Various methods have been used to prevent this initial contraction and the subsequent resorption, including immediate implant placement and socket preservation. 28However, human studies assessing the effect of preservation of the alveolar bone are limited. Animal studies using nonresorbable bone substitutes or autologous bone particulates appeared to induce bone formation within the socket space 29, 30; however, these procedures do not seem to completely prevent bone resorption activity on the external surfaces of the extraction socket, resulting in the development of a knife-edge residual ridge. New biomaterials and techniques to minimize contraction of the oral mucosa and resorption of alveolar bone can provide more predictable management of the soft and hard tissues around dental implants.
Bone density
In a classic study by von Wowern and Gotfredsen, 31the placement of two implants in the canine region prevented the long-term (5 years) reduction of bone mineral content (bone density) adjacent to the implant site. It has been postulated that implants retaining the mandibular overdenture will prevent compression of the mucoperiosteum anteriorly; if the denture properly engages the primary support areas posteriorly (buccal shelf and retromolar pad), there should be little resorption of the intervening alveolar ridge and mandibular body. The benefit should be considerable when the opposing maxilla is fully or partially dentate.
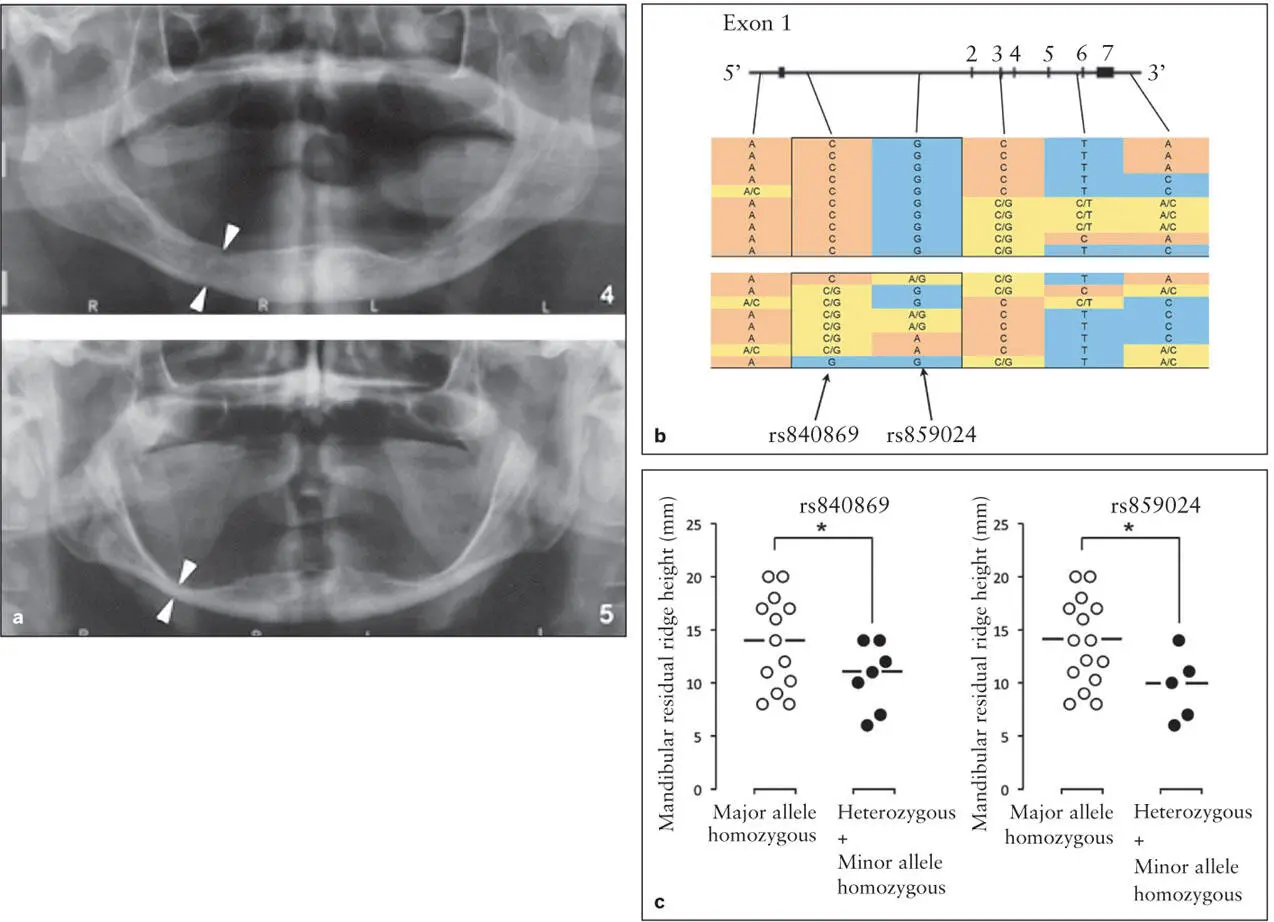
Interestingly, there have been numerous reports of the size and density of the mandibular body increasing following the placement of implants in the mandibular symphysis and the fabrication of a fixed implant-supported prosthesis 32( Fig 6-5). While this phenomenon appears to be most common in patients with severe resorption, the causes of have yet to be determined. Davis et al 32speculated that with the occlusal forces concentrated