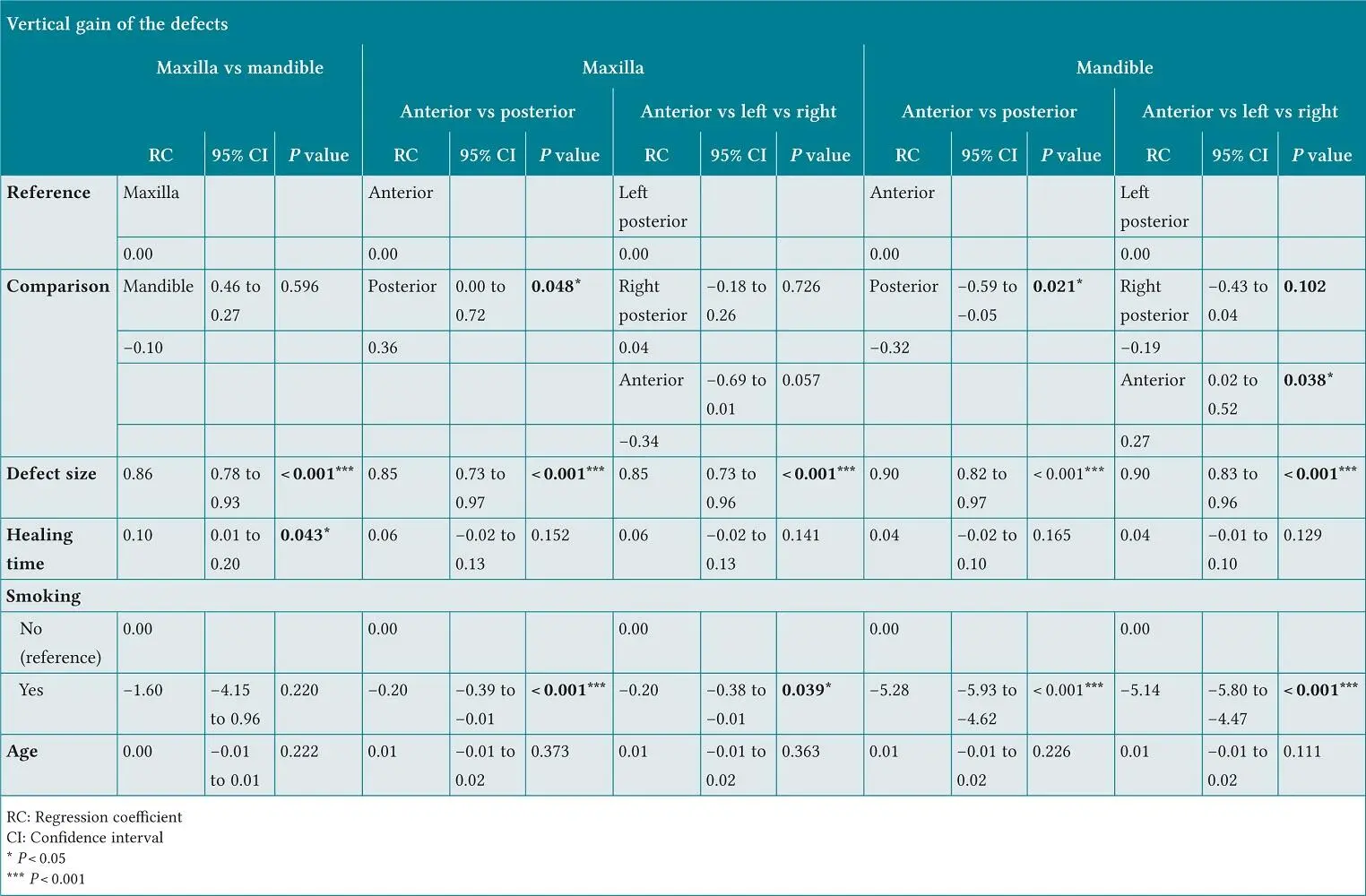
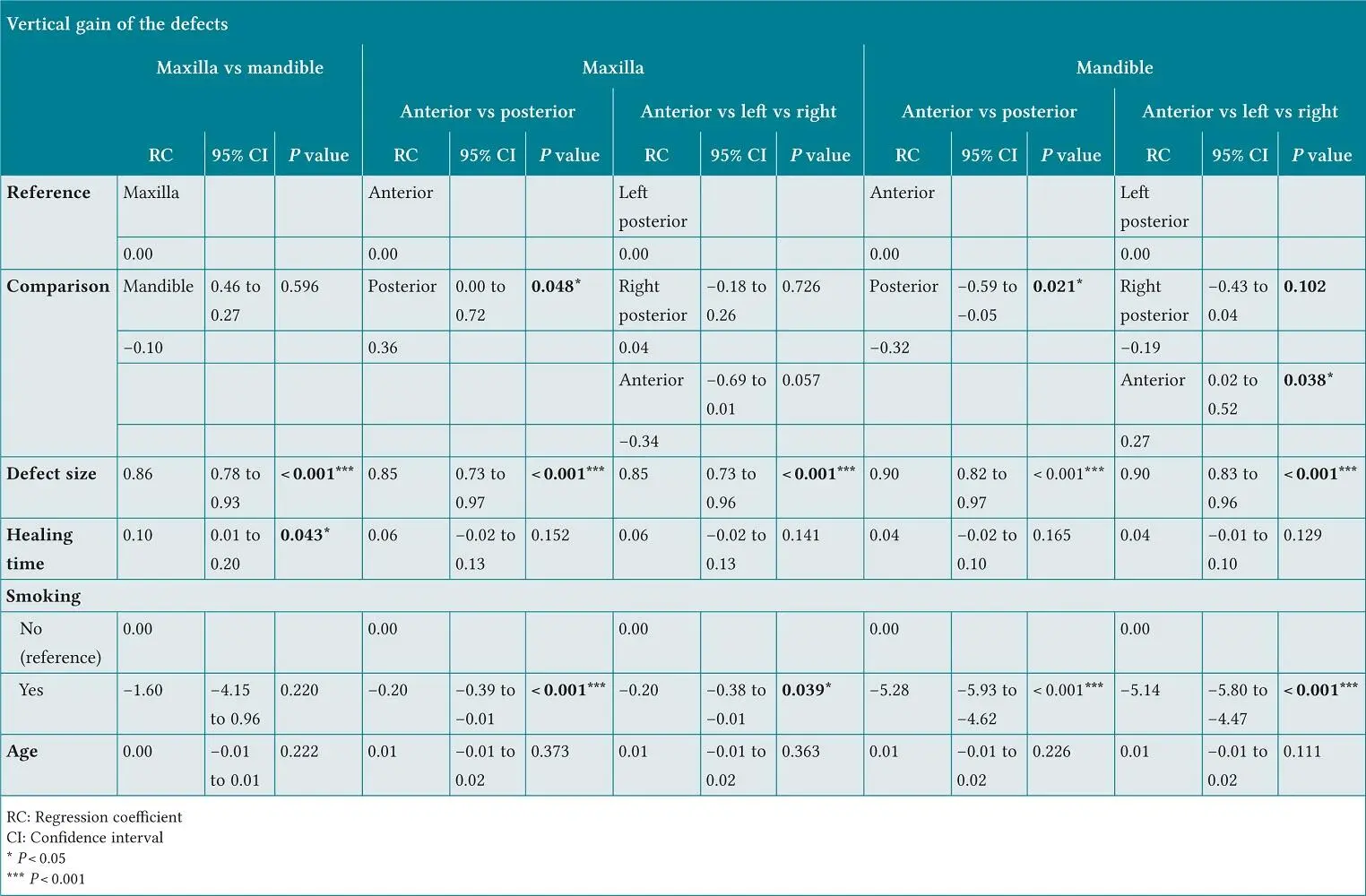
Table 2-4 Multiple linear regression analysis on the absolute vertical gain by sector controlling for defect size, arch, healing time, smoking, and age
Influence of defect location on absolute bone gain: anterior vs posterior
Out of the 29 maxillary vertical defects, 12 were anterior and 17 were posterior. The mean baseline vertical deficiency was 5.7 ± 2.7 mm anteriorly and 5.1 ± 2.4 mm posteriorly; these values were not statistically different ( P = 0.489). The mean absolute vertical gain was statistically higher in posterior sites than anterior ones by 0.36 mm ( P = 0.048) (see Table 2-4). The extent of the baseline vertical deficiency ( P < 0.01) and smoking ( P < 0.05) significantly affected maxillary absolute gain (see Table 2-4).
Out of 36 vertical defects, 4 were anterior and 32 were posterior. The mean vertical deficiency was 5.3 ± 1.0 mm anteriorly and 5.6 ± 2.9 posteriorly; these values were not statistically different ( P = 0.540). The mean absolute vertical bone gain was significantly greater in the anterior sites than the posterior ones by 0.32 mm ( P = 0.021) (see Table 2-4). The extent of the baseline vertical deficiency and smoking significantly affected mandibular absolute gain.
Influence of defect location on absolute and relative bone gain: anterior vs left posterior vs right posterior
In the maxilla, there were 12 anterior, 11 right posterior, and 6 left posterior defects. The mean vertical deficiency was 5.5 ± 2.9 mm on the right posterior side and 4.3 ± 0.8 on the left posterior side. There were no differences in absolute bone gain between maxillary left and right posterior sides per multiple linear regression ( P = 0.726). Maxillary anterior defects showed less bone gain compared with left and right posterior defects ( P = 0.05) (see Table 2-4and Fig 2-3a).
