The interest in health and well‐being over the recent years has gathered momentum significantly with a growing body of evidence that has demonstrated a link with working conditions, support offered by managers and staff engagement with patient outcomes.
Wellness is so much more than being simply free from illness. ‘Health’, according to the World Health Organization (2019) is ‘a state of complete physical, mental and social well‐being and not merely the absence of disease or infirmity’.
The WHO definition explicitly links health with well‐being, seeing health as a positive aspiration; health therefore is a means to living well, highlighting the link between health and participation in society, as a human right that requires physical and social resources to achieve and maintain. ‘Well‐being’ refers to a positive rather than neutral state.
Resilience is the capacity to bounce back from adversity; sometimes it is also known as emotional resilience. Protective factors increase resilience, and risk factors increase vulnerability. Resilient individuals, families and communities are more able to deal with difficulties and adversities than those with less resilience (University College London 2014). Resilience is associated with the ability to face adverse situations whilst remaining focused, continuing to be optimistic for the future. See also Chapter 8of this text.
The Nursing Associate needs to consider those factors that impact upon their own health; this is sometimes known as self‐care. There are several resources available that can help support the Nursing Associate and other nursing staff to take ownership of their own health (physical or/and mental), encouraging them to take the time to apply the same level of care to their own well‐being just as they would do for the people they care for and offer support to. The focus needs to on body, mind, heart, work, career, spirit and balance. Figure 6.1provides an overview of some of the components of healthy living that may lead to enhanced well‐being.
The Royal College of Nursing have produced a ‘Healthy You Assessment Worksheet’. The self‐assessment offers an overview of effective strategies to maintain a healthy you. The lists are not definitive, only suggestions. When completing the assessment, choose one item from each area that you will actively work on to improve.
Chapter 7 The principles of research and evidence‐based practice
At the point of registration, the Nursing Associate will be able to:describe the principles of research and how research findings are used to inform evidence‐based practice (EBP).
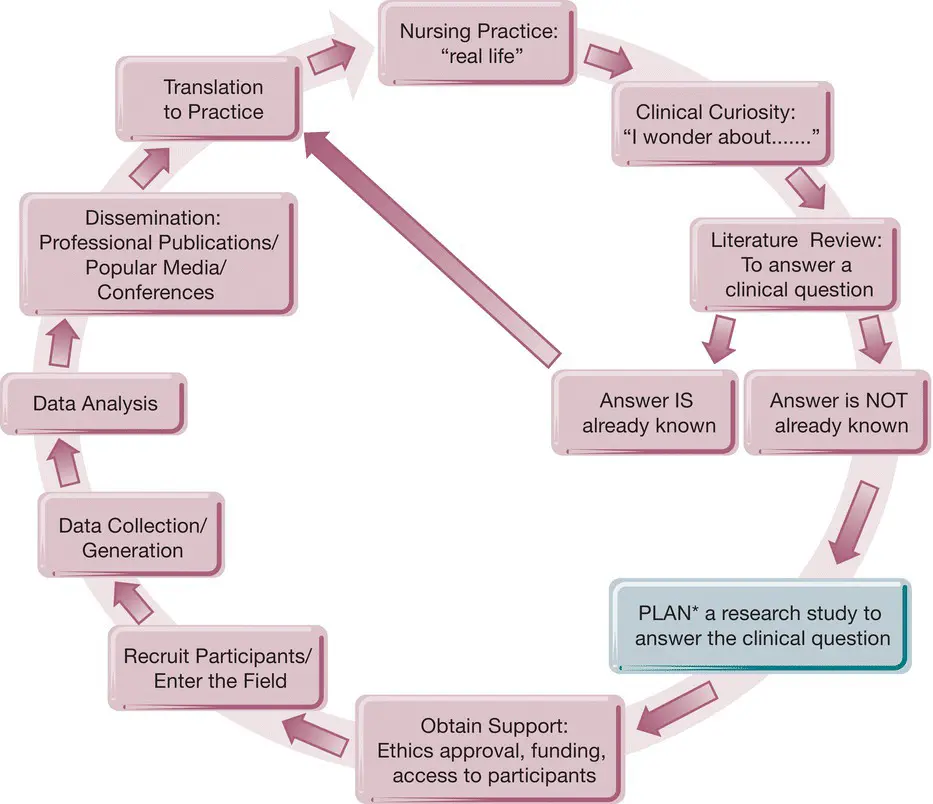
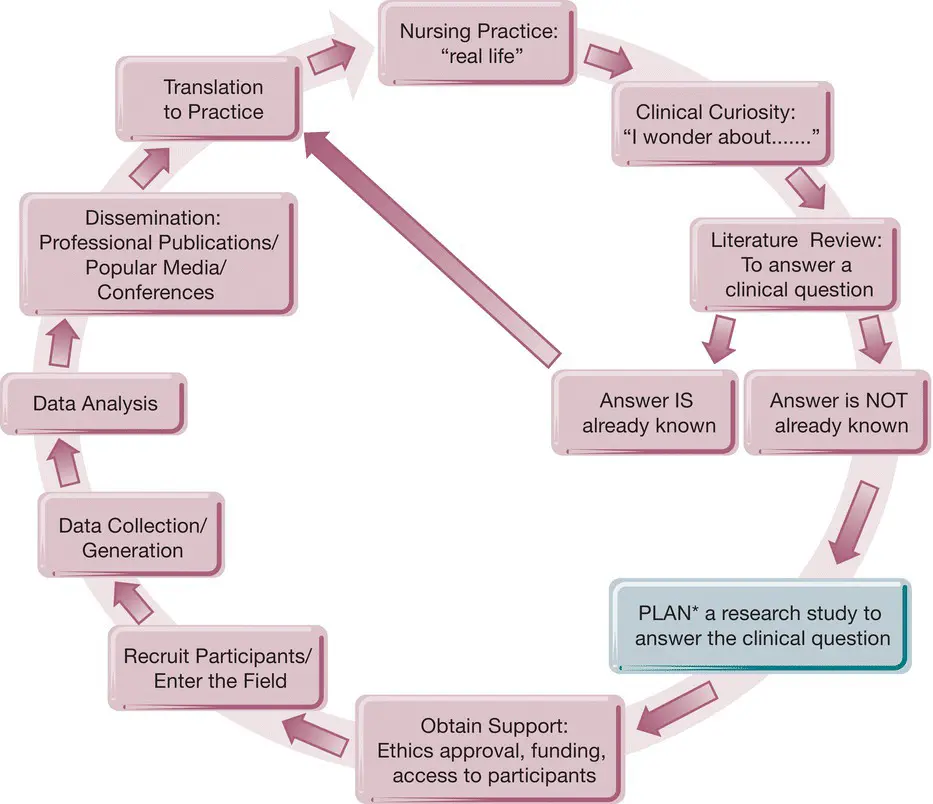
Figure 7.1 The stages of the nursing research journey.
Source: Glasper and Rees (2017).
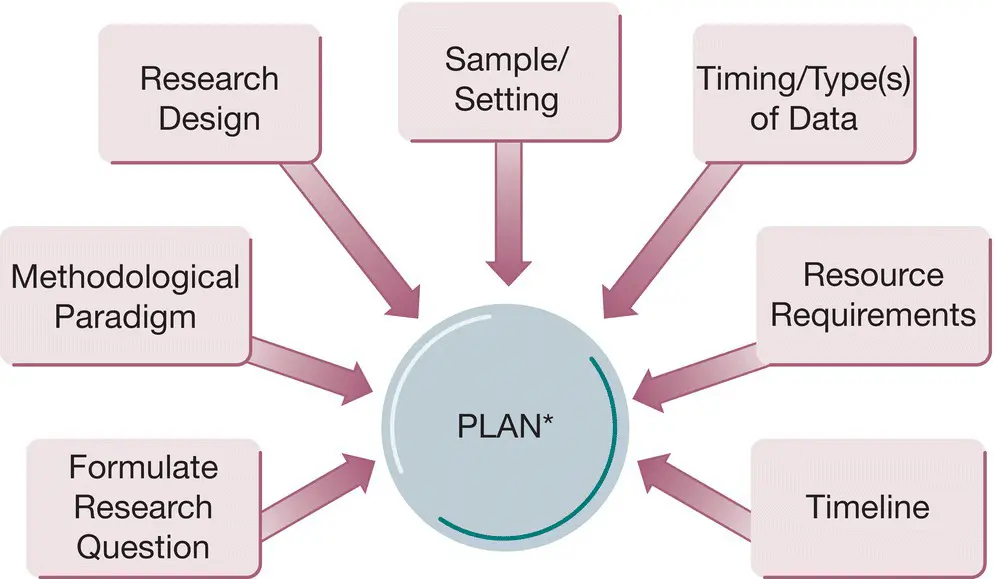
