The impact of mandibular ridge height on masticatory function following mandibular IOD treatment was further reinforced by Fontijn-Tekamp et al. 36Masticatory function in subjects with resorbed mandibles was significantly greater with the IOD compared with the CD. However, the masticatory performance of the IOD group with a resorbed mandible was still lower than the performance of a group of subjects with good mandibular residual ridges treated with CDs. It is clear that the benefits in masticatory function of IOD treatment are evident only in patients with relatively resorbed mandibular ridges and that the improvement in masticatory function is only to the level of a CD wearer with a good mandibular residual ridge.
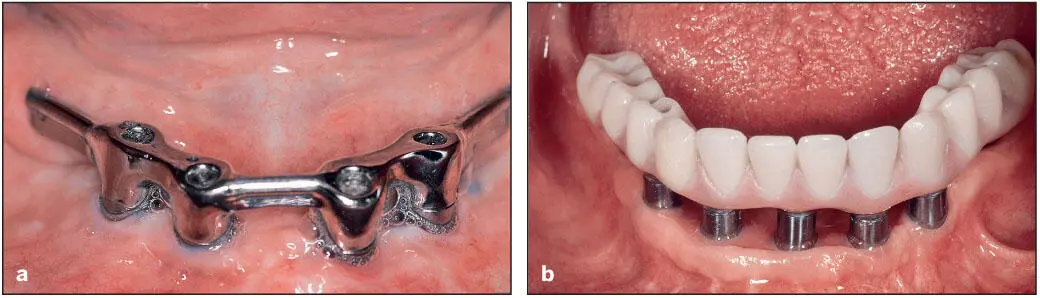
Increasing the number of implants in the mandible to four to six to support an overdenture ( Fig 6-8a) has been found to offer little advantage in masticatory function. Geertman et al 33found that the additional support provided by transmandibular implants and a fully implant-supported denture did not improve masticatory performance compared with the two-implant overdenture. The authors concluded that the increased retention and stability of the mandibular denture determined the denture wearer’s ability to grind up food during mastication, rather than the degree of support provided by implants. Tang et al 37reported a similar lack of difference in masticatory function based on within-subject comparisons of a mandibular long-bar (four implants) overdenture and a two-implant overdenture.
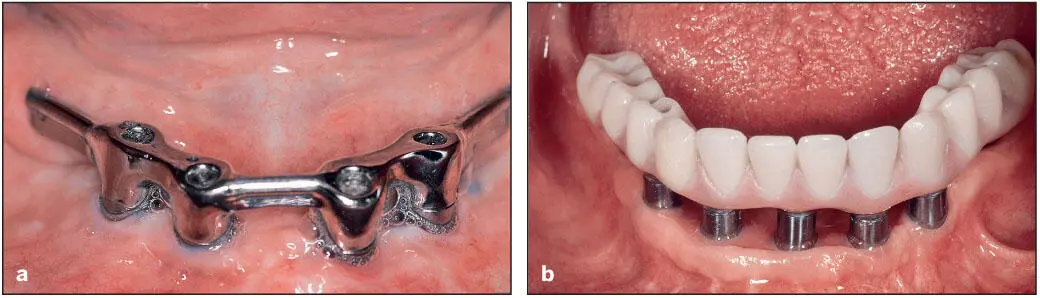
Fig 6-8 (a) Implant-supported bar design. (b) The original fixed hybrid prosthesis design sitting atop conventional titanium abutments.
Feine et al 38extended the comparison of masticatory function with removable implant-supported long-bar overdentures to fixed prostheses ( Fig 6-8b) in a within-subject crossover study. The fixed prosthesis offered no improvement over the implant-supported overdenture. In fact, the long-bar overdenture resulted in significantly better masticatory times for three of the five foods evaluated.
Lindquist and Carlsson, 39, 40on the other hand, found that patients who were not satisfied with acceptable CDs and those treated with mandibular implant-supported fixed prostheses experienced significant improvement in masticatory function. However, the addition of an implant-supported fixed prosthesis in the maxilla did not result in any improvement in masticatory performance over the mandibular fixed prosthesis opposing a maxillary CD.
