1 ...6 7 8 10 11 12 ...15 During specialist practice, it is recommended that a series of action learning sets are undertaken. These action learning sets can be inter‐professional, facilitating understanding of professional roles and responsibilities, which may help to support the delivery of an integrated care workforce (Gilburt, 2016). The process is based on the idea that effective learning and development has to be about real problems in real life with real people (Raelin, 1998). Through action learning, individuals learn with and from each other by working on real problems and reflecting on their own experiences (Haydock and Evers, 2014).
The benefits of action learning are:
Greater breadth in understanding collaboration and inter‐professional learning to build up relationships in community nursing practice.
Increased ability to analyse ambiguous situations and solve complex problems.
Enhanced capacity to understand and initiate changes that increases the focus on what makes a difference in a situation.
Better ability to be more action focused and proactive in delivering results.
Enhanced self‐awareness and appreciation of personal impact on others, contributing to improved ability to work with others.
Developed flexibility in responding to changing situations
Shared knowledge and learning.
Students are able to listen to and reflect upon others’ experiences, ask questions, gaining different perspectives (Pedler and Abbott, 2008). When members share information and resources, it provides practical and emotional support. The student and the practice assessor and practice supervisor should actively work together to participate in the action learning sets, which may be recorded and included as evidence in the portfolio.
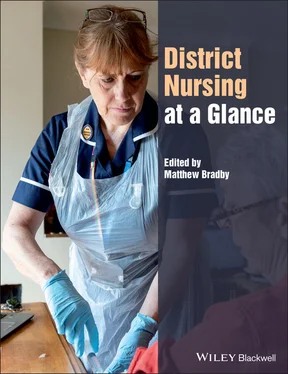
5 Supporting nursing students in the community
Josephine Gray, QN
Box 5.1Examples of clinical skill experiences students may undertake during their community placement.
Care of the diabetic patient, blood glucose monitoring and insulin administration.
Continence advice and assessment and knowledge of incontinence products, order and supply.
Tissue viability. Methods of wound assessment and correct choice of dressings. Venous and arterial leg ulcer management. Doppler assessment and compression bandaging. Pressure damage prevention and treatment and ordering of pressure‐relieving equipment.
Medicines management and community prescriptions. Administration of intramuscular and subcutaneous injections. Application of creams and lotions, eye and ear drops. PV and PR medications administration and use.
End‐of‐life care at home and in residential home. Syringe driver management. Care at time of death, verification of death and support for family and friends.
Intravenous medication administration. Care of central lines and cannula. Chemotherapy disconnection.
Care of patients living with dementia in their own home and in residential care.
Lone working, autonomous practice and insight into safety awareness in the community.
Teaching professional carers specific tasks under a shared care protocol.
Box 5.2Members of the multidisciplinary team that students may meet or work with during their community placement.
General practitioners
Practice nurses
Community physiotherapists
Community occupational therapists
Community psychiatric nurses
Podiatrists
Practice managers
Community matrons
Specialist nurses (e.g. respiratory, cardiac rehabilitation, heart failure, Parkinsons)
Community hospice nurses
Health visitors
School nurses
Community midwives
In recent years there has been a shift from care in hospital to more care being provided in the community, a move emphasised in the NHS Long Term Plan . In view of this, schools of nursing have had to adapt their teaching programmes so that students are prepared for this transition. Within the last few years, community placements have changed so that students can experience community nursing in all 3 years of their training.
Each learning establishment will have a different programme based on the fundamentals set down by the Nursing and Midwifery Council and each placement will differ in experience as community nursing is so diverse; however, the basic principles remain.
Year 1 focuses on the fundamental basics of nursing, all of which should be achievable in the community ( Box 5.1). For some students, it will be their very first placement so they will need extra support. Up to 50% of this placement will be spent with their workplace mentor and the remaining time will be with other team members and working with other professionals in the multidisciplinary team ( Box 5.2). They will be introduced to the everyday working of a community nursing team and experience the basics of community care. The mentor will introduce some of the key aspects of nursing during this placement.
The first action when working with the student will be to set out learning objectives. These will be a combination of both the fundamentals of nursing below and clinical tasks and skills.
Reflection: Students will be expected to complete many reflective pieces during their training. This will be introduced from the beginning of their course and they will be expected to complete at least one reflection during each community placement.
Portfolio: All nurses in training will be expected to complete a portfolio. Evidence from community placement must be collected, referenced and included in this.
Multidisciplinary working: There are opportunities to work with multidisciplinary teams working in the community. The student will learn how shared care is provided in order to maximise a high standard of patient care.
Record keeping: Meeting patients who have numerous sets of notes can be confusing. Most electronic NHS records should soon be within the same set of case notes. However, care agencies will always keep separate documentation.
Experience the patient‐centred care approach
The student will practice assessments, complete medicine charts and care plans under supervision, and identify how this information is shared with other disciplines.
The student may encounter difficult family dynamics, which can be heightened in times of illness and at the end of life, and will also visit home environments that are between the two extremes of poverty and wealth. The student must learn to be tolerant and non‐judgemental. The student will experience the dynamic of being a guest in someone’s home. They will also understand the role of a family carer and the importance they have on a patient’s wellbeing and ability to remain at home. Students will practise how to raise a vulnerable adult alert with social services. Students must be made aware of the lone working policy.
Effective communication, verbal and non‐verbal, will be explained and used. The student will learn effective responses to telephone enquiries, triage and information sharing, and maintain confidentiality especially in families when a patient does not want to share information with loved ones or in a shared office. They will experience many issues regarding language barriers and learn strategies to manage this. They will be involved in constructive feedback to other agencies involved.
The student will experience the need for infection prevention in patients’ homes that may not be hygienically clean. They will need to learn to identify potential risks and discuss them with families, and may need to work in areas that have manual handling problems such as low beds, cramped environments, and poor lighting. The student will learn to recognise problems that could arise if it was necessary to perform resuscitation in the community without complex equipment and often in confined places.
Читать дальше