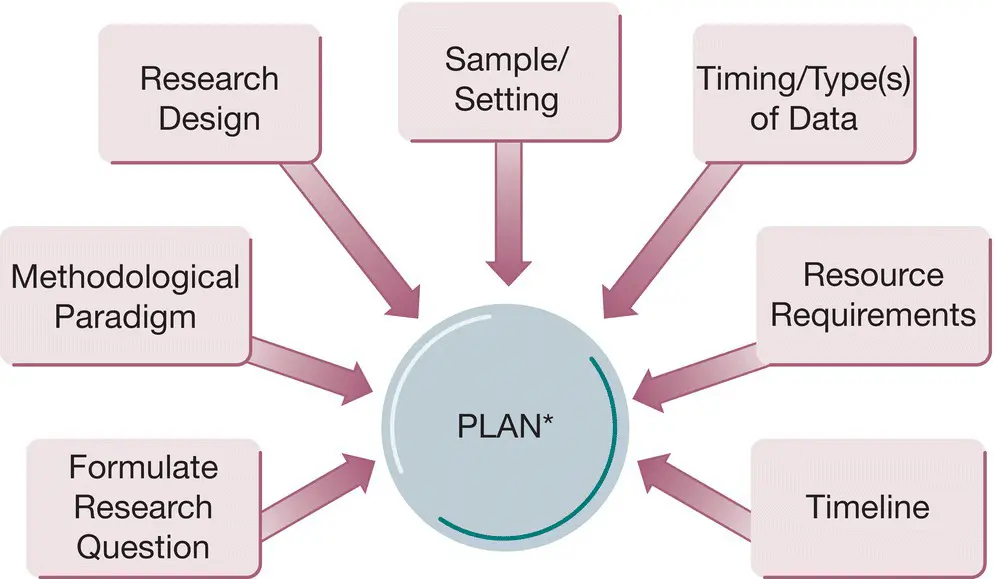
Figure 7.2 Planning: the research process.
Source: Glasper and Rees (2017).
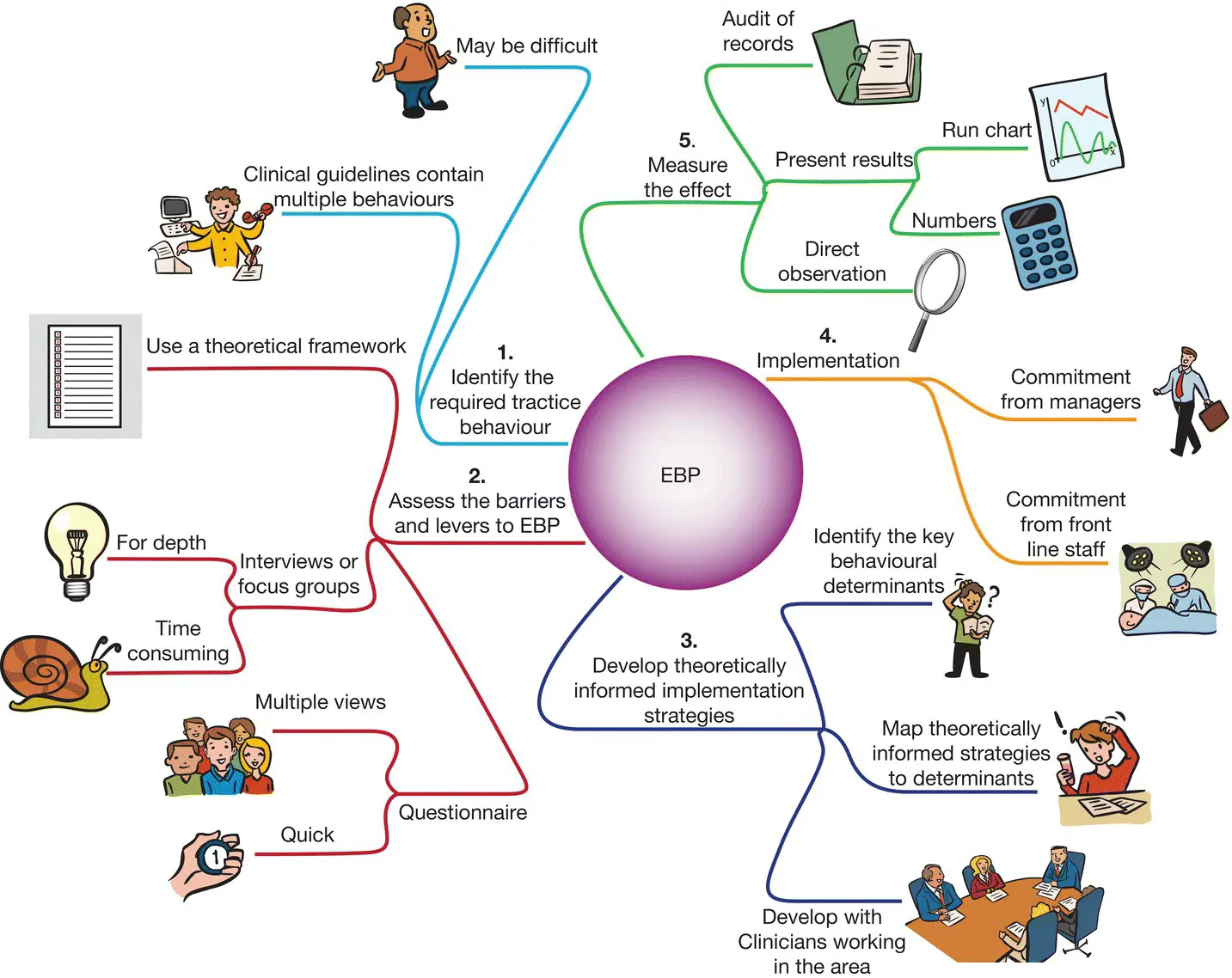
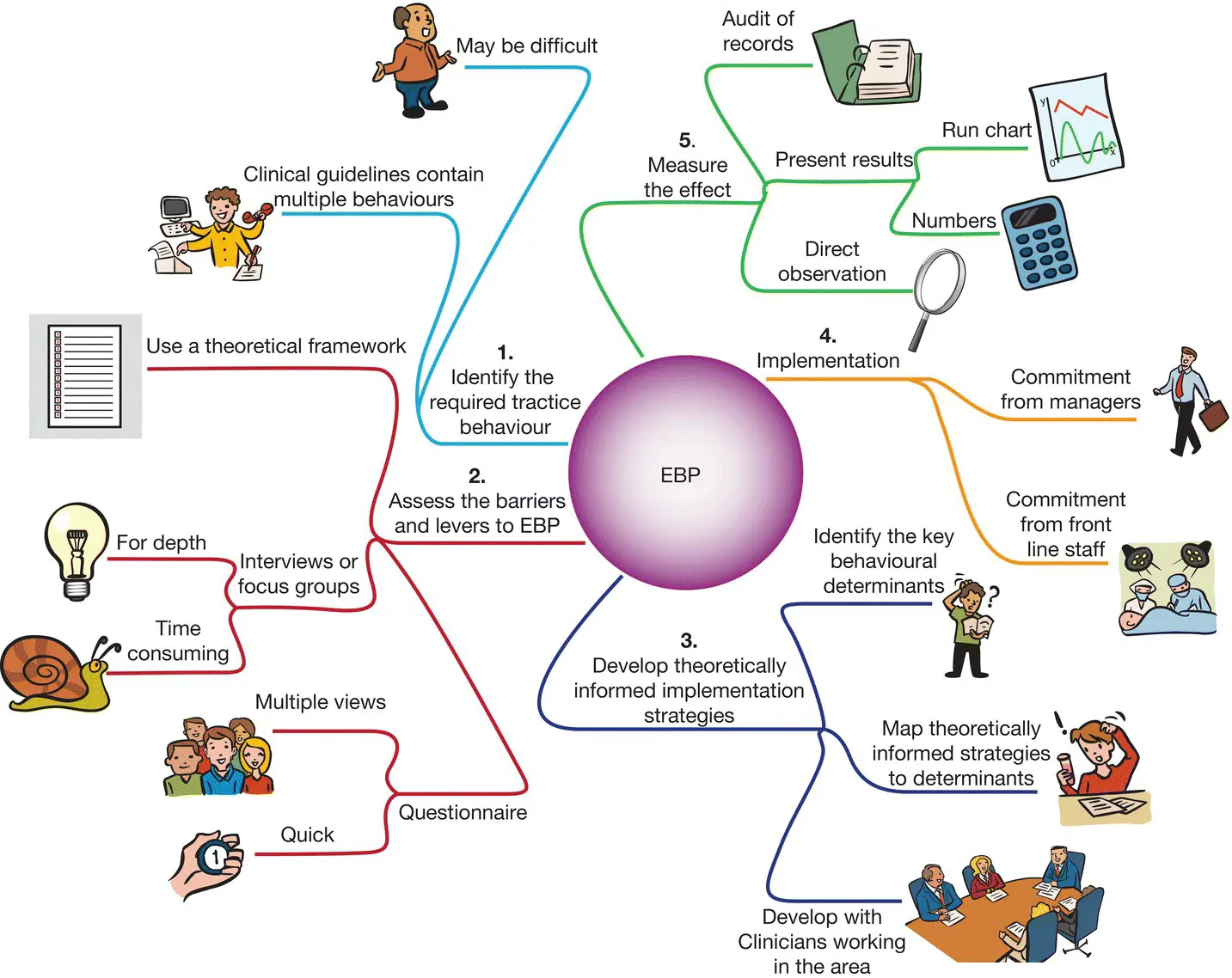
Figure 7.3 Implementation of evidence‐based practice (EBP).
Source: Glasper and Rees (2017).
It is not possible to address all aspects of research and evidence‐based practice (EBP) in this chapter. Glasper and Rees (2017) have edited an excellent text: Nursing and Healthcare Research At A Glance .
The provision of high‐quality care is supported by evidence. Gaining knowledge through research and evidence‐based practice (EBP) and developing strategies for implementation are key skills for Nursing Associates regardless of the setting.
The purpose of undertaking research is to generate new knowledge or to validate existing knowledge based on a theory. Research studies will involve systematic, scientific inquiry aimed at answering specific research questions or to test hypotheses using analytical, rigorous methods. Although research is about investigation, exploration and discovery, it also requires insight and understanding of the philosophy of science. For research results to be considered reliable and valid, those undertaking the research use the scientific method in orderly, sequential steps. The stages of the nursing research journey can be found in Figure 7.1. The planning stage is depicted in Figure 7.2.