Patient satisfaction
Patient perceptions of denture function
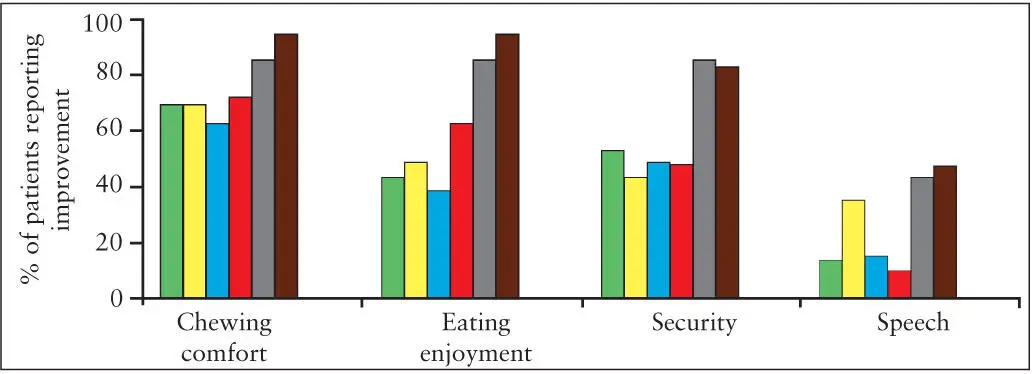
In general, patients report high levels of satisfaction with almost all prosthodontic interventions, including rehabilitation with dental implants. For example, improvements to the denture base fit, occlusion, and occlusal vertical dimension of clinically poor dentures, as well as delivery of new CDs, generate high percentages of patients reporting improved function and security with each change in the denture 41( Fig 6-9). Relatively high satisfaction with CDs is often seen in general samples of denture wearers, such as the 82% reporting good global satisfaction with their dentures in the study by Gjengedal et al. 4However, changes in patient perceptions from baseline with CDs to treatment with prostheses retained or supported by dental implants have been used to recommend implant-based therapies.
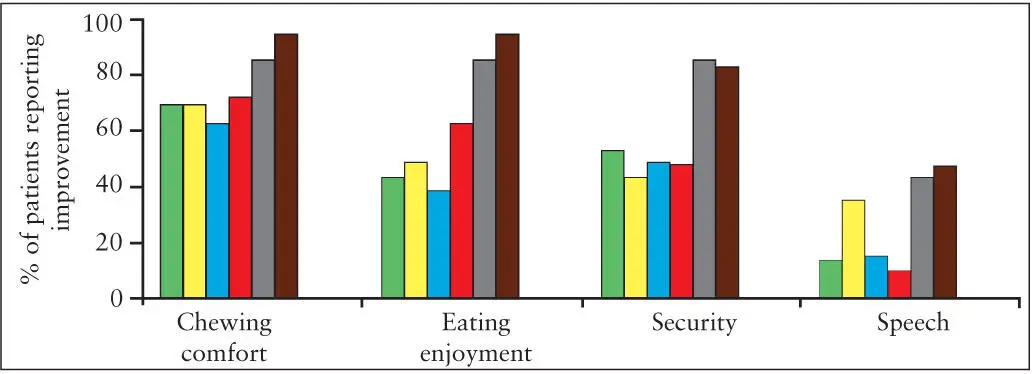
Fig 6-9 Percentage of patients reporting improvement in denture satisfaction regarding changes in occlusion (green) , vertical dimension (yellow) , and use of denture adhesive (blue) as well as after relining (red) and 3 weeks (gray) and 3 months (brown) after the delivery of new dentures. (Based on data from Garrett et al. 42)
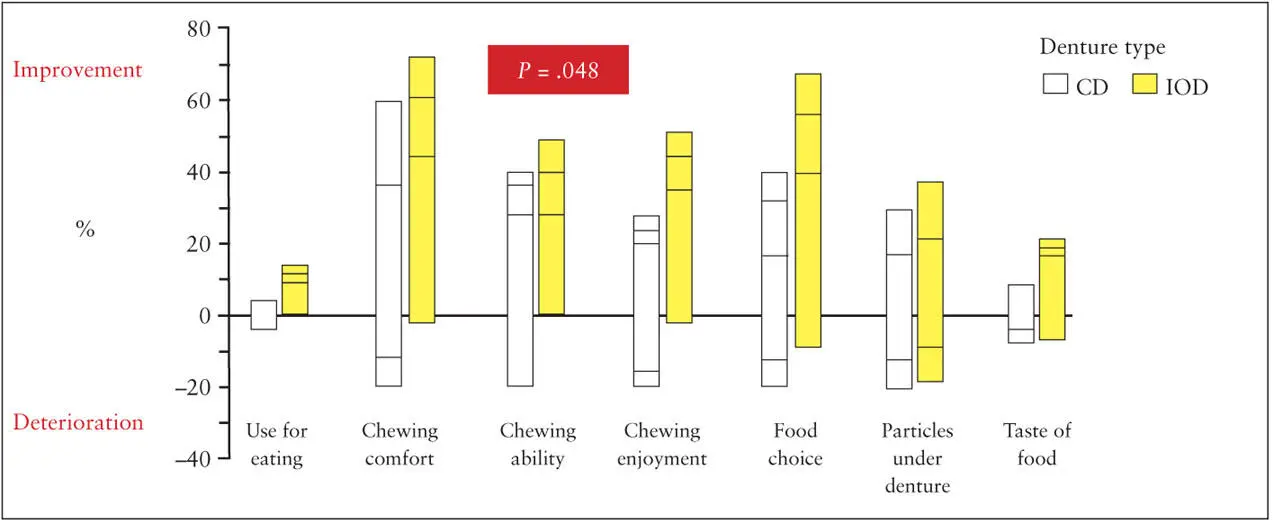
