1 ...6 7 8 10 11 12 ...29
LEARNING GOALS AND OBJECTIVES
The patient’s chief complaint
Medical and dental history
Soft tissue and gingival examination
Periodontal charting
Radiographic interpretations
Periodontal diagnosis
ASA classification 1
Vital signs: blood pressure 130/80 mmHg
Medication: none
Supplement: daily multivitamin
Allergy: none
The patient brushed three times daily and flosses daily.
The patient had received routine dental prophylaxis at her general dental practitioner’s office. Recently, the patient underwent extraction of her mandibular left first and second molars due to severe periodontal disease, and she would like to replace them with dental implants.
The patient denied any smoking habit and had never smoked.
The patient’s father suffered from periodontal disease and ended up receiving complete maxillary and mandibular removable dentures.
Patient was extremely motivated for dental treatment.
Soft Tissue and Gingival Examination
Extraoral examination did not reveal any significant findings. Intraorally, generalized gingival edema and erythema were noted ( Figure 1.1.1), which were more pronounced on #3 buccal, #8 buccal, #8 palatal, interproximal papilla between #8 and #9, interproximal papilla between #9 and #10, buccal gingival margin and interproximal papillae in mandibular incisors; rolled buccal gingival margins were noted on #3 mesiobuccal and #8 mesiobuccal aspect.
Comprehensive Periodontal Examination
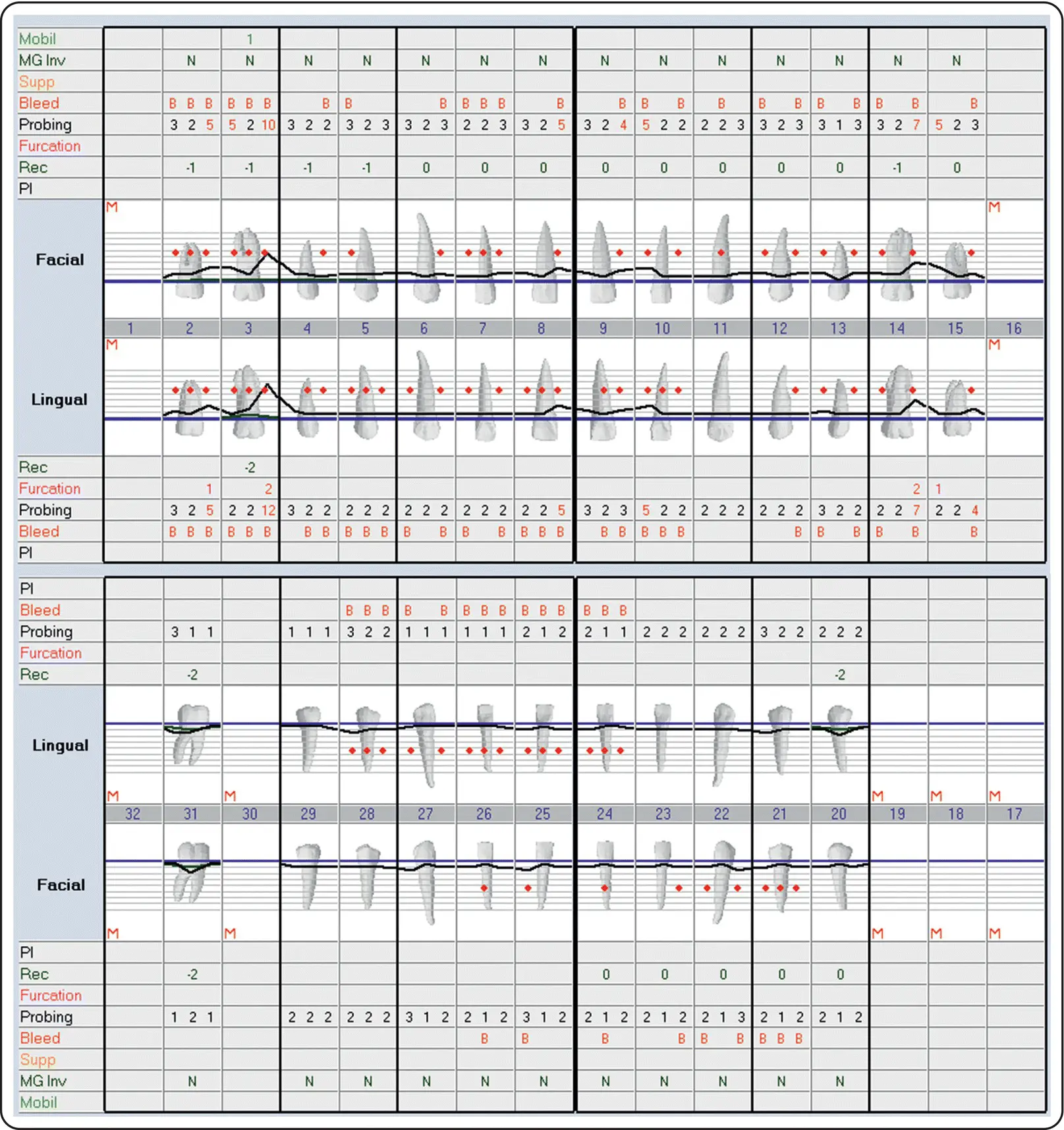