In the mandible, there were 4 anterior, 15 right posterior, and 17 left posterior defects. The mean vertical defect size was 5.8 ± 3.2 mm on the right posterior side and 5.5 ± 2.6 on the left posterior side, with no significant differences between the sides ( P = 0.72). A statistically significant difference in vertical bone gain was detected between the mandibular anterior, left posterior, and right posterior areas ( P = 0.028) (see Table 2-4and Fig 2-3b). The relative vertical gain was 98.3% for mandibular left posterior sites and 90.9% for right posterior sites (0.3 mm of absolute gain difference).
Postsurgical complications
There were only two cases (3%) with complications. One site presented membrane exposure (1-week postoperatively), and the graft material became infected at a second site. For the first case, the exposed membrane was maintained for 2 months and then removed. For the second case, the infected membrane and graft were explored and removed after 10 days of healing.
Vertical ridge augmentation using space-making frameworks and graft materials offers an ideal balance between the expected amount of bone gain and postoperative complications compared with other interventions. 4,5The rationale of GBR is based on the creation of a sheltered, soft tissue cell-excluding area to promote osteoblast migration. 6Dimensionally stable structures such as titanium-reinforced non-resorbable membranes or non-occlusive titanium meshes support vertical dimensions more reliably than cell-occlusive but pliant absorbable membranes. Although d-PTFE is a commonly used nonresorbable barrier material, it may exhibit subpar tissue adhesive properties that risk flap integrity. 7Innovators have developed materials that better approximate the periosteum to the underlying graft. Our study utilized a RPM perforated by macropores that theoretically improves vascularization by permitting direct contact between the periosteum and the bone grafts. To our knowledge, this is the first human case series to record the use of RPM for VBA.
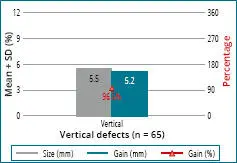
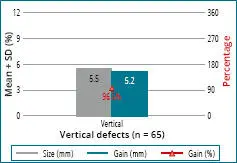
Fig 2-4 Graph showing defect size and absolute relative gain (SD = standard deviation).
Agreement with previous studies
Our case series achieved an absolute vertical bone gain of 5.2 ± 2.4 mm, which matched results reported in two previous case series by the author (IU (using titanium-reinforced d-PTFE membranes with the same bone graft composition that achieved mean height gains of 5.45 and 5.83 mm. 8,9In our study, a relative bone gain of 96.5 ± 13.9% was found, and complete vertical ridge regeneration in 89.2% of cases was achieved. Compared with the results of studies by the same author using nonporous d-PTFE, RPM seems to provide similar or better vertical bone gain. 2,8,9
Other studies using titanium-reinforced expanded polytetrafluoroethylene (e-PTFE) membranes reported similar results to ours. Urban et al 10attained a mean height gain of 5.5 mm using titanium-reinforced e-PTFE membrane and autologous bone for maxillary and mandibular, anterior and posterior VBA (staged or simultaneous). Can-ullo and Sisti 11demonstrated a mean height gain of 5.85 mm using titanium-reinforced e-PTFE membranes with magnesium-enriched hydroxyapatite for maxillary and mandibular, anterior and posterior VBA. Todisco 12achieved a mean vertical height of 5.3 mm using titanium-reinforced e-PTFE membranes with xenograft. Clinical VBA studies using nonresorbable membranes consistently report between 4 and 6 mm of vertical bone gain. 5,13-15
Although using space-making frameworks, including meshes and GBR membranes, results in fewer complications than distraction osteogenesis or block grafting, flap dehiscence is a chief concern. Absorbable membranes have been associated with more complications than nonresorbable ones. 16
This contrast holds true when VBA-only procedures are considered – for these surgeries, absorbable membranes have complication rates of 23%, whereas PTFE membranes have rates of 7%. 5However, not all nonresorbable membranes behave similarly. e-PTFE membranes present with twice the number of complications compared with d-PTFE barriers. 5Our study employing a novel PTFE mesh had a fairly low complication rate (3%). Two complications involved membrane exposure at 1 or 8 weeks post-VBA, which accorded with a previous study reporting early and late exposure (as early as 1 week and up to 6 months postoperatively). 16
Most studies investigating VBA report only mean vertical bone gain (absolute bone gain) and fail to calculate the relative percentage of bone gain with respect to initial defect size. We detected significant indirect correlations between baseline vertical deficiency and the amount of bone gained: as the baseline deficiency increased millimeter by millimeter, the probability of achieving complete regeneration decreased by 2.5 times. VBA achieved 6% to 12% greater relative bone gain when used for smaller height deficiencies (< 5 mm) compared with larger ones (≥ 5 mm) ( Fig 2-4).
Ours may be the first VBA study to investigate the effect of defect location on height gain. We did not find significant differences between the maxilla and mandible in terms of bone gain. However, the location of the defect within either jaw statistically influenced the amount of augmentation generated. In the maxilla, absolute bone gain was statistically greater in the posterior than the anterior area, with a mean difference of 0.36 mm. In contrast, absolute bone gain in the mandible was statistically greater in the anterior than in the posterior area, with a mean difference of 0.32 mm. The mean height gain differences were < 0.5 mm, which may have no clinical significance.
Читать дальше