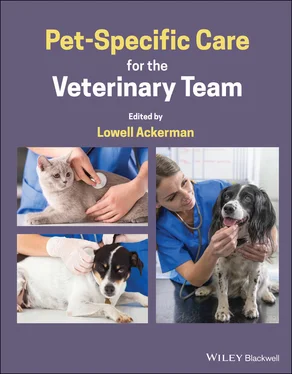
3 Nonsteroidal antiinflammatory drugs (NSAIDs).
4 Local and locoregional anesthetics and techniques – the “missing ingredient” for many if not most surgical procedures in small animal medicine (but not in large animal or in human medicine); nevertheless industry guidelines stipulate that local anesthetics should be utilized with every surgical procedure (even if just an incisional block but there are dozens of local and locoregional techniques within the scope of any veterinarian – and veterinary technician – to master).
5 Adjunctive pain‐modifying medications and modalities: these are deployed with patients undergoing predictably more painful procedures and/or are at higher risk for maladaptive pain, e.g. those with nerve injury, severe trauma (preexisting or surgical, soft tissue or orthopedic), or with long‐standing previous pain and inflammation. These include but are not limited to constant‐rate infusions of ketamine, systemic lidocaine, dexmedetomidine, oral gabapentin, amantadine, and others.
6 Nonpharmacological interventions such as cold compression, physical rehabilitation, possibly acupuncture, and energy‐based modalities such as therapeutic laser, pulsed electromagnetic field, and others.
There are a variety of options for managing the chronic pain of OA (see also 8.20 Team Strategies for Arthritis).
Weight optimization
Antiinflammatory agents (NSAIDs and prostaglandin receptor antagonists, PRA)
Eicosapentaenoic acid‐rich (dog), docosahexaenoic acid‐rich (cats) diets
Therapeutic exercise
Polysulfated glycosaminoglycan and nutritional supplements
Adjunctive pain‐modifying medications (e.g., gabapentin, amantadine)
Intraarticular (IA) agents such as biologics (stem cells, platelet‐rich plasma) and others
Anti‐nerve growth factor (NGF) monoclonal antibody (mAb)
2.16.3.3 Non‐OA Chronic Pain
Neoplastic pain, especially osteosarcoma (OSA) and any tumor metastasizing to bone, is generally considered to include a neuropathic component facilitated in part by osteoclastic activity. In palliative care circumstances (e.g., limb‐sparing OSA), multiple modalities should be deployed since undercontrolled pain will predicate the decision for humane euthanasia. As cyclooxygenase (COX) enzymes are greatly upregulated in OSA, NSAIDs are appropriate medications to deploy, along with one (or more) adjunctive pain‐modifying oral medications (among the higher effectiveness:safety ratios in human cancer‐related pain are anticonvulsants like gabapentin). Oral acetaminophen and opioids are frequently deployed in humans with chronic cancer pain, and can be utilized judiciously in dogs (not cats), but the bioavailability and clinic impact of these drugs have been questioned. Long‐acting (days, not weeks) parenteral opioid medications are available for off‐label use in dogs and cats. Uniquely in cancer pain, bisphosphonate (pamidronate, zolendronate) infusions freeze osteoclast activity and can elicit durable (approximately one month) improvement in a majority of dogs [6].
Nonneoplastic maladaptive and/or neuropathic pain syndromes described in dogs and cats often have an identifiable cause, but not always; it may be associated with identifiable inflammation, but not always. If an underlying condition is identifiable, it should be managed accordingly. To treat pain directly, if there is a grossly inflammatory component to the condition then antiinflammatory agents (NSAIDs or, when indicated, corticosteroids) can and should be utilized. But if there is no gross inflammation then antiinflammatory agents are unlikely to be beneficial, and one would gravitate to those medications and modalities which address hypersensitization leading to maladaptive and neuropathic pain. Chief among these would be gabapentinoids and possibly amitriptyline, amantadine, serotonin and norepinephrine reuptake inhibitors (e.g., venlafaxine) among others (clinical data limited).
