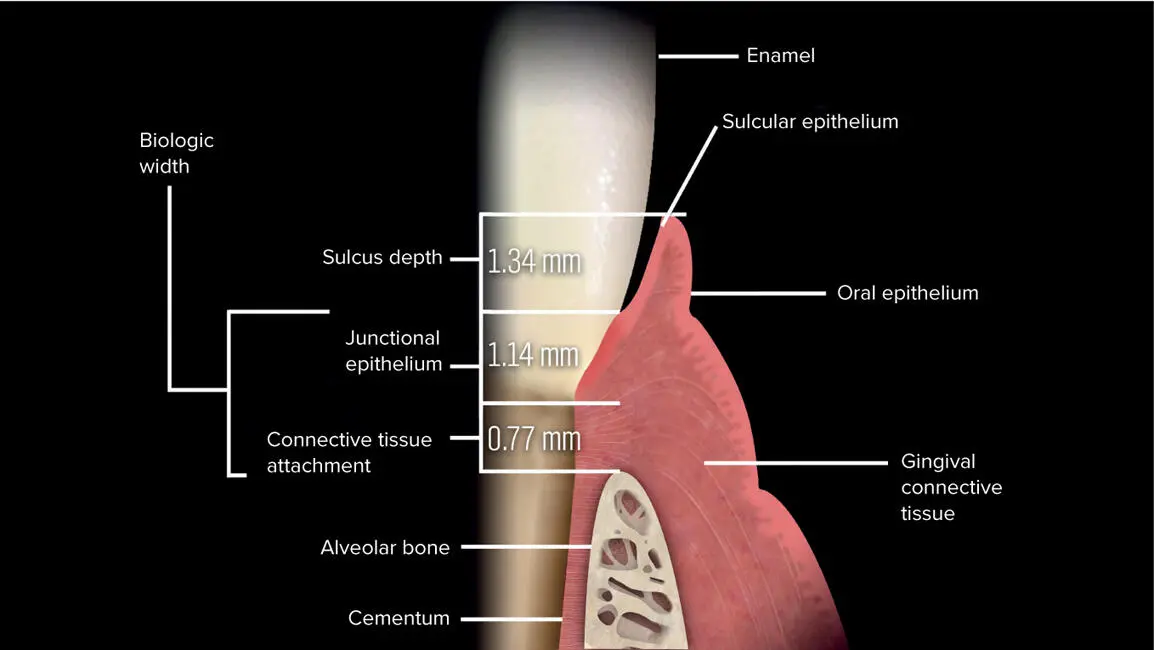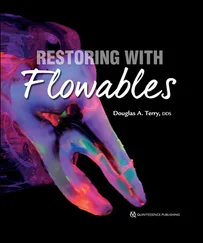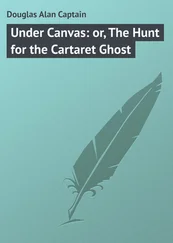
Fig 1-17 The biologic width is used as a guideline during the evaluation of periodontal-restorative interrelationships and is described as the physiologic dimension of junctional epithelium and connective tissue attachment to the root above the alveolar crest. (Illustration copyright by Nicolas Elian, DDS.)