A comprehensive periodontal examination ( Figure 1.1.2) revealed localized deep probing depths of 10–12 mm on tooth #3 mesial aspect with grade I mobility and grade II mesiopalatal furcation involvement. Tooth #14 exhibited localized deep probing depths of 7 mm on its distal aspect with grade II distopalatal furcation involvement. Teeth #2, #8, #10, and #15 also exhibited localized probing depths of 5 mm. Teeth #2 and #15 exhibited Class I mesiopalatal furcation involvement. Otherwise, the remaining dentitions exhibited generalized probing depths of 1–4 mm. There was generalized bleeding on probing. Furthermore, localized areas with gingival recession were noted in some posterior teeth.

Figure 1.1.1Complete series of intraoral photographs.
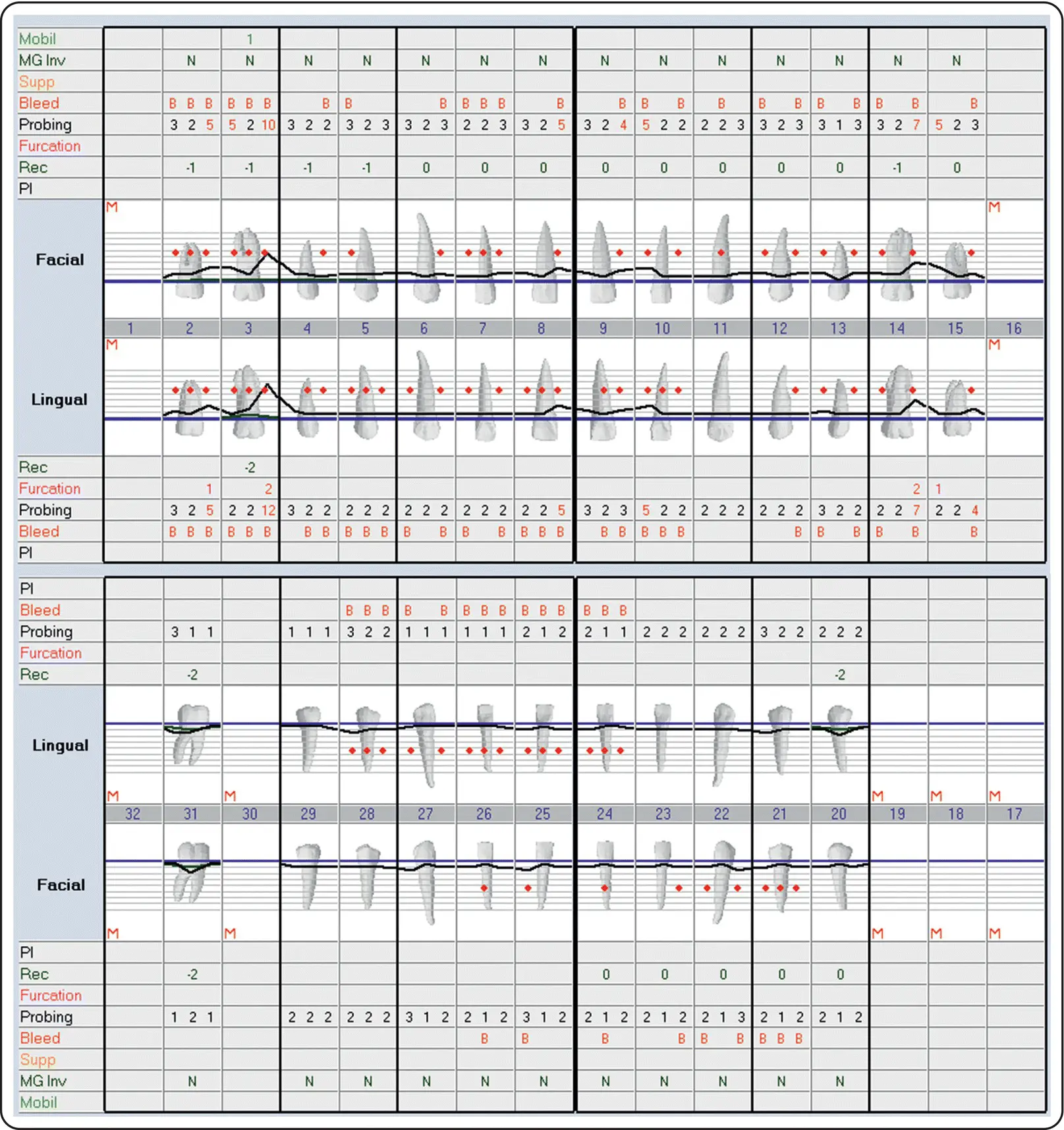
Figure 1.1.2Complete periodontal charting.
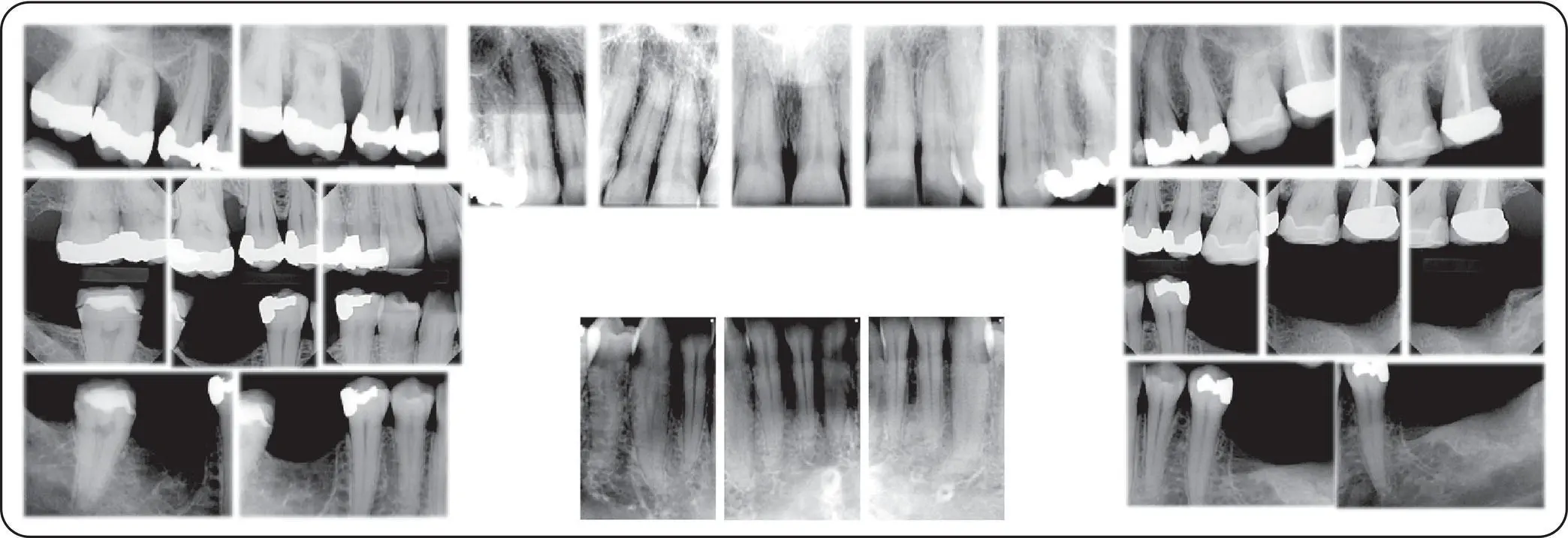