All research is different, and the following principles are common to all good pieces of research involving those using health and social care services, their families and carers and staff:
A clear statement of research aims, defining the research question.
Accessible information for participants, explaining what the research is about and what it will involve; consent is obtained in writing on a consent form prior to commencement of research.
The methodology is appropriate to the research question. Some research use a combination of methodologies, complementing one another.
The research should be carried out in an unbiased fashion. As far as possible the researcher should not influence the results of the research in any way.
From the outset, the research should have appropriate and sufficient resources allocated to it.
Those conducting the research should be trained in research and research methods.
Those involved in designing, conducting, analysing and supervising the research should have a full understanding of the subject area.
It may help if the researcher has experience of working in the area.
If applicable, information generated from the research will inform the policy‐making process, and it should be disseminated.
All research must be ethical and not harmful in any way to participants.
EBP, unlike research, is not concerned with developing new knowledge or validating existing knowledge. EBP is about translating the evidence and then applying this to clinical decision‐making situations (see Figure 7.3). One of the overall aims of EBP is to implement the best evidence that is available to make patient‐care decisions. Most of the best available evidence is derived from research. EBP, however, goes beyond research use and it also includes clinical expertise as well as patient preferences and values. EBP acknowledges that there are times when the best evidence is that of opinion leaders and experts (and these may include patients), despite the absence of definitive knowledge from research results. Although research is concerned about the development of new knowledge, EBP involves innovation in terms of finding and translating the best evidence into clinical practice.
A number of critical steps are associated with EBP.
The EBP process comprises seven critical steps:
1 Promote a body of inquiry (engender curiosity).
2 Ask a significant clinical question.
3 Collect the most relevant and the best evidence (there are hierarchies of evidence).
4 Critically appraise the evidence (use a systematic approach).
5 Integrate the evidence with clinical expertise, patient preferences and values in making a practice decision or change.
6 Evaluate the practice decision or change.
7 Disseminate EBP results.
Читать дальше