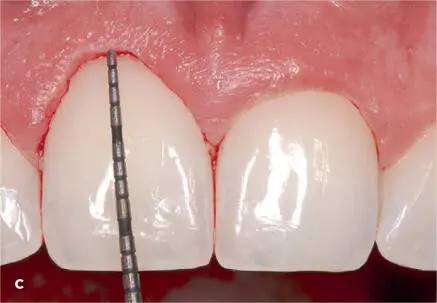
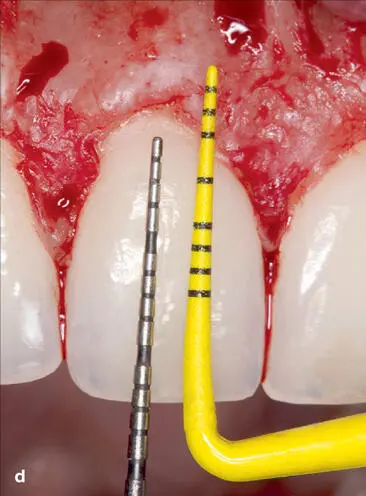
Fig 1-18 (a to c) After the patient is anesthetized, the sulcular depth and the dimension to the osseous crest are measured and recorded, and the difference between these two measurements is the biologic width.
Clinical observation indicates that impingement of the biologic width will result in attempts by the gingival tissue to reestablish its original dimension through bone resorption or, in the presence of a thick alveolar crest, chronic gingival inflammation159 ,196 ,586 ,588 –590 ( Fig 1-19). This physiologic dimension of supracrestal apparatus should not be violated by restorative procedures196 ,572 ,591 –594 and should be measured prior to initiating restorative treatment. The preservation of the biologic width is crucial for long-term success of the restoration. Thus, to attain an adequate ferrule dimension of 1.5 to 2 mm and maintain a biologic width of 3 mm requires a restorative dimension of 4.5 to 5 mm of supracrestal tooth structure. In those clinical scenarios where there is insufficient ferrule length and the potential for infringement on the biologic width, there are several treatment alternatives to achieve this restorative dimension, including surgical crown lengthening ( Fig 1-20) and/or orthodontic extrusion. 81 ,159 ,206 ,301 ,327 ,400 ,531 ,541 ,545 ,585 ,587 ,591 ,595 –608
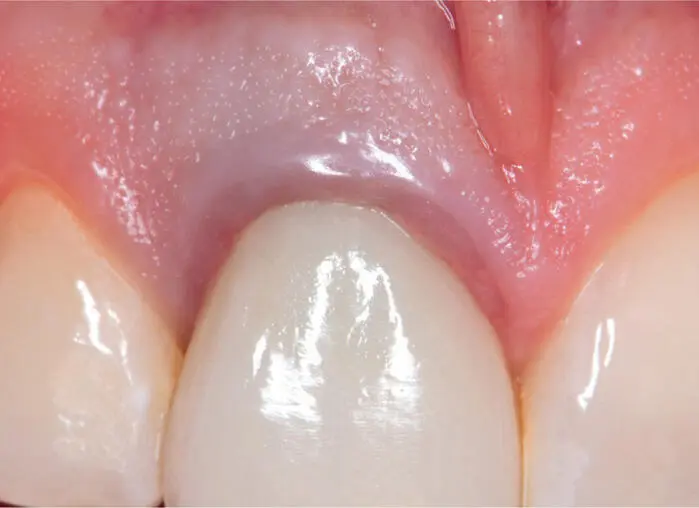
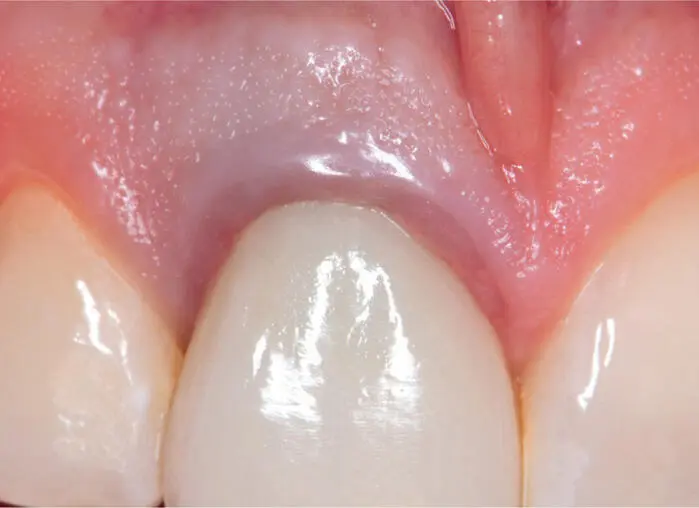
Fig 1-19 The restorative margin of the metal-ceramic crown is infringing on the biologic width. The consequences of placing the restorative margin into the (supracrestal apparatus) coronal attachment of the periodontal connective tissue can result in periodontal sequelae such as gingivitis, loss of clinical attachment, infrabony pocket formation, gingival recession, and bone loss.




Fig 1-20 (a to d) Crown lengthening was performed on the maxillary anterior central and lateral incisors to provide an adequate ferrule dimension, biologic width space, and an optimal gingival architecture. (Dentistry courtesy of Gamid Nasuev, DDS, PhD.)
METHODS FOR ESTABLISHING AN OPTIMAL FERRULE EFFECT
Periodontal crown lengthening
Crown lengthening procedures have been traditionally performed to provide access for treatment of subgingival caries, fractures, replacing defective restorations, and establishing an optimal restorative dimension. Crown lengthening is also recommended when there is inadequate tooth structure for crown retention as a result of excessive occlusal wear, abrasion, altered passive eruption, hyperplastic tissue, or asymmetric gingival margins. Furthermore, this procedure may be required for the treatment of chronic gingivitis caused by the placement of an otherwise satisfactory restoration exhibiting margins that impinge on the biologic width.196 ,588 ,589 ,609 Its surgical objectives include the exposure of an area of sound tooth structure suitable for placement of a restorative margin while providing adequate biologic width space.196 ,579 ,610 –612 This surgical procedure entails altering gingival and osseous levels through osseous contouring and/or gingivectomy196 ( Figs 1-21to 1-23). Consideration factors prior to performing this procedure include the taper of the root, the crown-to-root ratio, and the location of any furcation.159 This procedure requires minimal chair time for the patient; however, it usually requires crestal bone to be removed to establish this restorative dimension of 4.5 to 5 mm of supracrestal sound tooth structure. This procedure can result in an unfavorable crown-to-root ratio, larger interdental spaces (ie, black triangles), decrease in the cross section of the preparation, and an improper emergence profile that can result in esthetic compromises.327 ,545 Therefore, this procedure should be used in the posterior region where there are fewer negative effects on esthetics.606 Furthermore, in regard to length of time for maturation of tissue following the surgical procedure and the stability of the postoperative position of the gingival margin, there are various recommendations for the time between surgical procedure and final preparation and impression taking, ranging from 6 months to 1 year.579 ,587 ,613


