Table 3Summary of placement and loading protocols (Gallucci et al, 2018).
|
Loading protocol |
| Immediate restoration/loading (Type A) |
Early loading (Type B) |
Conventional loading (Type C) |
| Implant placement protocol |
|
|
|
| Immediate placement (Type 1) |
Type 1A CD |
Type 1B CD |
Type 1C SCV |
| Early placement (Type 2–3) |
Type 2–3A CID |
Type 2–3B CID |
Type 2–3C SCV |
| Late placement (Type 4) |
Type 4A CD |
Type 4B SCV |
Type 4C SCV |
 |
Review article from the 6th ITI Consensus Conference on Implant Placement and Loading Protocols in Partially Edentulous Patientsby Gallucci and coworkers (2018). |
Risk factorsThis term refers to any preexisting condition, treatment option, or material choice that may have an adverse effect on the outcome of treatment. These factors have the potential to influence the final SAC classification of a clinical situation.
This classification assumes that appropriate training, preparation, and care are devoted to the planning and implementation of treatment plans. No classification can adequately address cases or outcomes that deviate significantly from the norm. In addition, it is assumed that clinicians will be practicing within the bounds of their clinical competence and abilities. Thus, within each classification, the following general and specific assumptions are implied:
• Treatment will be provided in an appropriately equipped dental office with an appropriate aseptic technique.
• Adequate clinical and laboratory support is available.
• Patients’ medical conditions are appropriately addressed.
• The surgical procedures are planned and provided following recognized protocols.
• The prosthesis is designed, manufactured, and managed correctly.
 |
ITI Learning Module Surgical Setup for Office-Based Implant Surgeryby Waldemar Daudt Polido. |
2.3 Is the Clinician a Risk Factor?
With the increasing popularity of dental implant treatments with both patients and dental practitioners, the risks associated with the clinician are often overlooked. Derks and coworkers (Derks et al, 2016) described a situation where implant complications from peri-implantitis were significantly correlated with the level of experience of the dentist who was completing the restorative part of the treatment. In this study of real-world treatments, general dentists were 4.3 times more likely to be associated with a peri-implantitis problem than were restorative specialists. While this result may relate to confounding biases in the data set used in this study, which could not be controlled due to the nature of the data, it is still a somewhat disconcerting statistic.
It is also a concern in connection with the incidence of complaints and medicolegal claims relating to implant treatments that are increasing in many jurisdictions. In some regions, professional indemnity insurers are charging additional premiums for particular groups of practitioners who are participating in implant dentistry. These insurance companies do so on the basis of their own actuarial research, which indicates additional risk associated with these treatments in the hands of specific cohorts of practitioners.
2.3.1 Factors impacting the clinician as a risk factor
2.3.1.1 EXPERIENCE
It is a widely held truism in the surgical disciplines in medicine that a surgeon needs to complete between 50 and 100 procedures to be considered competent. The real evidence for this is somewhat less clear. Jerjes and Hopper (2018) described a number of investigations into the relationship between experience and postoperative outcomes in both medical and dental surgical disciplines. Their review found no consistent relationship between these factors. However, it did find evidence that there was often a threshold level of experience below which surgeons could be expected to have greater incidence of problems, indicating that there was a “learning curve” related to most surgical procedures. This threshold value varied between disciplines and studies.
In a systematic review of the relationship between surgeon experience and implant failure rates, Sendyk and others (Sendyk et al, 2017) noted that this relationship did not correlate with the surgeon’s specialty but was significantly related to the number of implants that the surgeon had placed. In an earlier study, Lambert and coworkers (Lambert et al, 1997) found similar outcomes, noting that implant failure rates were two times higher for inexperienced surgeons (ie, who had placed less than 50 implants) compared to those of surgeons who had placed 50 or more implants. They also noted that the first nine implants placed by a surgeon under training where at the greatest risk of failure. These findings could be reasonably accepted as showing a relationship between experience and outcomes in implant treatments.