A full‐mouth series of intraoral radiographs revealed generalized horizontal bone loss ( Figure 1.1.3). There was localized moderate horizontal bone loss on teeth #2 and #15. Tooth #3 exhibited vertical bone loss on its mesial aspect while tooth #4 exhibited vertical bone loss on its distal aspect. An open interproximal contact was evident on #3 mesial aspect. Vertical ridge deficiency was noted on edentulous teeth #18, #19 and #30, areas with slight radiolucency indicating possible horizontal ridge deficiency as well.
According to the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions by the American Academy of Periodontology and the European Federation of Periodontology [1], the patient exhibited stage III grade C periodontitis (localized).
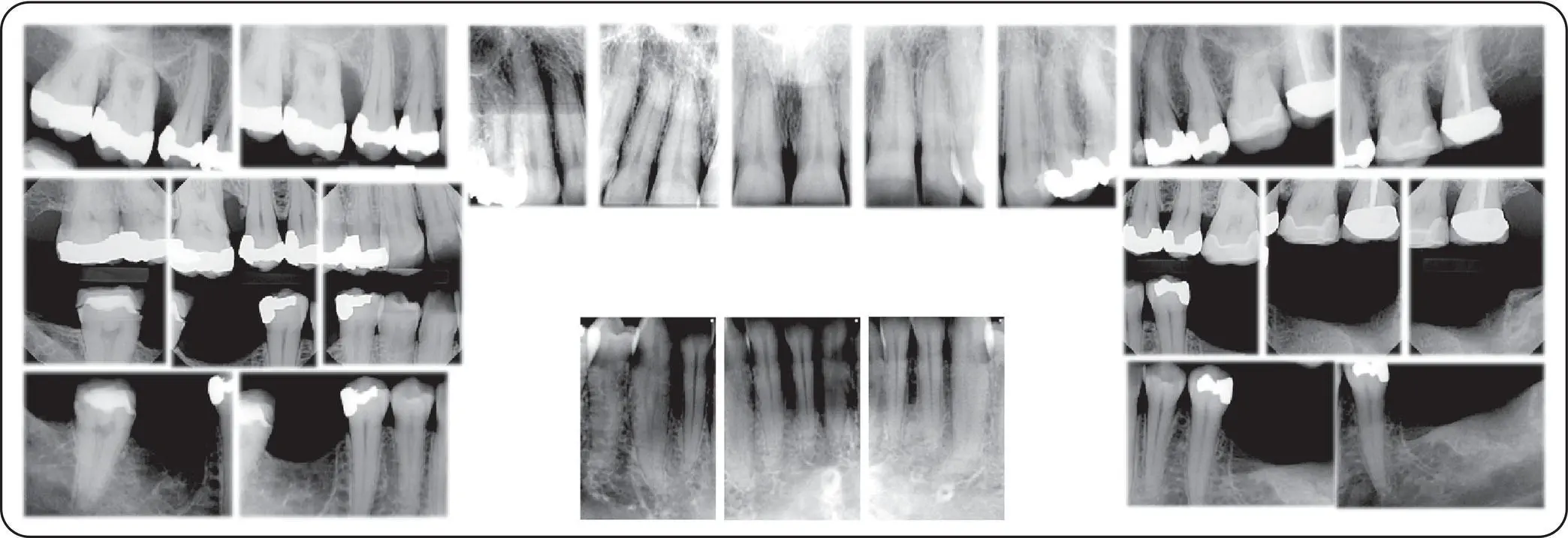
Figure 1.1.3Complete series of intraoral radiographs.
