1 ...6 7 8 10 11 12 ...17 Periodontitis in relation to systemic diseases
Diabetes mellitus
Diabetes mellitus is a metabolic condition with chronic hyperglycemia as the leading symptom. Both diabetes mellitus and periodontitis are chronic, inflammation-driven diseases with mutual influence regarding their impaired immunologic responses. 63,64
Diabetes mellitus as well as periodontitis are common, chronic, noncommunicable diseases that exhibit a bidirectional relationship (review 65). The relationship between both diseases was first described by Löe in 1993, and periodontitis found as the sixth complication of diabetes mellitus. 66It has been shown that patients with diabetes mellitus exhibit more severe and rapidly progressive forms of periodontitis compared to patients without diabetes mellitus. 67-70It is now widely accepted that diabetes mellitus represents a major risk factor for the development and progression of periodontitis, and thus, diabetes mellitus has now been added as a modifying factor within the grading of periodontitis. 29,33
Furthermore, during severe periodontitis, the inflammatory process can have detrimental effects on blood sugar control by influencing the insulin resistance, leading to a poorer glycemic control, increasing the rate of incident prediabetes and type 2 diabetes mellitus. 71-74Here, the periodontal inflammation exhibits a systemic impact along with bacteremia and increased levels of pro-inflammatory mediators detectable in the blood stream, and therewith, blood sugar control and insulin resistance are negatively influenced in patients with periodontitis and diabetes mellitus. 65,70,75-77
Diabetes mellitus-related complications, such as cardiovascular, cerebrovascular, renal, retinal, and neuropathic complications, are significantly increased in patients with severe periodontitis and type 2 diabetes mellitus. 78-82
Cardiovascular diseases
Cardiovascular diseases also belong to the group of chronic noncommunicable diseases, and it has been shown that there is a clear epidemiologic association with periodontitis. 83,84More precisely, epidemiologic studies have demonstrated that there is a positive association between periodontitis and coronary heart and cerebrovascular disease. 84,85
Similar to diabetes mellitus, one of the proposed mechanisms of interaction includes the incidence of bacteremia due to daily routine procedures such as tooth brushing or eating. 25It was found that the magnitude of bacteremia was higher in patients with periodontitis when compared to patients with gingivitis. 26Analyses of atherothrombotic tissues revealed the presence of periodontal bacteria, and patients with periodontitis showed a greater probability for the detection of periodontal pathogenic bacteria in those tissues. 86,87
In this context, the influence of periodontitis on the systemic inflammatory status has been recognized as an important mechanism. 75,76When compared to healthy control individuals, patients with periodontitis exhibited elevated levels for C-reactive protein (CRP), interleukin-(IL)-1 beta, IL-6, IL-8, and tumor necrosis factor alpha (TNF-α). 88-96
Dyslipidemia is recognized as a risk factor for cardiovascular diseases, and it has been shown that dyslipidemia is present in patients with periodontitis. 97,98Other parameters, such as increased intima media-thickness or alterations in the flow-mediated dilatation of blood vessels, may indicate pathologic cardiovascular alterations. Periodontitis is associated with an increased intima media-thickness, changes in the flow-mediated dilatation, and hypertension. 99-103
It is an interesting finding that both periodontitis and cardiovascular diseases seem to share common genetic risk factors. 58,59,104This functional and molecular background is the subject of current research projects. 62
Rheumatoid arthritis
Rheumatoid arthritis is a complex autoimmune disease that is characterized by the infiltration of macrophages and T-cells into the synovial membrane of joints leading to cartilage degradation and bone erosion. 105The production of auto-antibodies is typical for rheumatoid arthritis, and the auto-antibody against immune globulin G represents the rheumatoid factor. 106,107Biochemical post-translational processes, such as citrullination and carbamylation, are involved in the mechanisms leading to antibody synthesis. 108,109Citrullination is a post-translational modification of the amino acid arginine to citrulline promoted by an enzyme called peptidylarginine deiminase (PAD). Based on the current knowledge, the link between rheumatoid arthritis and periodontitis could be via the periodontal pathogen P gingivalis , which also expresses a similar enzyme (PPAD). 110The proteins modified by the PPAD from P gingivalis can further promote autoantibody production against citrullinated proteins (anti-citrullinated protein antibodies [ACPAs]), and this may be another stimulus for the development of rheumatoid arthritis. 108,110Current research investigates the hypothesis of periodontitis to be a risk factor for rheumatoid arthritis. 111,112
Periodontitis may exhibit a considerable influence on systemic conditions such as diabetes mellitus, cardiovascular disease, and rheumatoid arthritis.