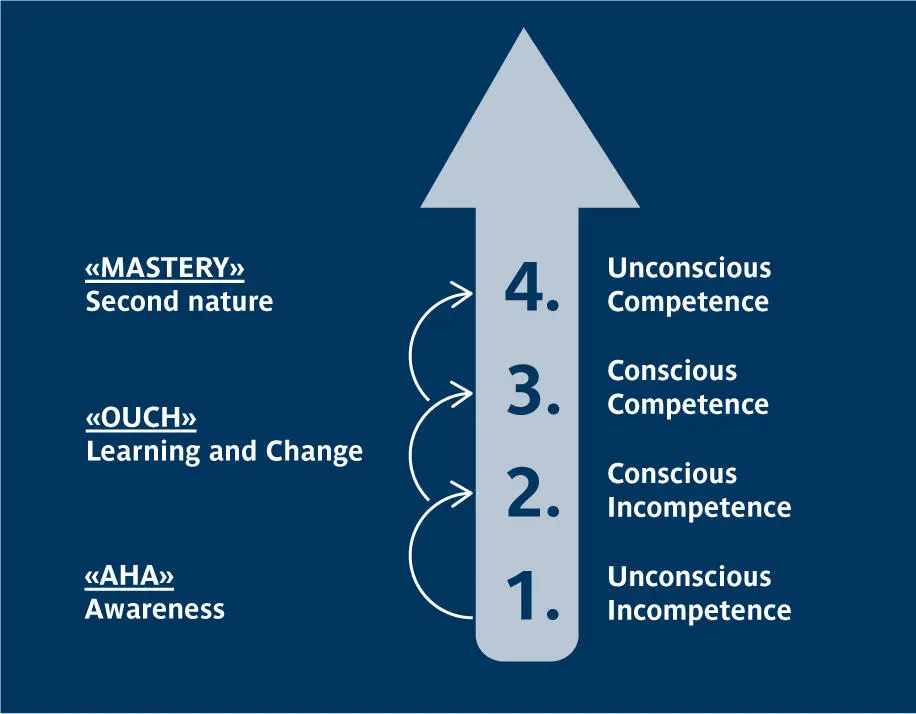
Training is another area of consideration. The Conscious Competence Learning Model (Curtiss & Warren, 1973) is an accepted description of how people learn new skills. In this model ( Figure 1), four stages of learning are described:
1. Unconsciously incompetent:Here
2. Unconsciously incompetent:Here the person knows little about what they are doing. They cannot comprehend the potential difficulties involved in a process, and they often feel that they are performing the task to a high standard. They do not know what they do not know, and this is a major impediment to learning.
3. Consciously incompetentThe learner comprehends that they fall short of ideal performance and understands their knowledge deficit. Making mistakes at this stage is often a key part of learning.
4. Consciously competent:The person at this level of learning can perform the task to an acceptable standard, but this requires concentration and attention to detail.
5. Unconsciously competentThe individual at this level has had so much practice that they can perform this task without conscious effort. These people can be good teachers in the technique but can also make the task appear “too easy” to casual observers.
 |
Congress lecture Surgical Treatment of Esthetic Disastersby Waldemar Daudt Polido. |
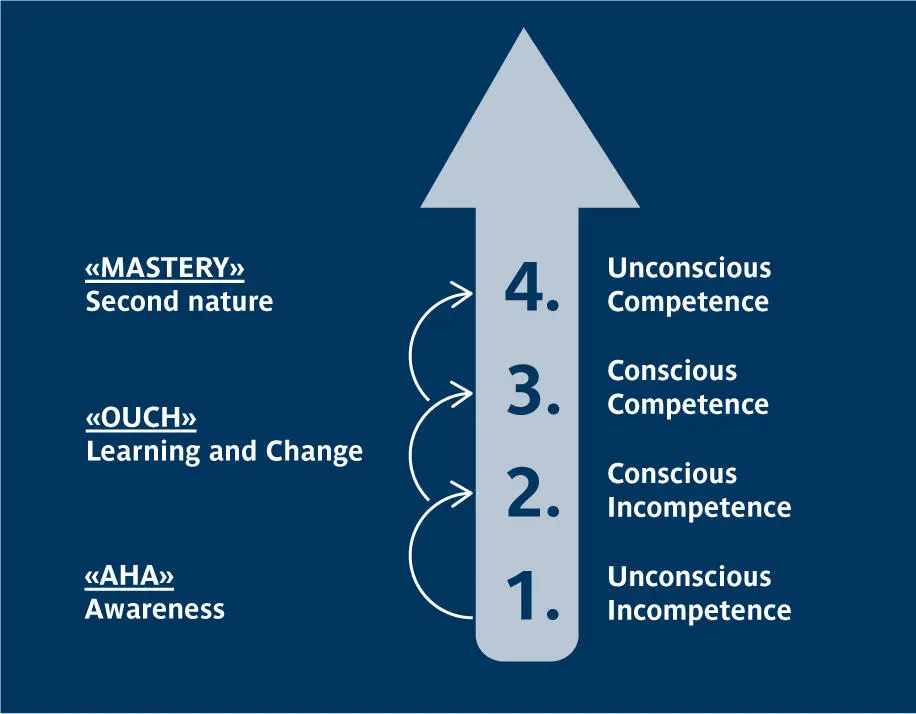
Fig 1.The Conscious Competence Learning Model.
Training in implant dentistry needs to address each of these learner levels. For the unconsciously incompetent , clinical training must address their knowledge deficit and stress best-practice approaches to treatment provision. Simulations of treatment provision, and mentoring by more experienced clinicians, can assist the consciously incompetent practitioner to pass through this level without endangering patients under their care. Mentoring will also benefit the consciously competent clinician by supporting their incremental development of skills. Finally, for the unconsciously competent clinician, training must support their focus on practicing in a reflective and consistent manner. The unconsciously competent clinician is at some risk of complacency and overconfidence and must make a conscious effort to remain focused on current best practices and the evolution of techniques in implant dentistry. They are also something of a risk to less knowledgeable and less skillful colleagues who might observe them providing patient care and conclude that these treatments are more straightforward than they really are.
Читать дальше