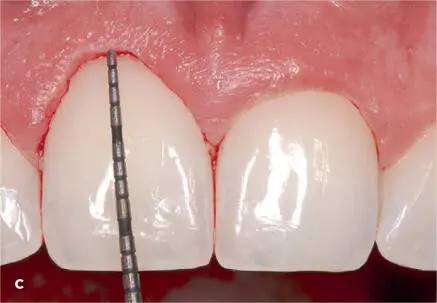
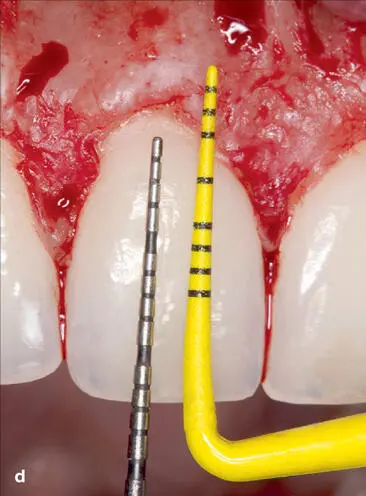

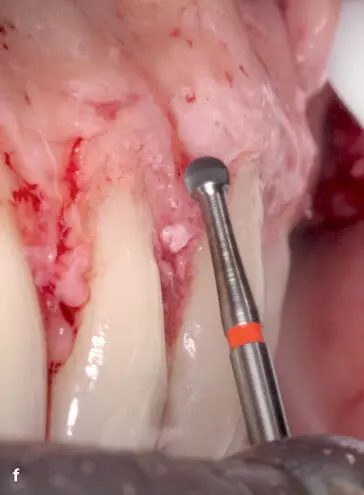



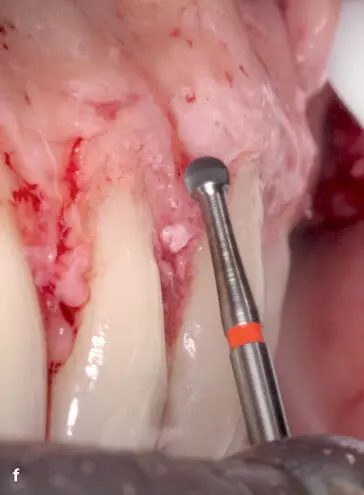
Fig 1-21 The following clinical presentation provides an illustration of the conventional approach of crown lengthening, which requires gingivectomy and resective osseous surgery to provide the 3-mm dimension of exposed tooth structure supracrestally. (a) The patient presented with excess gingival display and deficient anterior tooth proportions, requiring altering of the gingival margin-to-tooth relationship. (b and c) A gingivectomy was performed to the predetermined new gingival height and contour. (d) Afterward, a split-thickness flap was performed in the region with a full-thickness flap to reveal the osseous crest at the cementoenamel junction. The periodontal probe indicates the amount of osseous tissue to be resected to accommodate the biologic width and crevicular space. (e) An end-cutting surgical bur was initially used to perform the ostectomy and to develop an ideal parabolic form. (f) To enhance the appearance of the gingiva in the middle third, an osteoplasty was performed using a no. 6 surgical round bur to resect and contour the osseous architecture. (g) It is important to inspect for irregular steps at the interface of the bone and the root structure and smooth them to a 45-degree angle. (h) An improved coronal length of the maxillary anterior teeth with a 3-mm scallop was achieved. (i) Clinical appearance 6 months later. By altering the gingival and osseous levels through gingivectomy and osseous contouring, an increased dimension of tooth structure can be obtained while providing adequate biologic width space. (Surgery courtesy of Wesam Salha, DDS, MSD.)
Читать дальше