2.16.4 Confounders of Pain
There are a variety of other situations that can complicate the assessment and management of pain in animals.
Age: young, still‐growing patients have enormous “plasticity” in their CNS, and early painful experiences can elicit permanent alterations embedded in the CNS and can manifest as increased pain sensitivity later in life. Older patients are often beset by chronic inflammatory processes (OA, gingivitis, otitis, dermatitis) which can elicit a neuropathic component, and whose spinal cord is a “smoldering ember” of hypersensitization upon which a subsequent acutely painful event can cause greatly exaggerated pain.
Obesity: adipose tissue is the body's largest endocrine organ and secretes a witch’s brew of proinflammatory cytokines and mediators that circulate systemically and sensitize nociceptors. In humans, excess abdominal fat will double the risk for a chronic pain condition later in life [7].
 EXAMPLES
EXAMPLES
Example 1 : Ovariohysterectomy (OHE) in a 5‐month‐old mixed‐breed dog. Client administers trazodone at home prior to transport to hospital. Patient admitted with fear‐free and low‐stress handling techniques, premedicated with buprenorphine, midazolam intramuscularly (IM), and NSAID of choice orally (PO). Induction of anesthesia, placed on intravenous (IV) fluids, incisional block with bupivacaine. OHE proceeds with lidocaine mesovarium block. Patient discharged with three days of NSAID.
Example 2 : Comminuted femoral fracture resulting in hindlimb amputation of 7‐year‐old cat. Client administers gabapentin and NSAID at home prior to transport to hospital. Patient admitted with fear‐free and low‐stress handling techniques, premedicated with combination of buprenorphine, dexmedetomidine, and ketamine IM. Induction of anesthesia, placed on IV fluids with ketamine constant rate infusion (CRI), epidural with bupivacaine via lumbosacral or sacral‐coccygeal approach. Post‐op administered long‐acting buprenorphine and discharged with NSAID and gabapentin PO.
Example 3 : Cruciate repair surgery in a 6‐year‐old lab mix. Client administers NSAID and high‐dose gabapentin at home prior to transport to hospital. Patient admitted with fear‐free and low‐stress handling techniques, premedicated with hydromorphone and midazolam IM. Induction of anesthesia includes loading dose of ketamine IV, placed on IV fluids with ketamine CRI. Femoral and sciatic regional nerve block performed with bupivacaine, and IA hydromorphone. Patient prepped and surgery performed. Long‐acting (liposome‐encapsulated) bupivacaine infused into several layers of closure. Post‐op cold compression, continue ketamine ± opioid CRI for 4–6 hours. Patient discharged with NSAID, gabapentin PO, and physical rehabilitation instructions (or referral), to include therapeutic laser if available.
Example 4 : 12‐year‐old golden retriever with a BCS of 7/9 stiff in the mornings and after exercise; owner has to help up onto the couch. Physical exam reveals straight‐legged conformation and atrophy rear quarters, discomfort, physical examination, and radiographic signs consistent with hip dysplasia and advancing OA. Priority is to place patient on NSAID or PRA of choice and switched to an EPA‐rich diet formulation that also promotes weight loss to BCS of 6 and ultimately a lean 5. If owners agreeable, patient is also placed on polysulfated glycosaminoglycan, or alternatively, a high‐quality and reputable nutraceutical; exercise program implemented that includes vigorous walks and inclines but unrestricted activity is limited. If and when eventually deemed appropriate and available, choice (and/or combination of) pain‐modifying analgesic medication (e.g., amantadine, gabapentin) is prescribed as adjunct to the NSAID or PRA, IA biologic injections, and anti‐NGF mAb treatments are implemented. Acupuncture, therapeutic laser, pulsed electromagnetic field, myofascial trigger point, referral for aggressive physical rehabilitation, and other nonpharmacological modalities can be utilized at any time.
Читать дальше
 EXAMPLES
EXAMPLES