anteriorly and when those forces increased dramatically during function, significant bending moments are created in the body of the mandible that produce tensional forces on the superior surface, provoking osteoblastic activity and deposition of bone. The role of biomechanics on bone remodeling is detailed in chapter 3.

Fig 6-5 (a and b) Implants placed into a moderately resorbed mandible. (c) A fixed hybrid prosthesis was fabricated. Note the additional bone formed over the inferior alveolar nerve 10 years after delivery. (Courtesy of Dr H. Davis.)
Genetic factors
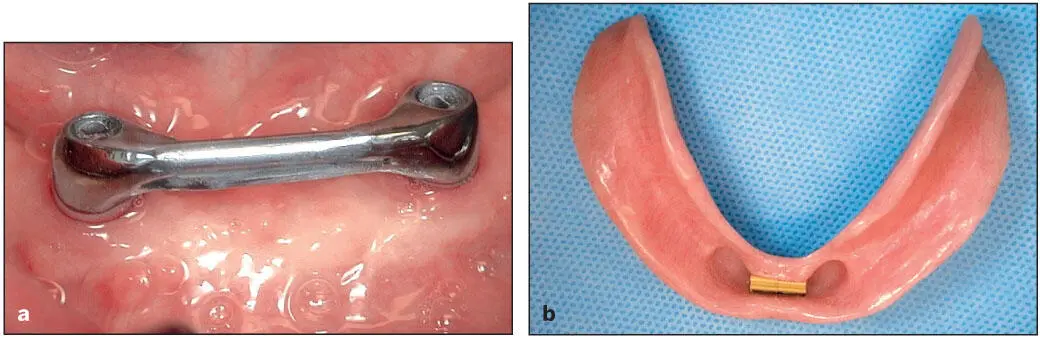
Implant placement after dental extraction for the purpose of maintaining the alveolar bone has been a well-accepted practice. However, implants do not prevent bone loss in all cases, and it is possible that the oral mucosa may play a role under certain combinations of risk factors. It is increasingly clear that many diseases and afflictions are caused by the interactions among genetic and environmental factors. If the placement of implants and denture-induced compression of the mucoperiosteum of the alveolar ridge are considered environmental factors, the individual variations in response to similar treatment may be related to the patient’s genetic factors. Using FGFR1OP2/wit3.0 as a genetic paradigm, Suwanwela et al 25demonstrated a method that may be used to identify those patients at risk for rapid bone resorption upon becoming edentulous. Two out of six single-nucleotide polymorphisms (SNPs) within the FGFR1OP2/wit3.0 genetic allele were strongly associated with severe mandibular atrophy 25( Fig 6-6). Current dental practice employs minimal clinical testing and bases the diagnosis and the prognosis of each patient almost entirely on empiric experiences. In the future, it may be possible that genetic screening tests using oral rinse or cheek swab samples will be available to assist with this problem.