For patients generally dissatisfied with CDs (ie, more than 90% of the sample) and with severely resorbed mandibles, two-implant mandibular overdentures produce significant improvement in patient satisfaction compared with CDs. 43, 44In patients with relatively good residual ridges and little dissatisfaction with their existing CDs, comparisons of CD patients randomized to treatment with another CD or a two-implant overdenture in the mandible opposing a new maxillary CD found that a significantly higher percentage of patients with the IOD noted improvements in chewing ability after 6 months ( Fig 6-10), while there was little difference between the two groups at 24 months posttreatment. 45The lack of difference at 24 months may indicate that some patients took longer to adapt to their new CDs compared with the IOD wearers. More than 84% of the patients were moderately or fully satisfied and experienced little or no discomfort with new CDs, and no significant differences were seen in denture satisfaction with the new IOD. Although not statistically significant, the patient satisfaction levels regarding chewing ability, chewing comfort, and food selection were somewhat higher with the IOD compared with the CD.
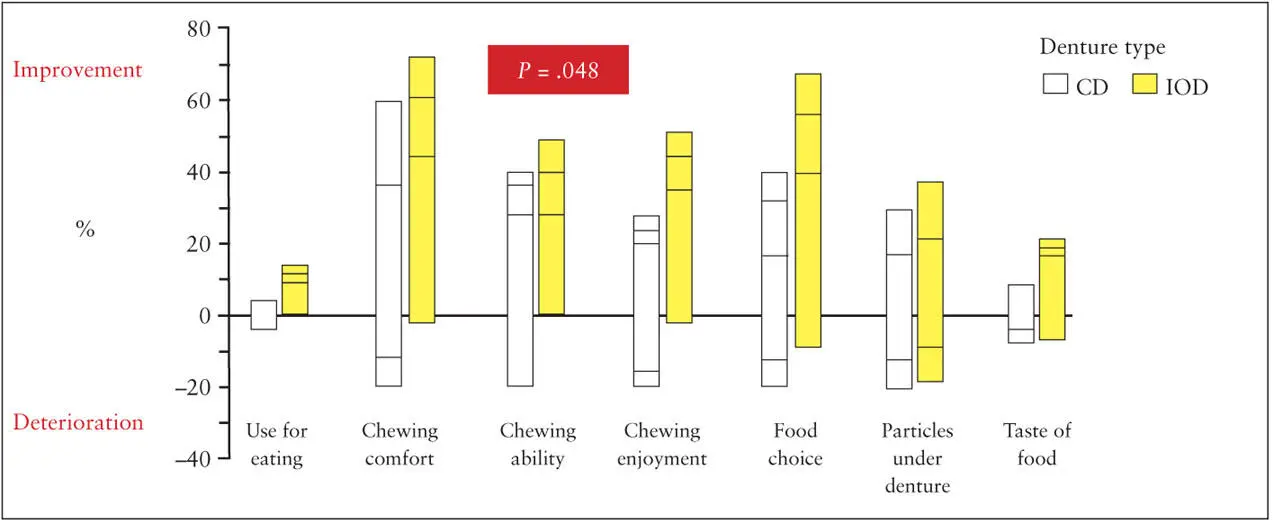
Fig 6-10 Percentage of patients reporting improvement or deterioration 6 months after placement of new CDs or IODs. (Reprinted from Kapur et al 45with permission.)