1 What is the significance of obtaining medical and dental history in treating a patient with periodontal conditions?
2 Aside from conventional parameters such as probing depth, recession, mobility and bleeding on probing, what are the additional parameters that should be obtained during a comprehensive periodontal evaluation?
3 How did we derive periodontal diagnosis for this case of interest?
4 What is the importance of conducting a comprehensive periodontal evaluation for a patient who needs a dental implant?
5 Aside from periodontal charting, are there any other clinical findings that clinicians should record during their routine comprehensive examinations?
Answers located at the end of the chapter.
1 1. Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. J Periodontol 2018; 89(Suppl 1):S173–S182.
2 2. Kwon T, Levin L. Cause‐related therapy: a review and suggested guidelines. Quintessence Int 2014; 45(7):585–591.
3 3. Eke PI, Wei L, Thornton‐Evans GO, et al. Risk indicators for periodontitis in US adults: NHANES 2009 to 2012. J Periodontol 2016; 87(10):1174–1185.
4 4. Grossi SG, Zambon JJ, Ho AW, et al. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J Periodontol 1994; 65(3):260–267.
5 5. Grossi SG, Genco RJ, Machtei EE, et al. Assessment of risk for periodontal disease. II. Risk indicators for alveolar bone loss. J Periodontol 1995; 66(1):23–29.
6 6. Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol 1965; 36:177–187.
7 7. Hirschfeld L, Wasserman B. A long‐term survey of tooth loss in 600 treated periodontal patients. J Periodontol 1978; 49(5):225–237.
8 8. McFall WT. Tooth loss in 100 treated patients with periodontal disease. A long‐term study. J Periodontol 1982; 53(9):539–549.
9 9. McGuire MK, Nunn ME. Prognosis versus actual outcome. III. The effectiveness of clinical parameters in accurately predicting tooth survival. J Periodontol 1996; 67(7):666–674.
10 10. Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol 1972; 43(10):623–627.
11 11. Thakur AM, Baburaj MD. Analysis of spontaneous repositioning of pathologically migrated teeth: a clinical and radiographic study. Quintessence Int 2014; 45(9):733–741.
12 12. Berglundh T, Armitage G, Araujo MG, et al. Peri‐implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. J Periodontol 2018; 89(Suppl 1):S313–S318.
13 13. Schwarz F, Derks J, Monje A, Wang H‐L. Peri‐implantitis. J Clin Periodontol 2018; 45(Suppl 20):S246–S266.
14 14. Ferreira SD, Martins CC, Amaral SA, et al. Periodontitis as a risk factor for peri‐implantitis: systematic review and meta‐analysis of observational studies. J Dent 2018; 79:1–10.
15 15. Swierkot K, Lottholz P, Flores‐de‐Jacoby L, Mengel R. Mucositis, peri‐implantitis, implant success, and survival of implants in patients with treated generalized aggressive periodontitis: 3‐ to 16‐year results of a prospective long‐term cohort study. J Periodontol 2012; 83(10):1213–1225.
16 16. Clark D, Levin L. Dental implant management and maintenance: how to improve long‐term implant success? Quintessence Int 2016; 47(5):417–423.
17 17. Jepsen S, Caton JG, Albandar JM, et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. J Periodontol 2018; 89(Suppl 1):S237–S248.
Читать дальше