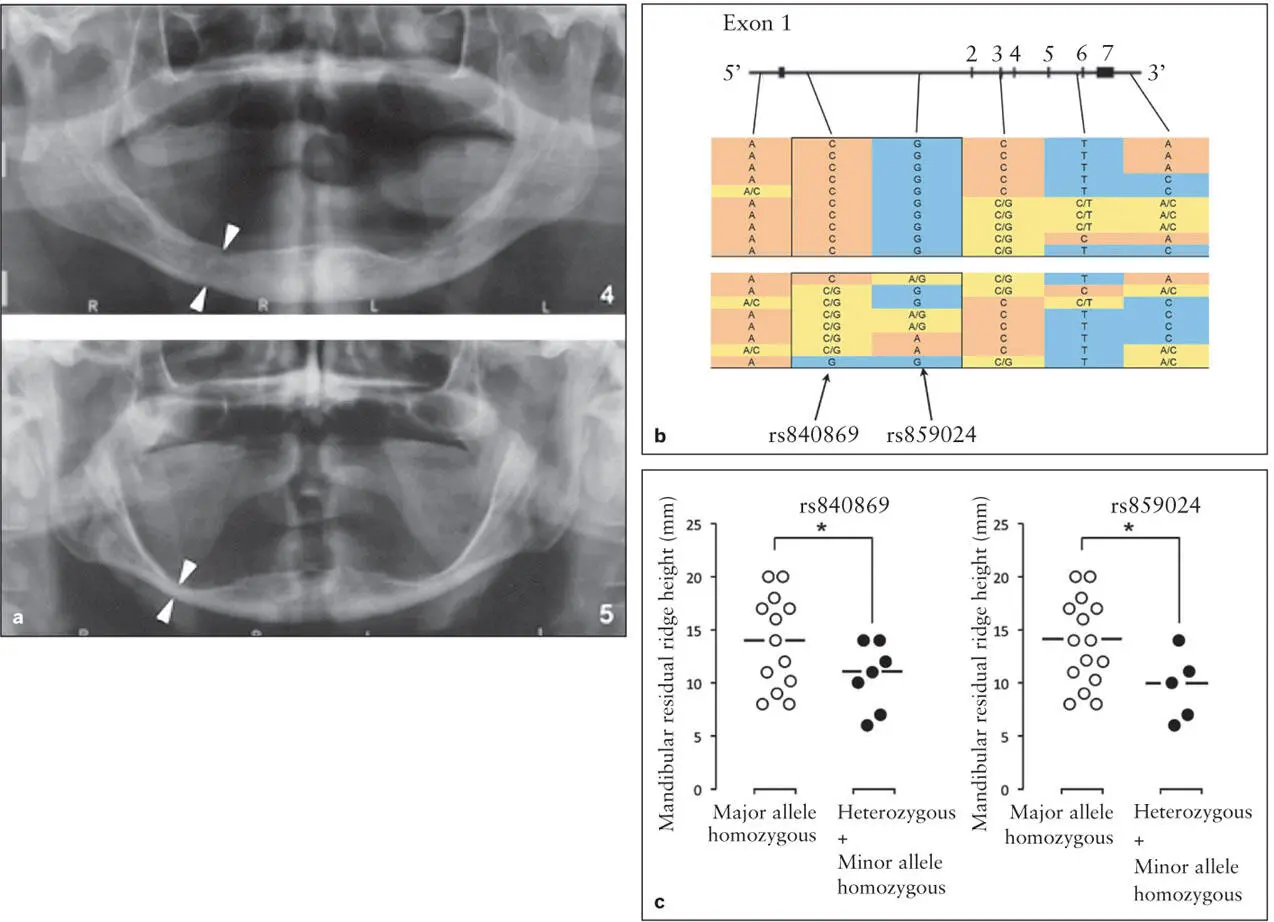
Fig 6-6 Twenty long-term edentulous patients were recruited for a genetic association study. The mandibular residual ridge height was measured following the protocol of the American College of Prosthodontists. Two SNPs in the FGFR1OP2/wit3.0 gene were positively associated with atrophic mandibular residual ridges. This pilot study may suggest a possible genetic screening test for better prognosis of severe residual ridge resorption even prior to tooth extraction. (a) Panoramic radiographs illustrating ridge resorption. (b) SNP alleles in FGFR1OP2/wit3.0 . (c) Ridge heights for SNP alleles. (Reprinted from Suwanwela et al 25with permission.)
