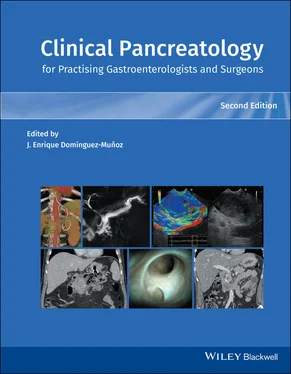
Pancreatic diseases represent an enigma to many physicians, even gastroenterologists and surgeons. Nevertheless, it encompasses a plethora of diseases that can severely affect the well‐being of any individual. Sound knowledge is therefore pivotal to provide clinical care for these patients. Pancreatologists have for long been pronounced an endangered species [1], triggering special efforts in postgraduate eductation [2].
It is the merit of the editor, J. Enrique Domínguez‐Muñoz, an esteemed and experienced gastroenterologist and pancreatologist who has left his mark in the field, to pull together an international group of highly recognized colleagues who themselves have made landmark contributions enlightening all of gastroenterology, pancreatology, and pancreatic surgery. One might ask whether in this day and age a textbook is needed. This book, the second edition of Clinical Pancreatology , proves that the answer to this is yes! In one physical place, everything related to the pancreas and its diseases, malfunction and affections, in conjunction with other aspects relevant to clinical practice, are covered. This book will provide reading for gastroenterologists, surgeons as well as fellows in pancreatology and anyone interested in pancreatic diseases. I trust that this second edition will be as well received and cherished as the first one.
J. ‐Matthias Löhr
Professor of Gastroenterology and HepatologyKarolinska InstitutetSecretary, European Pancreas Club (EPC)
1 1 Schmid R . Pancreatologists: an endangered species? Gastroenterology 2010; 138:1236.
2 2 Gasslander T, Holmberg B, Permert J. Pancreas 2000: a new concept for education and development in pancreatology. Pancreatology 2005; 5:545–546.
Since the book Clinical Pancreatology for Practising Gastroenterologists and Surgeons was first published 16 years ago, the knowledge and clinical management of pancreatic diseases have developed markedly. Thanks to the development of translational research and the “from bench to bedside” concept, much progress from the laboratory has been applied to clinical practice. In addition, several highly relevant clinical trials published over the last few years have resulted in the update and optimization of clinical guidelines.
A new and validated classification of severity and complications of acute pancreatitis is firmly rooted in clinical practice and has been the basis for the development of minimally invasive approaches to pancreatic necrosis. The etiopathogenic knowledge of chronic pancreatitis and other pancreatopathies, like that associated with diabetes mellitus, has developed significantly. Especially important has been the development of the field of cystic pancreatic tumors, which has been reflected in the publication of several guidelines and consensus reports over the last few years. Most research efforts have focused on pancreatic cancer, which have led and will further lead to a significant increase in the therapeutic armamentarium against this devastating disease. Finally, many newly published studies have changed the concept, causes, clinical relevance, diagnosis, and treatment of exocrine pancreatic insufficiency.
This new edition of Clinical Pancreatology for Practising Gastroenterologists and Surgeons has enjoyed the collaboration of the world’s leading experts in each of the areas of clinical pancreatology, with the aim of facilitating decision‐making by gastroenterologists, surgeons, oncologists, internists, nutritionists, diabetologists, pediatricians, radiologists, pathologists, and other specialists when facing patients with pancreatic diseases in their daily clinical practice. All in all, this book supplies an indispensable update of the relevant aspects of clinical pancreatology.
J. Enrique Domínguez‐Muñoz
To my wife, Beatriz, who still loves me despite my incurable tendency to keep working during my spare time on projects like this book.
To my father, who made me love Medicine.
To my mentors, Fernando Carballo and Peter Malfertheiner, who made me love the pancreas.
Section I Acute Pancreatitis
1 Acute Pancreatitis: An Overview
Jodie A. Barkin and Jamie S. Barkin
Department of Medicine, Division of Gastroenterology, Leonard M. Miller School of Medicine, University of Miami, Miami, FL, USA
Acute pancreatitis (AP) is a common problem worldwide. Its spectrum of disease varies from mild, so‐called interstitial acute pancreatitis, to severe necrotizing pancreatitis. Overall, its mortality rate is increased in patients older than age 65 years [1]. AP is among the most common gastroenterological causes of hospitalizations [2]. Roberts et al. [3] investigated regional and national patterns in the incidence and etiology of AP across Europe and found that the incidence of AP ranged from 4.6 to 100 per 100 000 population. Overall there was a median increase of 3.4% per annum over time and incidence was usually highest in eastern or northern Europe. Similarly, in the United States the rate of hospitalizations related to AP has increased from 2002 to 2013 [3,4] but overall mortality decreased [5]. In the 2012 Burden of Gastrointestinal Disease in the United States, AP was reported as the most common reason for hospitalization [6].
Table 1.1lists the causes of acute pancreatitis. However, biliary disease and alcohol are the two most common causes, together accounting for approximately two‐thirds of cases [7]. Biliary diseases include cholelithiasis, choledocholithiasis, microlithiasis (stones <5 mm), and biliary sludge, and are likely the most common cause of AP. Microlithiasis is more frequently detected by endoscopic ultrasound (EUS) than by transabdominal ultrasound [8]. It is also the most common diagnosis by EUS in patients with idiopathic AP [9].
Biliary causes should be evaluated in all patients who present with AP. The initial test is surface ultrasonography, which allows excellent visualization of the gallbladder but limited views of the common bile duct and pancreas, especially in obese patients and those with ileus.
Cholelithiasis is felt to be the most common cause of AP. Our goal is to determine its presence with the least mortality. The role of endoscopic retrograde cholangiopancreatography (ERCP) has changed from a diagnostic to a therapeutic modality for two reasons: first, because of its associated morbidity (4–7%) and mortality (0.06–0.33%) (although these figures include therapeutic and not simply diagnostic ERCP) [10,11]; and second because of the development and widespread availability of magnetic resonance cholangiopancreatography (MRCP) and EUS as diagnostic modalities. In patients with AP, the primary role of early ERCP (<48 hours) is in patients with acute cholangitis, where ERCP with endoscopic sphincterotomy (ES) reduces mortality and systemic and local adverse events [12].
In patients with AP and suspected biliary obstruction that is manifested by a dilated common bile duct and elevated liver function tests, MRCP or EUS is used to confirm these findings and establish a diagnosis [12]. EUS or MRCP has comparable accuracy to diagnostic ERCP and therefore a negative study obviates the need for ERCP. A systematic review of randomized controlled trials and clinical trials by De Lisi et al. [13] found that EUS had a lower failure rate than ERCP and that ERCP was avoided in 71% of patients. In the patient with suspected biliary AP and negative surface ultrasound, the question is whether MRCP or EUS should be utilized. The advantage of MRCP is that no contrast agent, anesthesia, or radiation is required. In a study by Makary et al. [14], magnetic resonance cholangiography accurately identified 57 of 62 (94%) of patients with gallstones and correctly identified choledocholithiasis in 94%. In a meta‐analysis, Wan et al. [15] compared EUS with MRCP in patients with idiopathic AP and found a diagnostic yield of 64% for EUS and 34% for MRCP.
Читать дальше