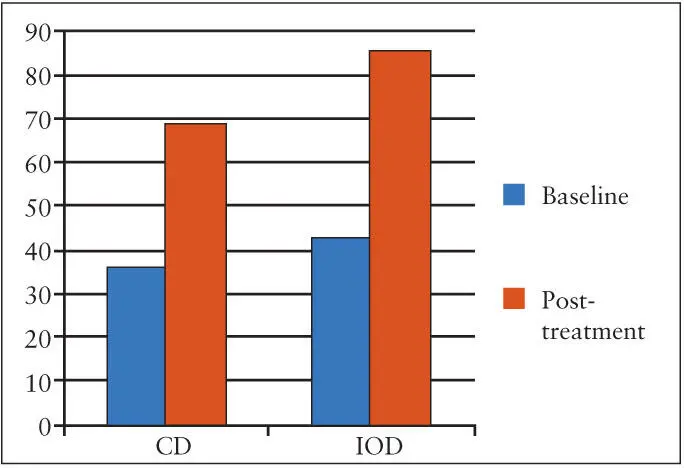
A similar study compared the effects of new CDs and mandibular implant overdentures on the perceptions of patients who had low satisfaction scores with their original CDs. 46, 47Perceptions regarding general satisfaction, comfort, stability, and chewing ability significantly improved following provision of new maxillary CDs with either a mandibular CD or IOD. The ratings on a visual analog scale for these four perceptions were significantly greater with the IOD compared with the CD, but some of this difference can be accounted for by the poorer ratings the CD group gave their original dentures compared with the IOD group. However, while both treatments provided considerable perceived improvement, the impact of IODs on patient ratings of satisfaction, comfort, stability, and chewing was greater than that of the CDs. These benefits of the IOD in treatment satisfaction have been extended to international populations in a study incorporating the many elements of an effectiveness trial, indicating that this benefit is likely to persist at the private practitioner level. 48Unlike as in RCTs, participants in this study selected the type of treatment (ie, CD or IOD) they preferred. As evident in Fig 6-11, while general satisfaction with the new prosthesis improved with both CD and IOD treatment, the magnitude of improvement is greater for those receiving the IOD.
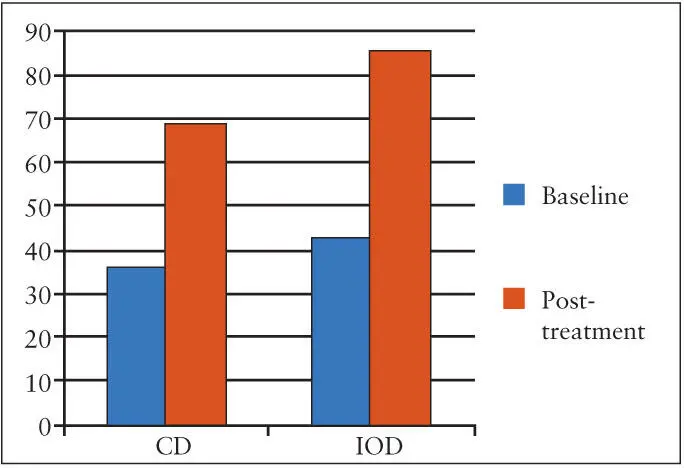
Fig 6-11 Mean in general satisfaction rating on 100-mm visual analog scale of mandibular prostheses with both CD and IOD treatment. (Based on data from Rashid et al. 48)
Improvements in treatment satisfaction and oral health quality of life (OHQoL) were seen for patients requesting CD or IOD treatment and receiving their preferred treatment. 49, 50Again the improvements were greater for the IOD group. However, patients requesting the IOD but receiving CD treatment showed no change in satisfaction or QoL. Clearly, patient expectations play a significant role in achieving treatment satisfaction.
Читать дальше