The authors believe that the placement of two implants into the anterior mandible to retain an overdenture will minimize further resorption of the alveolar ridge and the body of the mandible. A properly engaged retromolar pad and buccal shelf provide posterior support while the implants provide anterior support. In addition, the implants minimize lateral and posterior displacement and movement of the denture during function and parafunction. In addition to the environmental control by clinical procedures, genetic diagnosis may become available in the future.
Clinical Outcomes: Mastication, Satisfaction, and Diet
Masticatory function
Concern with restoration of function following tooth loss as well as frequent complaints by denture wearers regarding chewing difficulties have resulted in considerable research on masticatory function with compromised dentition. In the case of the edentulous patient, early studies of dentate patients and complete denture wearers demonstrated that significant impairment in masticatory function remains following treatment with complete dentures. Masticatory performance (degree of particle breakdown) with complete dentures is typically less than half of that achieved by persons with relatively intact dentition (28 or more teeth). It was hypothesized that with the improved stability and retention gained when the mandibular denture is retained or supported by dental implants, significant improvements in masticatory function would be achieved. A number of well-controlled clinical trials have been conducted evaluating the restoration of masticatory function with implant-retained mandibular dentures compared with conventional complete dentures.
Geertman et al 33evaluated masticatory performance in patients receiving a two-implant bar-retained overdenture (IOD) or CD in the mandible opposing a new maxillary CD. The group treated with the IOD in the mandible had significantly greater masticatory performance than the CD group. A key element in this study was the sample characteristic that all subjects had severely resorbed mandibles. In another randomized controlled trial (RCT) comparing treatment with a mandibular IOD ( Fig 6-7) or CD opposing new maxillary CDs, Garrett et al 34reported no significant difference in masticatory performance between the two treatment groups. However, the subjects for this study were not selected because of dissatisfaction with their CDs or severe resorption of the mandibular residual ridge, and the overall residual ridge height for the sample was generally good. When subjects in this study were stratified for residual ridge height, those subjects with more resorbed mandibular ridges were found to have significantly greater masticatory performance with the IOD compared with the CD. 35
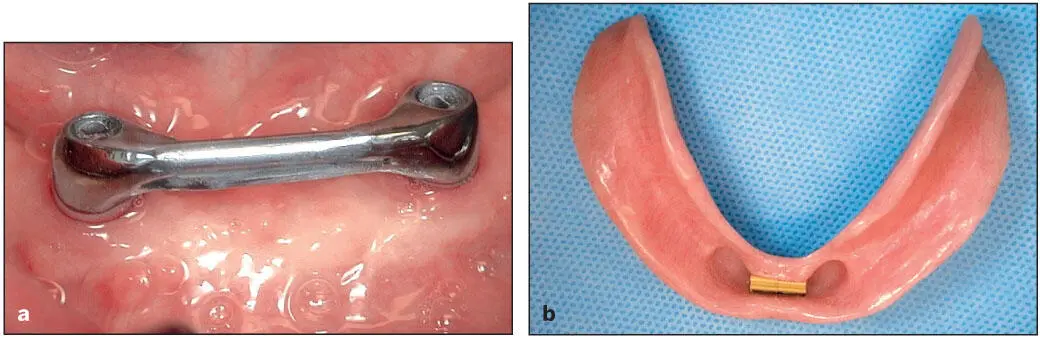
Fig 6-7 (a) An implant-assisted Hader bar fabricated with UCLA-type abutments has been screwed onto the implants. (b) Overdenture with Hader clips.
Читать дальше