Clinical features and diagnosis
Symptoms, clinical and radiographic features
Periodontitis represents major clinical characteristics including microbial biofilm formation (dental plaque biofilm), inflammation of the gingiva, periodontal attachment loss, and bone loss. The microbial biofilm is visible as dental plaque on tooth surfaces and around the gingival margin, which may calcify and form dental calculus when not routinely removed by daily oral hygiene procedures. In most patients, the amount of plaque formation and calculus is associated with severity of periodontitis. Inflammation of the gingiva around the teeth can be seen by swelling, redness, edema, and bleeding. Pocket formation, bleeding on probing, and gingival recessions combined with periodontal attachment and bone loss are clinical signs of periodontitis. Furthermore, patients with severe periodontitis often suffer from tooth migration, increased tooth mobility, and periodontal abscesses. Clinical periodontal examination comprises the measurements of attachment level, periodontal pocket probing, bleeding on probing, furcation involvement, and tooth mobility. The amount and the type of bone loss (horizontally versus vertically), furcation involvement, and combined periodontal-endodontic lesions are determined by additional radiographic examinations. Figures 2-2 to 2-11 display the periodontal screening index, different types of periodontal explorers, and a complete patient case documentation during active periodontal therapy, and further background information is given in the corresponding legends.
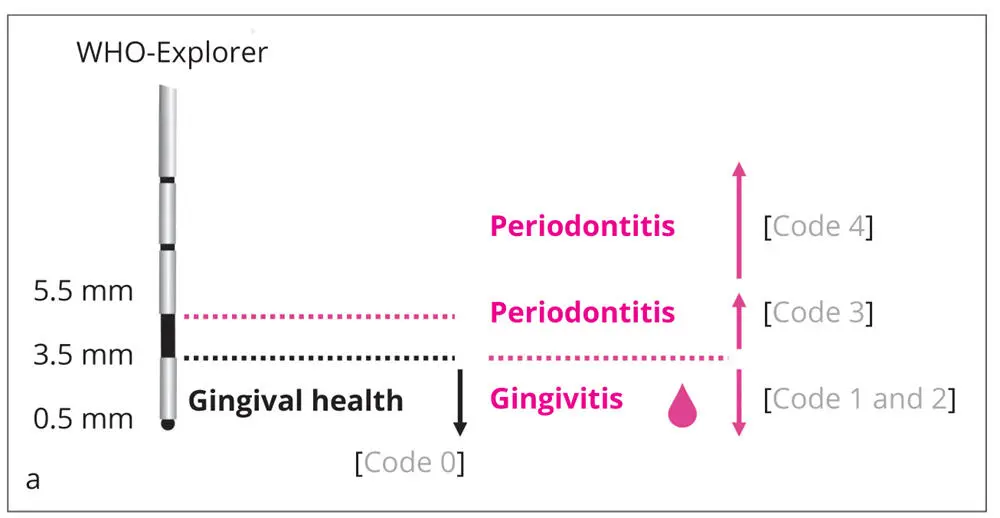
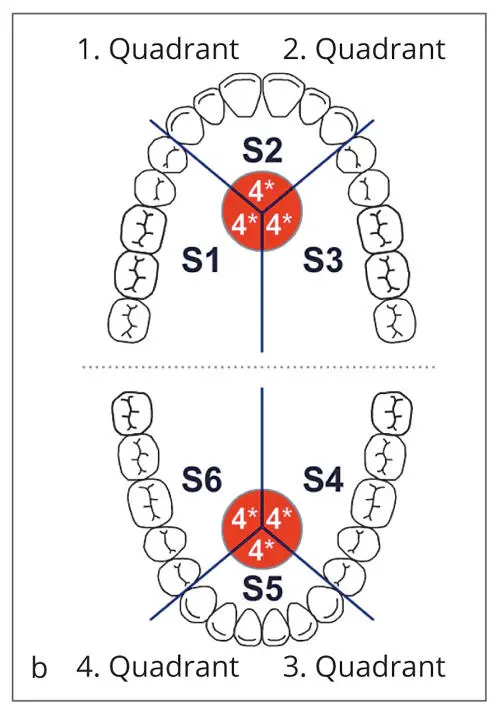
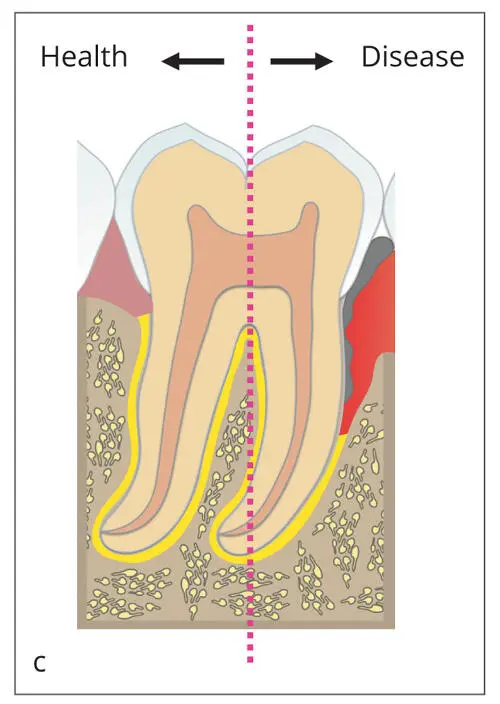
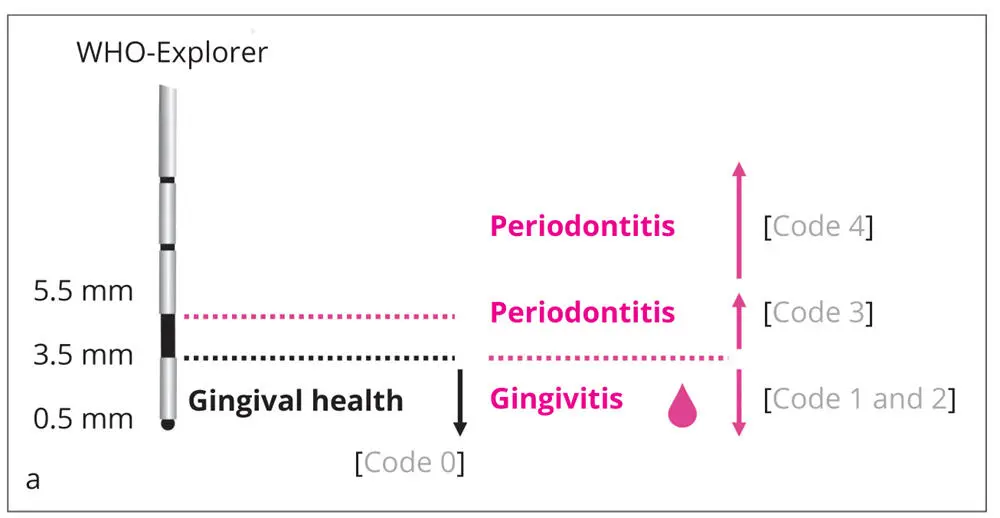
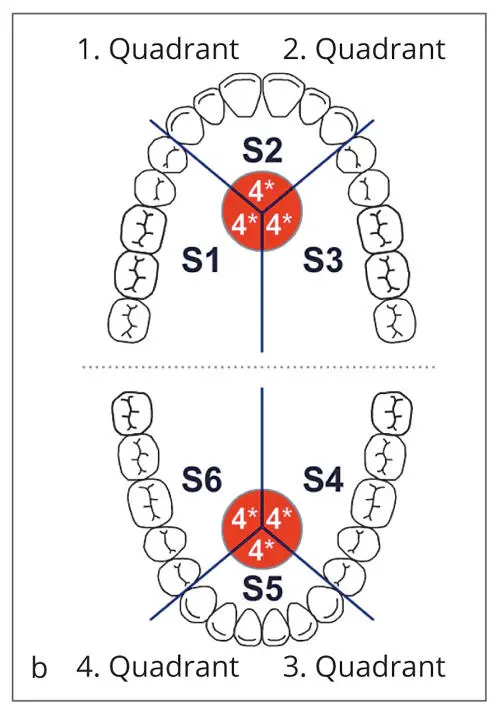
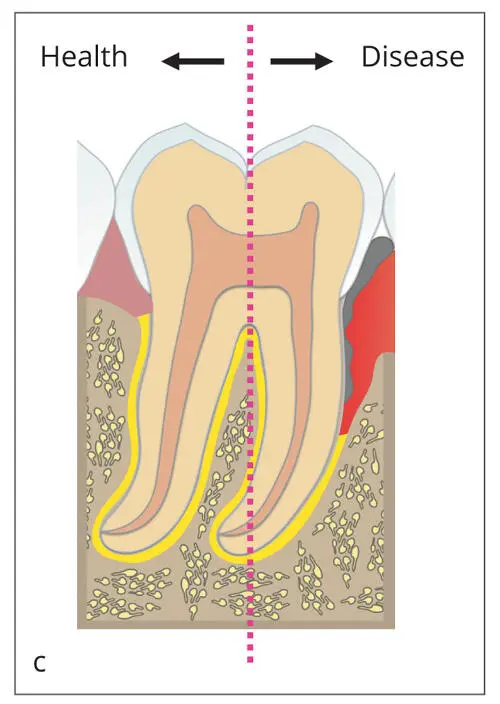
Figs 2-2a to cPeriodontal Screening Index (PSI). (a) Periodontal conditions are explored by a periodontal probe proposed by the World Health Organization (WHO). This probe is graded in sections of 0.5 mm, 3.5 mm, and 5.5 mm, respectively. Depending on the depth of penetration, different codes refer to the indication of health or disease. Shallow pockets (< 3.5 mm) without bleeding upon probing are considered healthy (code 0) and with bleeding on probing indicate gingivitis (code 1 and code 2 when calculus and/or overhanging restoration margins are present), whereas pockets > 3.5 mm to 5.5 mm indicate moderate, and ≥ 5.5 mm indicate more severe periodontal destruction (when no pseudopocket is present). (b) These codes are charged to each of the six quadrants; * indicates special findings, such as recessions, furcation involvement, tooth mobility, and migration. (c) The PSI allows a quick and safe examination of periodontal condition in the dentition. It helps to clearly distinguish between health and more or less severe disease without claiming a distinct periodontal diagnosis.
Читать дальше