clear. There are many intra‐abdominal conditions that can result in lipase and amylase elevations that may be misdiagnosed as AP, including inflammatory bowel disease, mesenteric ischemia, perforated peptic ulcer, dissecting aortic aneurysm, bowel obstruction, biliary colic, and acute appendicitis [9]. Therefore, imaging can help to exclude alternative causes of abdominal pain and can confirm the diagnosis of AP, particularly in those with a high suspicion of AP based on risk factors and clinical presentation.
Assessing the Etiology of Acute Pancreatitis
CT can assess for common bile duct (CBD) stones, which account for 40–70% of AP, although abdominal ultrasound and magnetic resonance cholangiopancreatography are the preferred methods of detection [5]. CT can evaluate for obstructive causes of AP including mass, cystic neoplasms, or pancreatolithiasis from chronic pancreatitis. Approximately 5–14% of patients with benign or malignant pancreatic masses may present with AP [4,10–12]. A pancreatic tumor may be seen as a focal area of high or low attenuation compared to the surrounding parenchyma. Other findings suggestive of a pancreatic neoplasm seen on CT imaging include an strictured or dilated pancreatic duct, deformed pancreatic contour, mass effect, arterial encasement, venous obstruction, dilated bile duct, metastasis, glandular atrophy of the distal parenchyma, and/or lymphadenopathy [13]. Other etiologies of AP that may be detected on CT include an intraluminal duodenal diverticulum. This should be suspected when CT reveals an enlarged duodenum, and a fluid density with a thin rim surrounded by hypodense tissue [14,15].
Assessing the Prognosis of Acute Pancreatitis
CT imaging has been included in several AP prognostic scoring systems. Table 5.1depicts the most common CT scoring systems. The earliest CT scoring system graded scans on an ordinal scale from A to E. Grades D and E correlated with clinically severe AP, with a corresponding mortality of 14% and morbidity of 54% compared with 2% morbidity and no mortality in grades A–C [16]. Studies have shown that the CT grading system has a sensitivity and specificity of 100% and 61.6%, respectively, for predicting morbidity, and 100% and 56.9%, respectively, for predicting mortality [17]. The strengths of the CT grading system are that it is easy to perform and does not require the use of intravenous contrast. However, limitations are that it does not significantly correlate with the development of organ failure, pancreatic and extrapancreatic necrosis, and peripancreatic vascular complications. Another limitation is that there is moderate interobserver agreement [3]. The CT Severity index (CTSI) is a scoring system that quantifies pancreatic and extrapancreatic inflammation and the extent of necrosis and thus helps distinguish between mild, moderate, and severe pancreatitis. A CTSI score of 0–3 correlates with mild AP, of 4–6 with moderate AP, and 7–10 with severe AP [16]. This has become the most widely used morphologic severity index for clinical and research purposes. Limitations of this scoring system is that it does not correlate with the development of organ failure, extrapancreatic parenchymal complications [18] and peripancreatic vascular complications [19]. Similar to the CT grading system, the CTSI is also limited by moderate interobserver agreement [20]. The modified CTSI (MCTSI) integrates extrapancreatic complications and extent of pancreatic necrosis (none, ≤30%, >30%) with the presence or absence of peripancreatic inflammation. MCTSI better correlates with patient outcome, length of stay, and development of organ failure and has similar interobserver agreement to the CTSI [21]. However, in a study with a larger number of patients with clinically severe AP, there were no significant differences between the two CT scoring systems [22]. Other scoring systems, such as pancreatic size index [23], MOP (“mesenteric oedema and peritoneal fluid”) score [24], retroperitoneal extension grade [25], and EPIC (“extrapancreatic inflammation on CT”) [26] have also been developed. However, these scores are not used in clinical settings. A large retrospective study comparing the accuracy of different CT scoring systems to clinical scoring systems found that CT scoring systems were not superior with regard to predicting mortality and persistent organ failure [27].
Table 5.1 CT prognostic scoring systems.
| CT grading system |
CT severity index |
Modified CT severity index |
| Grade |
CT findings |
Points |
Percentage necrosis |
Necrosis points |
Severity index |
Points |
Necrosis points |
Extrapancreatic complications a |
Severity index |
| A |
Normal pancreas |
0 |
0% |
0 |
0 |
0 |
0 |
0 |
0 |
| B |
Pancreatic enlargement |
1 |
0% |
0 |
1 |
2 |
0 |
0 |
2 |
| C |
Pancreatic inflammation and/or peripancreatic fat |
2 |
<30% |
2 |
4 |
2 |
2 |
0 |
4 |
| D |
Single peripancreatic fluid collection |
3 |
30–50% |
4 |
7 |
4 |
4 |
0 |
8 |
| E |
Two or more fluid collections and/or retroperitoneal air |
4 |
>50% |
6 |
10 |
4 |
4 |
2 |
10 |
aPleural effusions, ascites, vascular complications, parenchymal complications, gastrointestinal tract involvement.
Читать дальше