Technique
Fetal blood sampling
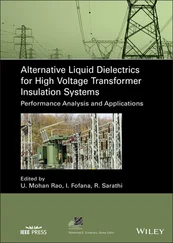
Fetal blood sampling can be done in the outpatient setting and requires minimal preparation, especially in a previable pregnancy. As shown in Figure 9.1, a sterile field, a 22 gauge needle, heparinized syringes, and ultrasound guidance are typically all that is required for diagnostic cordocentesis. Color Doppler can help to identify umbilical cord vessels at their insertion into the placenta. Accessing the fetal umbilical vein at its placental insertion is preferred; this is the most stable point and the least likely to allow the needle to dislodge. When this approach is technically difficult, the second choice should be the intrahepatic part of the umbilical vein. Alternatively, a free loop of cord can be used, which will prove more challenging and is also associated with a higher procedural loss rate. Placement into the lumen of the umbilical vein is immediately confirmed by observing either backflow of blood or turbulent flow in the cord when a saline flush is utilized and further documented by assessing putative fetal versus known maternal red blood cell (RBC) mean corpuscular volume (MCV) values. Fetal samples are drawn into heparinized syringes and sent for testing. Some streaming is expected from the cord once the needle is withdrawn.

Figure 9.1 A typical procedure tray set‐up for cordocentesis, with 22 gauge spinal needles of varying lengths, 10 cc and 20 cc syringes to collect amniotic fluid samples, if needed, and heparinized syringes to collect a fetal blood sample. Sterile gel and ultrasound transducer probe cover are also shown in the image.
Though diagnostic cordocentesis may be done in the outpatient setting, most fetal transfusions are performed in or near an operating room, particularly if a fetus is viable and a failed procedure might prompt delivery. The patient would be evaluated preoperatively by the obstetric anesthesia providers, as well as the NICU team, depending on gestational age. Anesthesia options for the mother range from regional block to sedation and local anesthetic. The NICU team will want to discuss with the patient the neonatal management of anemia in a newborn. Steroids for fetal lung maturation should also be considered preprocedurally depending on gestational age, though they are not used routinely in some major centers.
It is a critical part of preparation for fetal blood transfusion to communicate with your blood bank/transfusion services, so they are aware of the request for a specially prepared unit. These units require a maternal “type and cross” for ½ to 1 unit of O negative, washed, leukoreduced, irradiated, cytomegalovirus (CMV)‐negative packed red blood cells (PRBC), with a hematocrit (Hct) of at least 75%. If there is suspicion of fetal thrombocytopenia (for instance, in cases of parvovirus) you may also need to order an aliquot of platelets for fetal transfusion.
Preoperative testing of the mother should include complete blood count (CBC). You will need the maternal MCV to compare to the fetal MCV to ensure you have sampled the fetal blood, since fetal RBCs are larger than maternal RBCs. Labs to be drawn at the time of fetal blood sampling (fetal Hgb/Hct, MCV, blood type/Rh, and platelets) should be preordered in the medical record so results are processed in the most expeditious manner, since total transfusion volume will depend on those initial results.
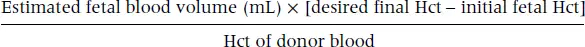
In anticipation of the fetal transfusion, you will want to make all calculations for transfusion volume ahead of time based on most recent estimated fetal weight. The original formula described by Rodeck and colleagues in 1984 is:
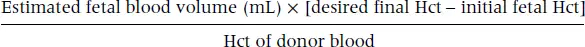
Estimated fetal blood volume varies with gestational age but a good rule of thumb is 100 mL per kg. A helpful webpage for quicker calculations is www.perinatology.com/protocols/rhc.htm. As an example, assuming a Hct of 75% for the transfusion unit, and a 1600 g fetus with a starting Hct of 20% and an end Hct goal of 35%, you will need to transfuse 35 mL of blood. You will want to have worked out the possibilities for several starting hematocrits and chart them on a table so you don’t have to do math in your head while holding a needle inside the cord of a fetus!
Generally, you might suspect a low Hct hematocrit based on sonographic findings (hydrops, for example) or other signs of fetal compromise. The goal at the first transfusion in such cases is to reach a closing Hct of 30–35%. Overtransfusion might put the fetus at risk of heart failure. The compromised fetus might need follow‐up transfusion within a week of the initial one with a goal of closing Hct 40–45%. Thereafter transfusions are scheduled depending on the diagnosis and severity of disease.
The preferred route of fetal transfusion is intravascular, via the umbilical vein. On occasion, related to fetal position or posterior placenta, it might be technically impossible to access the umbilical vein at the cord, making it necessary to access the intrahepatic portion of the umbilical vein. In the very premature or hydropic fetus, intraperitoneal transfusion may also be performed by injecting donor blood directly into the fetal peritoneal cavity, where blood would be absorbed through lymphatics. Absorption of the transfused blood may not be optimal in these situations.
A typical set‐up for fetal transfusion is shown in Figure 9.2. Your OR table should be readied with prepared syringes with paralytics and sedative for the fetus. The appropriate doses are based on estimated fetal weight: the usual dose for vecuronium is 0.1 mg/kg, and typical dose for fentanyl is 10 μg/kg. Though these may not be needed, especially in the case of an anterior placenta with easy access to the placental cord insertion site, use of paralytics has been associated with lower rates of procedure‐related fetal loss. You will also need heparinized syringes to draw fetal blood samples for testing. These can be prepared by drawing heparin into 1 cc syringes. Caution is required when using heparinized syringes: you will need to waste the heparin from each syringe immediately prior to drawing a fetal sample. IV tubing for your transfusion circuit, sterile probe and ultrasound covers, and spinal needles should be placed on the procedure table as well.
Once your OR table set‐up is complete, follow sterile technique to prep and drape the maternal abdomen. Most large studies conclude that routine antibiotic prophylaxis is not necessary. Your ultrasound machine should ideally have a clear plastic sterile cover over the control panel, so you can continue to manipulate your image settings even after you are gowned up in sterile fashion. A sterile probe cover is part of the usual prep of equipment as well.
Prior to your initial attempt at sampling of the cord, prime the transfusion circuit. The specifics of a transfusion circuit may vary, but typically consist of simple IV tubing connecting the donor blood unit to the lateral port of a three‐way stopcock, and another piece of simple IV tubing extending from the other lateral port, to connect to the spinal needle that accesses the fetal intravascular space. This fetal side of the circuit remains closed while a 10 or 20 cc syringe attached to the middle port is used to draw blood into it to use as a reservoir. Make sure that you and your assistant are familiar with the on/off twisting of the three‐way stopcock and how it changes direction of flow prior to starting the procedure.
Читать дальше