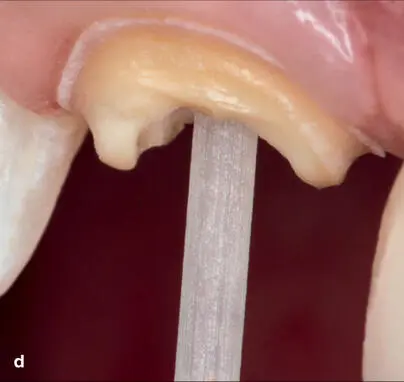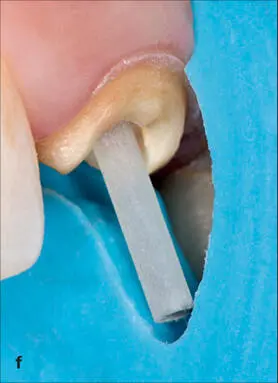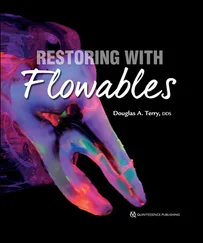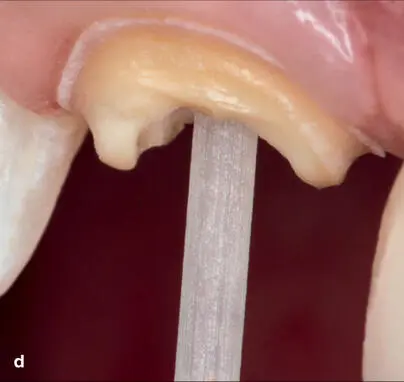

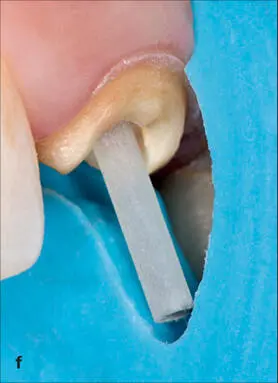


Fig 1-16 (a to h) Developing a ferrule effect. Dislodgment and tooth fracture are causes for failure of post and core restorations. Core stability and post retention are important in preventing these failures in the restoration of ETT. The ideal post system should replace lost tooth structure while providing adequate retention and support to the core, allowing retention of the restoration while transferring occlusal forces during function and parafunction to prevent root fracture. The completed crown preparation should have a ferrule design that encapsulates the endodontically restored tooth complex. This collar effect provides an antirotational feature for the stability of the crown. The general guideline is a 1- to 2-mm preparation on sound tooth structure. Procedures that provide a shoulder on tooth structure and an axial preparation that covers only the core buildup will have an insufficient ferrule design. In cases where there is insufficient sound tooth structure for this ferrule design, it is necessary to obtain this dimension through periodontal crown lengthening and/or forced tooth eruption procedures.
Studies indicate that a minimum of 1 to 2 mm of remaining tooth structure coronal to the preparation finish line is required to establish an adequate ferrule.541 ,554 ,559 Other studies indicate that a ferrule height of 2 mm of vertical sound tooth structure provides the most favorable resistance to tooth fracture and the most optimal stress distributions,560 thus decreasing the weakening effect of a post system.551 Numerous studies have indicated that a uniform ferrule provides a significantly greater resistance to fracture than a nonuniform ferrule.551 ,552 ,561 However, it has been suggested that a partial ferrule is a better alternative than the absence of any ferrule,301 although a circumferential coronal structure extending 1.5 to 2 mm from the margin of the crown has an improved prognosis.301 One study concluded that the clinical success of endodontically treated premolars was improved when a ferrule of at least 2 mm was present.562 Also, in vitro and clinical studies have demonstrated that allowing 2 mm of coronal tissue to remain around the entire circumference of the endodontically treated tooth will provide resistance so that the design of the post and material are irrelevant. 47 ,216 ,361 ,529 ,541 ,563 –565
Dislodgment and tooth fracture are causes for failure of post and core restorations. A finite element analysis of ferrule design confirmed that a ferrule increases the mechanical resistance of a post-core-crown restorative complex by reducing the potential for displacement.547 A restoration without a ferrule is susceptible to failure from debonding and subsequently by root fracture through the lever action motion of the unstable debonded post.547 Core stability and post retention are important in preventing these failures in the restoration of ETT. The stability of the crown is influenced by the preparation design. This collar effect provides an antirotational feature for the stability of the crown. The ideal treatment should replace lost tooth structure while providing adequate retention and support to the core, allowing retention of the restoration while transferring occlusal forces during function and parafunction to prevent root fracture. Root fractures are prevalent in ETT without an adequate ferrule effect. 19 ,566 A direct correlation has been reported between the amount of existing sound coronal tooth structure and the capacity of the tooth to resist occlusal forces.387 ,567 –569 The author’s general guideline is a 1- to 2-mm preparation on sound tooth structure. Procedures that provide a shoulder on tooth structure and an axial preparation on the core buildup will have an insufficient ferrule design and will compromise the ferrule effect.327 Therefore, it has been suggested that although the ferrule is recommended and desirable, it should not be provided at the detriment of the remaining tooth and/or root structure. 19In cases where there is insufficient sound coronal tooth structure for this ferrule design, it is necessary to obtain this dimension through periodontal crown lengthening and/or forced tooth eruption procedures for optimal clinical results. If these are not considered to be treatment options after informing the patient, a post and core with crown or an extraction with an implant-supported crown or a fixed (conventional or adhesive bridge) or removable prosthesis are considered the alternatives.327
CLINICAL CONSIDERATIONS FOR DETERMINING AN INADEQUATE FERRULE EFFECT
Subgingival fractures and root caries present periodontal and restorative challenges for the restorative team. Because minimal supragingival tooth structure can compromise the attainment of a ferrule design, the restorative team should initiate periodontal evaluation to determine the restorability of the fractured tooth prior to endodontic and restorative rehabilitation. One significant consideration in establishing the ferrule design is the influence of the biologic width. The biologic width or supracrestal tissue is described as the physiologic dimension of junctional epithelium and connective tissue attachment to the root above the alveolar crest570 ( Fig 1-17). It is measured from the coronal part of the junctional epithelium to the crest of alveolar bone.571 ,572 Biologic width dimensions have been traditionally based on the work of Gargiulo et al,573 who reported average values for epithelial and connective tissue attachment to be 0.97 mm and 1.07 mm, respectively, yielding a combined measurement of 2.04 mm. Although these dimensions are ubiquitously quoted in the literature, recent data published by Vacek et al574 suggest that supracrestal gingival tissue dimensions as well as the mean gingival sulcus depth may be larger than originally described. Individual variability does exist; however, a methodology where bone sounding or transgingival probing is used to preoperatively determine the baseline dimensions of the supracrestal gingival tissues has been recommended196 ,575 ( Fig 1-18). This concept of biologic width is used as a guideline during the evaluation of periodontal-restorative interrelationships.196 Several authors have published various dimensions of the human dentogingival junction,196 ,572 ,575 –579 and it has been established that a minimum of 3-mm biologic dimension from the osseous crest to the restorative margin should be maintained supracrestally during restorative treatment196 ,531 ,577 ,580 to avoid impingement on the coronal attachment of the periodontal connective tissue. Placing the margin of the restoration infringing on biologic width can result in periodontal sequelae such as gingivitis, loss of clinical attachment, infrabony pocket formation, gingival recession, and bone loss.581 –587
Читать дальше